ORIGINAL RESEARCH ARTICLE
Clinical effects of homodigital dorsal branch of the proper digital artery flap on repairing soft tissue defects of fingers
Yong Zhang, Jupu Zhou and Jianzhong Qin
Department of Hand and Foot Surgery, The Second Affiliated Hospital of Soochow University, Suzhou, Jiangsu, China
Homodigital dorsal branch of proper digital artery flaps (HDBPDAF) have been proved to be an excellent alternative for repairing distal soft tissue defects of fingertip. This study was to evaluate the clinical effects of HDBPDAF on repairing various soft tissue defects of fingers, including thumb and multi-fingers defects. A retrospective study was conducted in 40 patients with 44 finger defects treated with HDBPDAF from August of 2014 to December of 2021. The defects were located on fingertip and finger pulp (n = 28), finger pulp (n = 10), and dorsum of fingers (n = 6) with bone, tendon or nerve exposed. The average size of the flaps was 1.9 × 3.9 cm. Semmes Weinstein monofilament (SWM) test, Static two-point discrimination (2-PD), Total active motion (TAM) scores, the mean Disabilities of the Arm, Shoulder, and Hand (DASH) score were evaluated through long-term follow-up. Forty-two flaps survived completely and uneventfully. Partial flap necrosis was observed in two flaps because of the absence of dorsal branch of proper digital artery. No visible scar contracture and joint limitation were noticed. The mean SWM score of flaps was 4.11 ± 0.4 g. The average 2-PD of the flaps was 8.9 ± 0.9 mm. The mean TAM of injured fingers was 268.7 ± 5.2° (contralateral side: 283.2 ± 6.4°, p < 0.05). The mean DASH score value was 29.7 ± 7.9. The HDBPDAF was an optimal and reliable alternative to repair various distal soft tissue defects of fingers, despite a lower absent rate of dorsal branch.
KEYWORDS: Proper digital artery; dorsal branch; surgical flaps; soft tissue defect
Citation: Journal of Plastic Surgery and Hand Surgery 2023; 58: 18–23. DOI: https://doi.org/10.2340/jphs.v58.11967.
Copyright: © 2023 The Author(s). Published by MJS Publishing on behalf of Acta Chirurgica Scandinavica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Received: 1 April 2023; Accepted: 3 May 2023. Published: 14 June 2023.
CONTACT Jianzhong Qin, qinjianzhong2008@163.com Department of Hand and Foot Surgery, The Second Affiliated Hospital of Soochow University, Suzhou, Jiangsu 215004, China
Competing interests and funding: The authors declare that they have no conflicts of interest. The authors have no proprietary, financial, professional, or other personal interests of any nature or kind in any product, service, or company that could be construed as influencing the position presented in, or the review of, the manuscript.
This work was supported by the Science and Technology and Planning Program of Suzhou City under Grant [No. SYS2020127, No. SKY2022143].
Introduction
Over the past years, many flaps, such as cross-finger flap [1], thenar flap [2], digital artery flap [3], and dorsal metacarpal flap [4] have been uninterruptedly introduced to cover various soft tissue defects of long fingers successfully. However, the versatile optimal flap for soft tissue reconstruction of thumb and multi-fingers defects with bone, tendon or nerve exposed has not been clearly defined in the literature.
Identifying the versatile optimal alternative has become a must to avoid the disadvantages including second surgery, sacrifice of one proper digital artery (PDA), incapacity of simultaneous reconstruction of multi-fingers defects. The flap pedicled on the dorsal branch (DB) of PDA has been reported in a few literatures and has been proved to be a promising alternative to solve those problems excellently [5–7]. Here, we report the use of homodigital DB of PDA flaps (HDBPDAF) on repairing soft tissue defects of fingers, including thumb and multi-fingers defects and evaluate the clinical effects by presenting functional and aesthetic outcomes. The purpose of this study was to describe outcomes of reconstruction soft tissue defects of fingers with HDBPDAF, introduce our experiences and summarize the indications of the HDBPDAF.
Materials and Methods
Patients
From August of 2014 to December of 2021, a total of 40 patients (31 males and nine females) with 44 finger defects, aged 20 to 56 years (mean age: 45 ± 13.6 years), were treated with DB digital flaps. The causes of injuries included machine crushing (n = 23), electrical sawing injury (n = 15) and chronic infection (n = 2). Twenty-eight digital defects were located on the fingertip and pulp of injured fingers, 10 on the finger pulp, and six on the dorsum with bone, tendon or nerve exposed. Among these, four patients had multiple fingers injured at the same time. A total of 26 fingers were on the left hand and 18 on the right hand. There were 10 thumbs, 14 index fingers, 10 middle fingers, eight ring fingers and two little fingers injuries (Table 1). All patients gave written informed consent. The study was approved by the ethical review committee of the Second Affiliated Hospital of Soochow University. The study adhered to declaration of Helsinki guidelines.
Surgical technique
Patients were administered under brachial plexus anesthesia and an inflatable tourniquet was applied to the upper arm to occlude blood flow at a pressure of 30 kPa. After thorough debridement, the flap was designed on the dorsal aspect of middle or proximal phalanx of injured finger according to the pattern and area of the defect. The pivot point of the flap was located around the midportion of midlateral line of middle or proximal phalanx, where one constant DB originating from the PDA could be identified predictably (Figure 1). With the aid of operating loupes, the flap was elevated carefully, avoiding damage of the vascular networks between DBs of PDAs and making sure that the skin was not separated from subcutaneous tissues. The paratenon should be left in situ to ensure the take of the skin graft. To avoid kinking and reduce tension on the vascular pedicle, a 0.5 cm wide subcutaneous fascial tissue incorporating DB of PDA and tiny perivascular venules, should be dissected and thoroughly released to the originating point of DB from PDA, thus the length of the pedicle could be significantly increased and the torsion stress of the pedicle could be dispersed after the rotation of the flap. Tourniquet was loosed after full flap elevation to observe the blood supply of the flap. An opened tunnel was prepared for the transfer of the flap, which was then sutured to the defect loosely. Whereas for those who had a larger defect, our extended flaps based on the DB of PDA at the middle or proximal phalanx was raised by extending the distal end of the flap to the middle level of proximal phalanx or the base of the proximal phalanx and the length of injured fingers was maintained to the most extent successfully. Similarly, large defect of fingertip and pulp of the thumb was also resurfaced by extending the flap to the middle third of the first metacarpal. The proximal donor site was sutured directly or covered with a full-thickness skin graft according to the size of the donor site. The operation time for one injured finger was within 1 h in all cases.
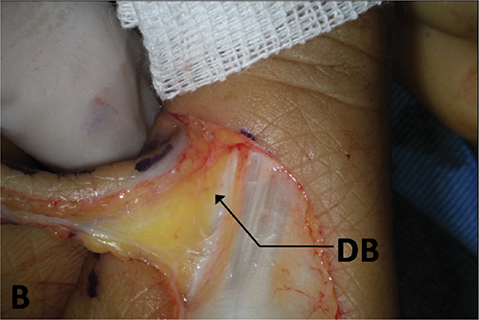
Figure 1. Intraoperative view. The DB of the ulnar PDA was visible at the base of the flap.
Postoperative management
Patients were instructed to stop smoking for 2 weeks after surgery. The fingers were kept warm by a medical electric baking lamp. Blood supply of each flap was monitored hourly for 7 days. The partial suture was removed when severe swelling occurred. Antibiotic was used to prevent postoperative infections and papaverine was used to prevent vasospasm for 5 days after surgery.
Measurement of sensory recovery
The sensibility of the flaps was evaluated using the Semmes Weinstein monofilament (SWM) test with a five-piece hand kit (normal, ≤2.83; diminished light touch, 2.84–3.61; diminished protective sensation, 3.62–4.31; loss of protective sensation, 4.32–4.56; and anesthetic, ≥6.10) [8]. The static two-point discrimination (2-PD) test was performed to quantitatively evaluate sensory recovery using a caliper with two small needles. Patients were instructed to close their eyes and touch the needles on the caliper against the skin at different distances from each other. The test determines the minimal distance at which the patient cannot distinguish two points in contact with the skin. The patient must be comfortable, and the examiner must avoid pushing against the calipers with his/her fingers, thereby artificially increasing the pressure. The higher the pressure, the wider the area of skin that was deformed and stimulated. One or two points were touched in a random sequence along a longitudinal axis in the center of the fingertip. The normal distance was 3–5 mm. The closer the defected finger to the normal range, the better the recovery of the sense [9].
Measurement of functional recovery
The range of motion (ROM) of the injured fingers was performed to evaluate functional recovery and was assessed using the total active motion (TAM) scoring system of the American Society for Surgery of the Hand. TAM = active flexion [metacarpophalangeal (MP) + proximal interphalangeal (PIP) + distal interphalangeal (DIP) − extension deficit (MP + PIP + DIP). The parameters were compared with the contralateral side (100% of normal as excellent, 75–99% as good, 50–74% as fair and < 50% as poor) [10].
To quantify postoperative physical function and symptoms, all patients were evaluated using the Disabilities of the Arm, Shoulder, and Hand (DASH) score. The main part of the DASH is a 30-item disability/symptom scale concerning the patient’s health status during the preceding week. The items ask about the degree of difficulty in performing different physical activities because of the arm, shoulder, or hand problem (21 items), the severity of each of the symptoms of pain, activity-related pain, tingling, weakness and stiffness (5 items), as well as the problem’s impact on social activities, work, sleep, and self-image (4 items). Each item has five response options. The scores for all items are then used to calculate a scale score ranging from 0 (no disability) to 100 (most severe disability) [11].
Results
The finger defects size ranged from 1.7 × 1.8 cm to 2.3 × 4.7 cm. The average size of the finger defects was 1.6 × 3.6 cm. The flaps size ranged from 2.0 × 2.0 cm to 2.5 × 5.0 cm. The average size of the flaps was 1.9 × 3.9 cm. Fingertip and pulp defect of the thumb was repaired in 10 cases. Multiple finger defects were covered simultaneously in four cases. Forty-two flaps survived completely and uneventfully, whereas partial flap loss occurred in the remaining two case because of the absence of DB of PDA. The mean follow-up period was 22.8 ± 5.3 months, ranged from 13 to 28 months. Visible scar contracture in flap donor sites and joint motion limitation of injured fingers were not observed in our patients even if linear scar was observed on the first metacarpophalangeal joint in one case. Good aesthetic and functional outcomes were obtained in our patients. The mean SWM score of the flaps was 4.11 ± 0.4 g (range: 3.59–4.61 g). The average 2-PD of the flaps was 8.9 ± 0.9 mm, ranged from 7 to 11 mm. The mean TAM for the injured fingers was 268.7 ± 5.2° (range: 202–285°), which was over 95% of the contralateral side (283.2 ± 6.4°, p < 0.05), with six fingers scored as excellent and 38 fingers scored as good grade. The mean DASH score value was 29.7 ± 7.9, ranged from 0 to 35 (Table 1).
Typical case
One case of thumb defect and one of two finger defects were presented, respectively.
Case 1
A 42-year-old female had her left thumb crushed seriously in a machine. The defect of fingertip and pulp of her thumb was identified with phalanx exposed. The extended and oversized area of the HDBPDAF was about 2.5 × 5.0 cm. The distal end of the flap approached the middle third of the first metacarpal. In a two-year postoperative period, the follow-up did not reveal any morbidity, such as claw nail deformity and joint motion limitation, related to the flap (Figures 1–3). The mean SWM score of the flap was 4.29 g. The 2-PD of her flap was 7.5 mm and her DASH score was 19.
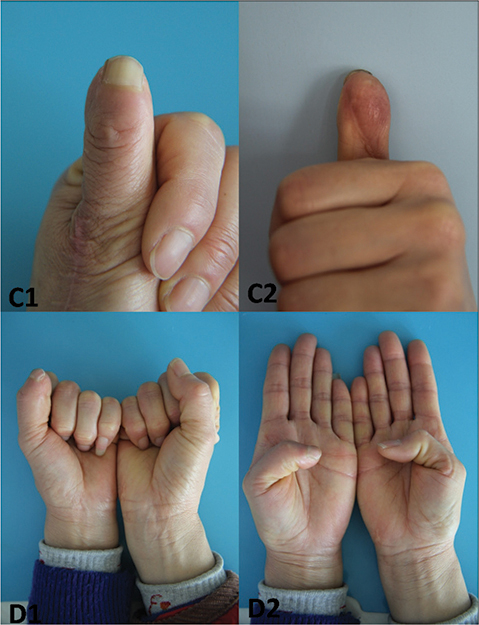
Figure 2. Preoperative view. The left thumb was crushed seriously in a machine. The size of the flap was 2.5 × 5.0 cm.
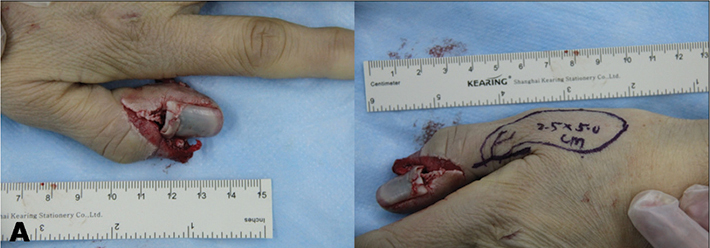
Figure 3. Postoperative view 24 months after surgery. Good aesthetic and functional outcomes were obtained.
Case 2
A 38-year-old male sustained a severe crushing injury to his right middle through little finger, with extensive pulp loss of middle and ring finger with bone and tendon exposed. His little finger was amputated and the amputation stump healed uneventfully. The defects of middle and ring finger were reconstructed with two HDBPDAFs of the same size (2.0 × 4.0 cm) pedicled on the DB of PDA at the proximal phalanx of injured finger, respectively (Figures 4–6). Satisfactory aesthetic and functional outcomes were obtained at follow-up. The mean SWM score of the flaps was 4.31 g and 4.36 g, respectively. The 2-PD of the flaps was 8.8 mm and 8.5 mm, respectively, and his DASH score was 36.

Figure 4. Preoperative view. The patient sustained a severe crushing injury to his right middle through little finger, with extensive pulp loss of middle and ring finger.
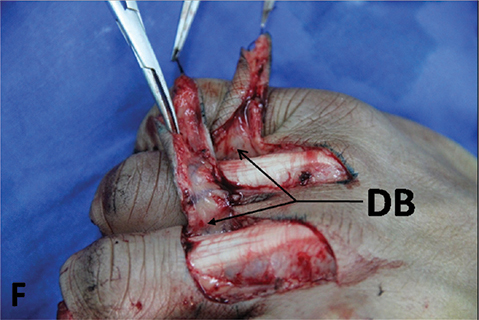
Figure 5. Intraoperative view. The two flaps were harvested from the dorsum of proximal phalanx of middle and ring finger, respectively. The DB of PDA at the proximal phalanx of injured finger was identified.
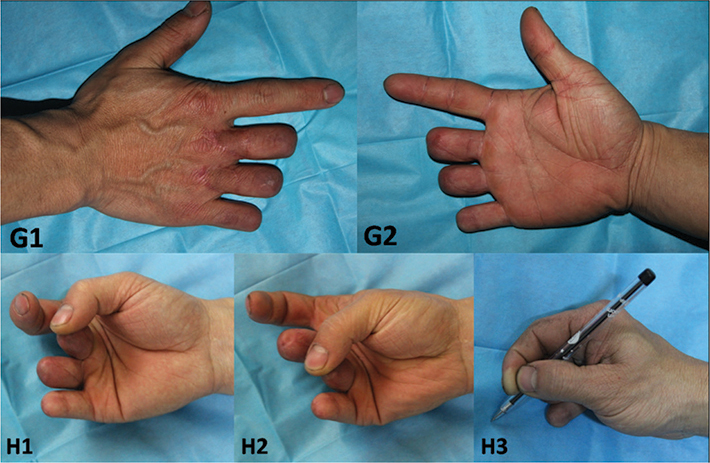
Figure 6. Postoperative view 18 months after surgery. Satisfactory aesthetic and functional outcomes were obtained.
Discussion
It has been identified that, for long fingers, four constant DBs of PDA (i.e. two pairs of proximal and distal DBs located at the middle and distal third of the proximal phalanx, and at the proximal and middle third of the middle phalanx, respectively) supply the dorsal skin of proximal and middle phalanx [11,12]. Among them, two DBs, located at the middle third of the proximal and middle phalanx, respectively, were commonly used as the pedicle of DB of PDA flap [6,7,13,14]. Simultaneous reconstruction of multiple separate finger defects was successfully performed and minimal morbidity was ultimately observed by the HDBPDAFs.
To our knowledge, the dorsal arteries of the thumb have rarely been the subject of an in-depth anatomic study. Few literatures have been reported about the vascular blood supply on the dorsal aspect of the thumb. The dorsal vascular system of the thumb was supplied by two constant arteries, the radial and ulnar collateral dorsal artery. At the level of the middle third of the proximal phalanx of the thumb, the collateral dorsal artery anastomosed with the DB of the volar digital artery and dorsally with the collateral dorsal artery opposite [15–17]. Taking into account these anatomical characteristics of the thumb, it has been proved possible to raise an extended and oversized flap pedicled on the DB of the volar digital artery. Ten extended HDBPDAFs pedicled on the DB of the volar ulnar PDA have been employed for repair of fingertip and pulp defects of the thumb in our patients.
It was reported that innervated flap with a sensory nerve to resurfacing the volar aspect of the tip or finger pulp would better restore sensation of the injured finger [18]. However, whether an innervated flap is superior to a non-innervated flap still remains controversial. The extent of sensory recovery of the non-insensate flap depends on the size of the flap and the extent of peripheral nerve regeneration around the flap [19]. Although previous studies had demonstrated that flaps larger than 1.0 × 1.0 cm had a reduced capacity for recovery of sensation without nerve coaptation, many studies obtained a protective 2-PD at a satisfactory level by using non-innervated flaps [20,21]. Although the innervated flap provided fairly rapid and satisfactory sensory recovery of the repair area, it caused noticeable sensory loss of the donor site on the dorsal side of the proximal or middle phalanges. In addition, it is sometimes difficult to dissect small nerves and requires a longer operation time and microsurgical expertise. For neurorrhaphy, carrying nerves may lead to flap pedicle torsion or excessive tension [18]. Therefore, we did not actively use innervated flap surgery technology. In the retrospective study by Chen et al., the average 2-PD of 12 non-innervated digital flaps was 7.5 mm at 28 months postoperatively [22]. This outcome was 1.4 mm better than our non-innervated flaps, possibly related to the longer follow-up period, indicating that sensory function can improve over time.
It may be necessary to shorten the phalanx when resurfacing the defect of fingertip with flaps [1,23,24]. Practically, conventional flaps used to cover the exposed bone were not large enough to preserve the length of phalanx to the most extent. The purpose of our extended flaps for fingertip reconstruction was to maintain the length of injured fingers as much as possible.
With the angiography in a dog model raised various flaps to predict the safe survival lengths of flaps, Taylor concluded that one of the main determinants of flap survival length was related to the distance between the perforator at the base of the flap and the next dominant perforator along a chosen axis. And the necrosis line of the flap appeared in the zone of choke vessels connecting adjacent territories [25–27]. Similar theory was subsequently presented by Rikimaru [28] and Thomas [29]. The largest area of skin viability was defined as the summation of the vascular territories of both the source vessel and its immediately neighboring perforator. Beyond this territory, flaps would not survive [27].
Based on the given theory, we concluded that the distal end of HDBPDAF at the middle phalanx could approach the proximal DB by capturing the distal DB in the proximal phalanx for long fingers because the next adjacent territory was near the spot. Whereas for the thumb, four dominant DBs, with one originating from the volar PDA of the thumb (located at the level of the middle third of the proximal phalanx) and the other three from the first dorsal metacarpal artery (located at the level of the base, the middle and distal third of the first metacarpal, respectively) were constantly present and two consistent anastomoses with the corresponding branches were located in the middle third of the first metacarpal and the proximal phalanx of the thumb, respectively [17]. According to its anatomic basis, the distal end of our HDBPDAF pedicled on the DB of the volar PDA at the proximal phalanx of the thumb could reach the middle third of the first metacarpal.
Quite interestingly, the distance between the two branches located at the middle third of the proximal phalanx of the thumb and the first metacarpal, respectively, was substantially equal to the distance between the DB of the proximal phalanx and fingertip. So, our extended and oversized HDBPDAF could adequately cover large fingertip and pulp defects of the thumb with the length of digital bone saved as much as possible. Similarly, for long fingers, the length of our extended HDBPDAF was equal to the distance between the DB located at the midpoint of middle phalanx and fingertip. Therefore, whether thumb or other fingers, it is more possible to maintain the length of injured fingers with our extended HDBPDAF. Moreover, satisfactory aesthetic and functional outcomes were successfully obtained in our patients.
Therefore, we prefer the use of HDBPDAFs on repairing distal soft tissue defects of fingers. The indications of our HDBPDAF include defect coverage of fingertip and pulp, dorsal, lateral or ventral side of thumb and other fingers, and even multiple fingers. Furthermore, our HDBPDAF could be an optimal alternative when the fingertip and pulp defects of thumb and other fingers were large enough and shortening the digital bone was against the will of the patient.
Despite many anatomical studies of DB of PDA published in the literature, the absence rate of DB has never been reported and discussed [12,13,30]. In our 44-digital series, the DB of PDA of two fingers were found to be absent during operation. Reluctantly, other flaps had to be taken into account accordingly.
In our experience, it’s better to incise only one side when initially harvesting the flap, and to confirm the presence of the DB of PDA at first. Although the introduction of advanced vessel detection technology, such as Doppler sonography [31] and computed tomographic angiography [32] may provide useful information on the DB anatomy, the availability of the equipment and expertise, added cost, and scheduling issues may prove impractical for most surgeons in the one-stage procedure. In fact, we rarely use any detection technology to predict the DB of PDA, preoperatively. We believe that designing and harvesting the HDBPDAF, based on the anatomical landmarks and our experience, are simple, effective, reliable, and applicable for any reconstructive surgeon.
After harvesting the HDBPDAF, an optimal aesthetic and functional restitution of the donor site was required. In order to cover the secondary defect and decrease morbidity of the donor site, dermal substitutes have been used in the wound management with excellent functional and aesthetic outcomes [33,34]. However, the price of dermal substitutes is relatively expensive, some patients refuse to use it in clinic, especially for the patients with finger injury. In this study, the donor site of the HDBPDAF was sutured directly or covered with autologous full-thickness skin graft according to the size of the donor site. The injured fingers had a mean TAM of 268.7 ± 5.2°, which was over 95% of the contralateral side (283.2 ± 6.4°, p < 0.05), with six fingers scored as excellent and 38 fingers scored as good grade. No significant limitation in active and passive activity was observed. Here, the TAM results showed that the postoperative mobility of the affected fingers recovered well.
In spite of the lower absent rate of DB, the HDBPDAF proves to be an optimal option for one-stage reconstruction of various defects of thumb and even multiple fingers, because of its thinness, good pliability, minimal donor site deformity, and the simplicity and rapidity of the procedure. Further anatomy should be made to identify the real absent rate of DB of PDA and map them precisely.
Ethical approval
The study was approved by the ethical review committee of the Second Affiliated Hospital of Soochow University with an approve No. EC2014086.
ORCID
Yong Zhang  https://orcid.org/0000-0002-2783-9768
https://orcid.org/0000-0002-2783-9768
References
[1] Paterson P, Titley OG, Nancarrow JD. Donor finger morbidity in cross-finger flaps. Injury. 2000;31(4):215–218. https://doi.org/10.1016/S0020-1383(99)00205-3
[2] Hehl R. The thenar flap. Handchirurgie. 1975;7(4):155–157.
[3] Cormack G. Reverse digital artery flaps: a note of caution regarding cold intolerance. Br J Plast Surg 1993;46(1):87–88. https://doi.org/10.1016/0007-1226(93)90076-N
[4] Lai-jin L, Xu G. The reverse dorsal metacarpal flap: experience with 153 cases. Ann Plast Surg. 2006;56(6):614–617. https://doi.org/10.1097/01.sap.0000205775.41405.fa
[5] Kawakatsu M, Ishikawa K. Dorsal digital perforator flap for reconstruction of distal dorsal finger defects. J Plast Reconstr Aesthet Surg. 2010;63(1):e46–e50. https://doi.org/10.1016/j.bjps.2009.05.014
[6] Qin JZ, Wang PJ. Fingertip reconstruction with a flap based on the dorsal branch of the digital artery at the middle phalanx: a simple and reliable flap. Ann Plast Surg. 2012;69(5):526–528. https://doi.org/10.1097/SAP.0b013e31821ee3c5
[7] Iwasawa M, Kawamura T, Nagai F. Dorsally extended digital island flap for repairing soft tissue injury of the fingertip. J Plast Reconstr Aesthet Surg. 2011;64(10):1300–1305. https://doi.org/10.1016/j.bjps.2011.04.026
[8] Imai H, Tajima T, Natsuma Y. Interpretation of cutaneous pressure threshold (Semmes-Weinstein monofilament measurement) following median nerve repair and sensory reeducation in the adult. Microsurgery. 1989;10(2):142–144. https://doi.org/10.1002/micr.1920100216
[9] Wang X, Lv J, Liu S, et al. Effect of dorsal nerve fascial island flap on repairing distal soft tissue defects at the proximal segment of the index, middle, ring, and little fingers. J Orthop Surg Res. 2022;17(1):413. https://doi.org/10.1186/s13018-022-03309-9
[10] Libberecht K, Lafaire C, Van Hee R. Evaluation and functional assessment of flexor tendon repair in the hand. Acta Chir Belg. 2006;106(5):560–565. https://doi.org/10.1080/00015458.2006.11679952
[11] Gummesson C, Atroshi I, Ekdahl C. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: longitudinal construct validity and measuring self-rated health change after surgery. BMC Musculoskelet Disord. 2003;4:11. https://doi.org/10.1186/1471-2474-4-11
[12] Braga-Silva J. Anatomic basis of dorsal finger skin cover. Tech Hand Up Extrem Surg. 2005;9(3):134–141.
[13] Endo T, Kojima T, Hirase Y. Vascular anatomy of the finger dorsum and a new idea for coverage of the finger pulp defect that restores sensation. J Hand Surg Am. 1992;17(5):927–932. https://doi.org/10.1016/0363-5023(92)90472-2
[14] Sebastin SJ, Mendoza RT, Chong AK, et al. Application of the dorsal metacarpal artery perforator flap for resurfacing soft-tissue defects proximal to the fingertip. Plast Reconstr Surg. 2011;128(3):166e–178e. https://doi.org/10.1097/PRS.0b013e318221ddfa
[15] Brunelli F, Vigasio A, Valenti P, et al. Arterial anatomy and clinical application of the dorsoulnar flap of the thumb. J Hand Surg Am. 1999;24(4):803–811. https://doi.org/10.1053/jhsu.1999.0803
[16] Moschella F, Cordova A, Pirrello R, et al. Anatomic basis for the dorsal radial flap of the thumb: clinical applications. Surg Radiol Anat. 1996;18(3):179–181.
[17] Pistre V, Pelissier P, Martin D, et al. Vascular blood supply of the dorsal side of the thumb, first web and index finger: anatomical study. J Hand Surg Br. 2001;26(2):98–104.
[18] Xiong X, Xu M, Shuai M, et al. Comparative study of the clinical effects of reverse digital artery island flaps and antegrade homodigital neurovascular island flaps for fingertip reconstruction. Ann Plast Surg. 2022;88(4):395–400. https://doi.org/10.1097/SAP.0000000000002967
[19] Bertelli JA, Khoury Z. Neurocutaneous island flaps in the hand: anatomical basis and preliminary results. Br J Plast Surg. 1992;45(8):586–590.
[20] Lai CS, Lin SD, Chou CK, et al. Innervated reverse digital artery flap through bilateral neurorrhaphy for pulp defects. Br J Plast Surg. 1993;46(6):483–488. https://doi.org/10.1016/0007-1226(93)90222-W
[21] Yuan C, Wang S, Wang Y, et al. Reverse digital artery island flap with versus without sensory nerve coaptation for finger pulp reconstruction. ANZ J Surg. 2023;93(1–2):281–287.
[22] Chen QZ, Sun YC, Chen J, et al. Comparative study of functional and aesthetically outcomes of reverse digital artery and reverse dorsal homodigital island flaps for fingertip repair. J Hand Surg Eur 2015;40(9):935–943. https://doi.org/10.1177/1753193415579300
[23] Okazaki M, Hasegawa H, Kano M, et al. A different method of fingertip reconstruction with the thenar flap. Plast Reconstr Surg. 2005;115(3):885–888; discussion 889–890. https://doi.org/10.1097/01.PRS.0000153221.39347.AB
[24] Han SK, Lee BI, Kim WK. The reverse digital artery island flap: clinical experience in 120 fingers. Plast Reconstr Surg. 1988;101(4):1006–1011; discussion 1012–1013.
[25] Callegari PR, Taylor GI, Caddy CM, et al. An anatomic review of the delay phenomenon: I. Experimental studies. Plast Reconstr Surg. 1992;89(3):397–407; discussion 417–418. https://doi.org/10.1097/00006534-199203000-00003
[26] Taylor GI, Corlett RJ, Caddy CM, et al. An anatomic review of the delay phenomenon: II. Clinical applications. Plast Reconstr Surg. 1992;89(3):408–416; discussion 417–418.
[27] Morris SF, Taylor GI. Predicting the survival of experimental skin flaps with a knowledge of the vascular architecture. Plast Reconstr Surg. 1993;92(7):1352–1361.
[28] Rikimaru H, Kiyokawa K, Inoue Y, et al. Three-dimensional anatomical vascular distribution in the pectoralis major myocutaneous flap. Plast Reconstr Surg. 2005;115(5):1342–1352.
[29] Thomas BP, Geddes CR, Tang M, et al. The vascular basis of the thoracodorsal artery perforator flap. Plast Reconstr Surg. 2005;116(3):818–822. https://doi.org/10.1097/01.prs.0000176253.42394.7c
[30] Braga-Silva J, Kuyven CR, Fallopa F, et al. An anatomical study of the dorsal cutaneous branches of the digital arteries. J Hand Surg Br. 2002;27(6):577–579. https://doi.org/10.1054/jhsb.2002.0830
[31] Hallock GG. Doppler sonography and color duplex imaging for planning a perforator flap. Clin Plast Surg. 2003;30(3):347–357, v–vi. https://doi.org/10.1016/S0094-1298(03)00036-1
[32] Ting JW, Rozen WM, Chubb D, et al. Improving the utility and reliability of the deep circumflex iliac artery perforator flap: the use of preoperative planning with CT angiography. Microsurgery. 2011;31(8):603–609. https://doi.org/10.1002/micr.20942
[33] Di Giuli R, Dicorato P, Kaciulyte J, et al. Donor site wound healing in radial forearm flap: a comparative study between dermal substitute and split-thickness skin graft versus full-thickness skin graft primary coverage. Ann Plast Surg. 2021;86(6):655–660. https://doi.org/10.1097/SAP.0000000000002777
[34] De Francesco F, Busato A, Mannucci S, et al. Artificial dermal substitutes for tissue regeneration: comparison of the clinical outcomes and histological findings of two templates. J Int Med Res. 2020;48(8):300060520945508. https://doi.org/10.1177/0300060520945508