ORIGINAL RESEARCH ARTICLE
Comparison of patient-reported achievements of goals and core outcomes with delayed breast reconstruction in irradiated patients: latissimus dorsi with an implant versus DIEP
Jonas Löfstranda,b, Anna Paganinia,b,c, Mattias Lidéna,b and Emma Hanssona,b
aDepartment of Plastic Surgery, Institute of Clinical Sciences, University of Gothenburg, Gothenburg, Sweden;
bRegion Västra Götaland, Sahlgrenska University Hospital, Department of Plastic Surgery, Gothenburg, Sweden;
cDepartment of Diagnostics, Acute and Critical Care, Institute of Health and Care Sciences, Sahlgrenska Academy, University of Gothenburg
ABSTRACT
Background: Different women’s individual goals with a breast reconstruction vary, and few studies compare techniques in light of the different goals. This study aimed to compare patient-reported core outcomes in patients reconstructed with deep inferior epigastric artery perforator (DIEP) flaps and latissimus dorsi (LD) flaps. Second, breast-related factors that the patients were particularly satisfied/dissatisfied with were analyzed.
Methods: This was a retrospective cross-sectional study, which includes women who had undergone mastectomy and radiation, followed by delayed breast reconstructions with either LD flap and implant or DIEP flap during 2007–2017. The patient-reported core outcomes of overall breast-specific quality of life, normality, women’s cosmetic satisfaction, self-esteem, emotional well-being, and physical well-being were analyzed using BREAST-Q.
Results: The patients were divided into LD and implant (n = 135 patients) and DIEP (n = 118 patients) groups, and both were demographically similar. The median follow-up was 8 years. The DIEP group scored significantly higher than the LD and implant group in five out of six domains. A high satisfaction was reported in questions regarding the feeling or appearance when having clothes on, whereas the greatest dissatisfaction was reported regarding questions entailing symmetry and the appearance without clothes.
Conclusion: After 7 years, patients’ breast-specific quality of life, normality, women’s cosmetic satisfaction, self-esteem, emotional well-being, and physical well-being seem to be higher in irradiated patients who have been reconstructed with DIEP flap as compared to patients reconstructed with LD flap and implant. In both groups, patient satisfaction is high regarding their appearance when clothed, whereas the lowest satisfaction scores were reported in situations without clothing.
KEYWORDS: Latissimus dorsi flap; deep inferior epigastric perforator flap; breast reconstruction; patient-reported outcome; patient satisfaction; long-term follow-up
Citation: Journal of Plastic Surgery and Hand Surgery 2023; 58: 74–81. DOI: https://doi.org/10.2340/jphs.v58.12417.
Copyright: © 2023 The Author(s). Published by MJS Publishing on behalf of Acta Chirurgica Scandinavica. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material, with the condition of proper attribution to the original work.
Received: 1 May 2023; Accepted: 1 June 2023. Published: 24 August 2023.
CONTACT Emma Hansson emma.hansson.2@gu.se Department of Plastic Surgery, Sahlgrenska University Hospital, Gröna Stråket 8, SE-413 45 Gothenburg, Sweden.
Competing interests and funding: No potential conflict of interest was reported by the author(s).
Introduction
A breast reconstruction is ultimately performed to increase a patient’s quality of life. Different women will have individual interpretations of what quality of life is, and therefore for choosing breast reconstruction [1,2]. The reasons are not always straightforward to explain [3,4], but purposes of a breast reconstruction can roughly by divided into physical and psychosocial goals [5–7]. Physically, a breast reconstruction should diminish the risk of the cancer treatment affecting the woman’s daily life, for example, in choice of clothes, activities, and work and eliminate the need for an external prothesis [5]. Psychosocially, a breast reconstruction should give rise to an improved body-image, feelings of femininity and sexual attractiveness, a reduction of symptoms of depression/anxiety [6,7], make the woman feel ‘whole again’ [5], and eliminate daily reminders of the breast cancer [6,7]. It is largely unexplored how different techniques, such as the deep inferior epigastric artery perforator (DIEP) flaps and latissimus dorsi (LF) flaps with an implant, compare the achievement of specific goals. Differences in effects on goals might have implications when a breast reconstruction technique is chosen. Previous studies comparing DIEPs and LDs have not focused on specific goals with breast reconstruction and often include few patients, and the results are somewhat inconclusive [8–11]. Two of the studies used non-validated, study-specific questionnaires [8,10].
The different goals of a breast reconstruction make outcome evaluation complex. The core outcome set for breast reconstruction [12], including items evaluating the aforementioned described goals such as overall breast-specific quality of life, normality, women’s cosmetic satisfaction (core items for both patients and professionals) and self-esteem, emotional well-being, and physical well-being (core items for patients alone) [12]. Aspects such as normality, self-esteem, and emotional well-being can be difficult to measure but are included as specific items in the BREAST-Q reconstruction module.
In Sweden, autologous and mixed (combining autologous tissue with an implant) techniques, DIEPs and LDs with implants, are offered mainly to patients who have received previous radiotherapy [13], which renders the possibility to compare these techniques in patients who prior to reconstruction have received similar cancer treatment, including mastectomy followed by radiotherapy. We hypothesize that the goals of improved cosmetic satisfaction, normality, self-esteem, and emotional and physical well-being are better achieved when a complete autologous technique is used, and that the patients are more satisfied with their decision to have a breast reconstruction. The primary aim of this study was to compare the core outcome measures of breast-specific quality of life and physical well-being, women’s cosmetic satisfaction, including satisfaction with outcome, and normality, self-esteem, and emotional well-being, after a reconstruction with a DIEP flap with that performed with an LD flap in combination with an implant. The secondary aim was to analyze breast-related factors that patients were particularly satisfied/dissatisfied with.
Materials and methods
Study design, protocol, and ethics
This study is a retrospective observational cohort study comparing breast satisfaction after breast reconstruction with an LD flap or a DIEP flap. It is part of the ‘Reconstruction with back donor site flaps study’ protocol (ClinicalTrials.Gov identifier NCT04526561). This study was vetted and approved by the Regional Ethical Committee of Gothenburg/the Swedish Ethical Review Authority (254-18 and 2021-00432) and conducted in accordance with the Helsinki Declaration and the Good Clinical Practice (GCP) guidelines. All participants gave their informed consent to participations, chart review, and to publication of the results.
Setting
This study was performed at Sahlgrenska University Hospital in Gothenburg, Sweden, where the Department of Plastic and Reconstructive Surgery currently performs about 350 breast reconstructions yearly, of which around 80 are autologous. Autologous reconstruction, most commonly by means of DIEP flap or LD flap in combination with an implant, is offered to women who have undergone radiation to the chest wall, in accordance with national guidelines [13]. The patient must have a body mass index (BMI) of ≤30, show absence of generalized disease, and abstain from smoking for at least 6 weeks prior to, and after, the operation. When both an LD flap and a DIEP flap are technically feasible, the patient herself chooses the reconstructive method to be performed. All autologous reconstructions were delayed procedures.
Participants
All women consecutively operated for a breast reconstruction with an LD flap with an implant or a DIEP flap following mastectomy and radiotherapy from 2007 to 2017 were recruited as participants. When both a LD flap with an implant and a DIEP flap were technically possible, the woman chooses the technique herself [13]. Participants were identified via the operation planning program and sent an envelope including information regarding the study, the questionnaires, a consent form, and a stamped return envelope. If unanswered, the participants received two reminders, after 2 and 5 weeks. All data were collected in September 2020–June 2021. Some of the participants had previously been randomized to either a DIEP flap or an LD flap in the GoBreast study (ClinicalTrials.Gov identifier NCT03963427) [14] (Figure 1).
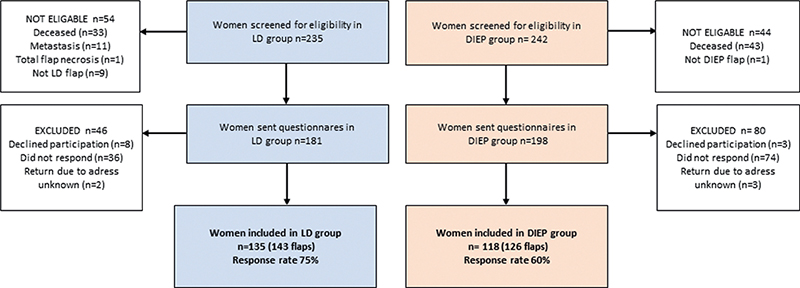
Figure 1. STROBE diagram of the included patients in the two groups.
Outcome measurements
BREAST-Q reconstruction (version 1) postoperative was used. The items and domains of the instrument were developed in North America with qualitative technique [15] and have been validated [16,17] and translated to Swedish. The following domains were analyzed: Satisfaction with breast/s (16 items), Satisfaction with outcome (7 items), Psychosocial well-being chest (10 items), Sexual well-being (6 items), Physical well-being chest (16 items), and Satisfaction with information (15 items). Each item is rated on a Likert scale from 1 to 3, 4, or 5, depending on the domain. For each domain, the raw scale-summed scores are transformed to Rasch logits, which are then transformed to a standardized score between 0 and 100, where a higher score indicates a better outcome/higher satisfaction. There are no anchor-based minimal important differences (MIDs) published for BREAST-Q [18]. Distribution-based MIDs, which indicate the lowest change value beyond the measurement error [19,20], are published for Satisfaction with Breasts: 4, Psychosocial Well-being: 4, Physical Well-being: 3, and Sexual Well-being: 4 [21]. Normative data have been described for two American populations including a total of 1500 women [22,23]. Individual BREAST-Q items that are specifically related to the core outcome measures were analyzed separately [12]. The use of BREAST-Q, authored by Drs. Klassen, Pusic, and Cano, was made under license from Memorial Sloan Kettering Cancer Center, New York, USA. Clinical data were collected from the medical charts.
Statistics
Descriptive data were given as both median and ranges, as well as means and standard deviations, and frequencies, when applicable. BREAST-Q data were treated as described in the manual, that is, if at least half of the items of a domain of BREAST-Q were answered, missing data were replaced with the mean of the answered items for each domain. The domain was excluded if more than half of the items were missing. QScoreTM was used to calculate scores between 0 and 100. According to the developers, the Rasch logits have been calibrated based on minimum and maximum logits in a calibrated data; therefore, the 0–100 scale has retained the metric properties achieved in the Rasch analysis, and the transformed standardized 0–100 can be considered a continuous scale, although the raw scores of BREAST-Q are ordinal [24]. For the domains satisfaction with breast/s and satisfaction with outcome, frequencies of different answers were given for each item, as well as for items e, f, and h in the psychosocial well-being domain.Differences between the two groups were performed with the non-parametric Mann–Whitney U-test for unpaired samples for ordinal values (BREAST-Q scores) and Pearson’s Chi-squared test (χ2) for categorical variables (BREAST-Q items). Statistical comparison was not made between the values of the groups and the norm population as we do not have access to the datasets, only the mean and SDs for the norms. All tests were two-tailed, and a p-value of ≤0.05 was considered to indicate a statistically significant difference. Statistical analyses were performed using Excel® version 16.30 (Microsoft Corporation, Redmond, Washington, USA) and SPSS® version 27.0.0.0 for Mac (IBM, Armonk, New York, USA).
Results
Participants
During 2007–2017, 467 patients underwent an autologous or mixed method breast reconstruction at the department. After exclusions, response rates were 75% in the LD and implant-group (135/181) and 60% in the DIEP group (118/198) (Figure 1). The follow-up period was a median of 7 years (range 3–14 years). Demography and surgical details were similar in the two groups (Table 1).
| LD and implant (n = 135 patients, 143 flaps) | DIEP (n = 118 patients, 126 flaps) | |
| Age at time of surgery (median (range), mean (SD)) |
53 (32–75) 52 (9.7) |
50 (33–66) 50 (7) |
| Age at time of questionnaire (median (range), mean (SD)) |
60 (38–81) 59 (10) |
58 (43–76) 59 (7) |
| Years since surgery (median (range), mean (SD)) |
7 (3–11) 7 (2) |
7 (3–14) 7 (3) |
| Number of flaps (n, (%)) | ||
| Unilateral | 127 (89) | 110 (87) |
| Bilateral | 16 (11) | 16 (13) |
| Reason for flap (n, (%)) | ||
| Radiation | 124 (92) | 115 (97) |
| Salvage | 11 | 61 |
| Previous implant-based reconstruction | 15 | 5 |
| Randomized in GoBreast | 3 | 10 |
| Implant/stages (n, (%)) | ||
| Two stages (expander+implant) | 28 (21) | |
| One stage (implant) | 106 (79) | |
| LD without an implant | 0 | |
| LD primarily augmented with fat (FALD) [25] | 0 | |
| Missing data | 1 (1) | |
| Denervation (n, (%)) | ||
| None | 15 (11) | |
| Primary | 33 (24) | |
| Secondary | 3 (2) | |
| Missing information | 84 (62) | |
| Reoperation due to complications (n complications, (%)) | ||
| Hematoma | 3 (2) | 5 (4) |
| Removal of implant | 7 (5) | - |
| Anastomosis insufficiency | - | 4 (3) |
| Wound dehiscence/necrosis requiring surgery | 5 (4) | 20 (17) |
| Nonsurgical complications in the breast (n, (%)) | ||
| Seroma | 0 | 0 |
| Infection | 10 (7) | 25 (21) |
| Wound dehiscence | 5 (4) | 33 (28) |
| Surgical corrections breast | ||
| Capsulectomy/adjustment of implant location | 16 (12) | - |
| Implant size change | 8 (6) | - |
| Lipofilling | 27 (20) | 19 (16) |
| Skin correction | 11 (8) | 10 (8) |
| Trimming of flap | 0 | 25 (21) |
| Liposuction | 0 | 14 (14) |
| Implant insertion | - | 1 (1) |
| Three of the salvage patients had radiation and are therefore counted in both groups. | ||
Differences in overall breast-specific quality of life and physical well-being between the LD and implant group and the DIEP group
The DIEP group reported a higher satisfaction and well-being in all domains of BREAST-Q, and the differences were statistically significant in all domains except physical well-being chest (Table 2).
| BREAST-Q | Norm values [22,23] Mean (SD) | LD and implant Mean (SD) Median (Range) | DIEP Mean (SD) Median (Range) | Difference in points between LD and implant and DIEP (distribution-based MIDs [21]) | Statistical difference between LD and implant and DIEP Mann–Whitney U-test | ||||
| Unilateral | Bilateral | Total t | Unilateral | Bilateral | Total t | p | |||
| (n = 127) | (n = 8, 16 flaps) | (n = 135, 143 flaps) | (n = 110) | (n = 8, 16 flaps) | (n = 118, 126 flaps) | ||||
| Satisfaction with breasts | 58 (18) 59 (21) |
54 (18) 55 (0–100) |
58 (16) 53 (40–91) |
54 (17) 53 (0–100) |
66 (19) 67 (16–100) |
72 (19) 67 (48–100) |
67 (19) 67 (16–100) |
13 (4) |
<0.001 |
| Satisfaction with outcome | 64 (27) 61 (0–100) |
67 (23) 67 (43–100) |
61 (26) 61 (0–100) |
76 (22) 75 (0–100) |
68 (22) 75 (43–100) |
76 (22) 75 (0–100) |
15 | <0.001 | |
| Psycho-social well-being | 71 (18) 70 (19) |
70 (25) 70 (0–100) |
67 (22) 58 (40–100) |
68 (24) 70 (0–100) |
76 (23) 82 (23–100) |
78 (18) 81 (47–100) |
76 (22) 81 (23–100) |
8 (4) |
0.010 |
| Sexual well-being | 56 (18) 57 (19) |
51 (25) 47 (0–100) |
52 (28) 42 (22–100) |
48 (25) 47 (0–100) |
56 (24) 54 (0–100) |
62.5 (20) 63.5 (39–100) |
57 (24) 54 (0–100) |
9 (4) |
0.018 |
| Physical well-being chest | 93 (11) 84 (13) |
73 (18) 74 (0–100) |
78 (17) 76 (57–100) |
74 (18) 74 (0–100) |
77 (18) 77 (18–100) |
81 (12) 80 (66–91) |
77 (18) 77 (18–100) |
3 (3) |
0.088 |
| Satisfaction with information | 56 (17) 54 (0–100) |
63 (24) 52 (44–100) |
56 (17) 54 (0–100) |
61 (18) 58 (0–100) |
61 (11) 60 (49–85) |
61 (17) 58 (0–100) |
5 | 0.012 | |
Sexual well-being and physical well-being chest were lower than the norms in the LD and implant group and similar to the norms in the DIEP group (Table 2).
Womens’ cosmetic satisfaction and satisfaction with outcome
The biggest differences between the groups could be seen for the domain Satisfaction with breast and Satisfaction with outcome (13 and 15 points, respectively) (Table 2). Satisfaction with breast was similar to the norm population in the LD and implant group and higher than the norms in the DIEP group (Table 2). The DIEP patients were statistically significantly more satisfied than the LD and implant patients with all breast-specific items expect for ‘bra comfort’ and ‘size of reconstructed breast’ (Figure 2).
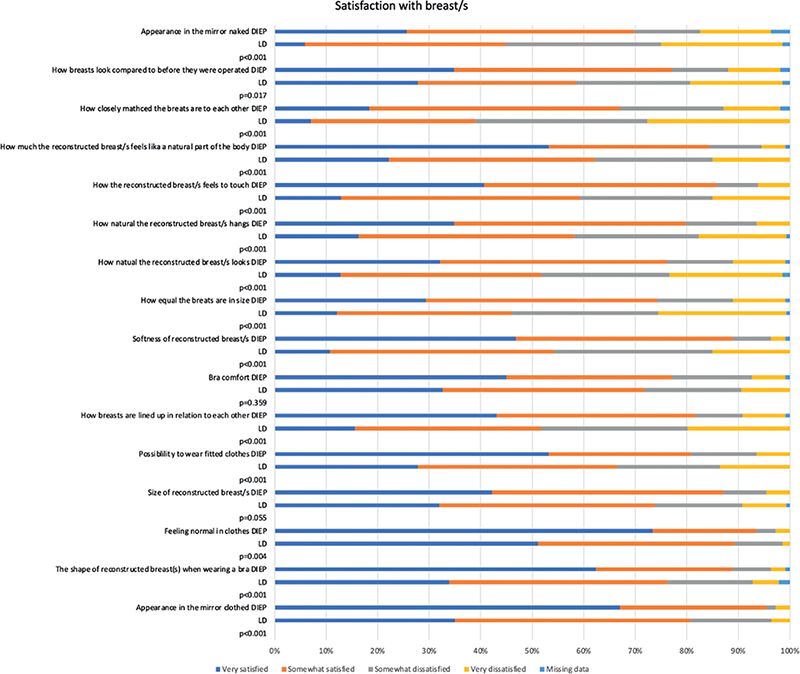
Figure 2. Women’s cosmetic satisfaction with different aspects of the reconstructed breast/s in the two groups. Women’s cosmetic satisfaction is part of the core outcome set of breast reconstruction [12]. The figure depicts the patients’ answers to individual items of the BREAST-Q domain ‘Satisfaction with breast/s’. Differences between the two groups were performed with Pearson’s Chi-squared test (χ2).
The great majority of women in both groups think that a breast reconstruction is better than no breast reconstruction, and that it changed their lives to the better, although the ratios of patients who agreed completely were slightly higher in the DIEP group (p = 0.09 and p = 0.017, respectively). Regarding expectations, one-fourth of the LD and implant patients and half of DIEP patients thought that they had been fully met (p < 0.001), whereas 35% of the LD and implant patients and 16% of the DIEP patients thought that the reconstruction had not turned out the way they had thought it would (p < 0.001).
Emotional well-being, normality, self-esteem, and femininity
Emotional well-being, as measured with the BREAST-Q domain Psychosocial well-being, was higher in the DIEP group than in the LD with implant group and well exceeded the distribution-based MIDs (Table 2). The proportion of women who agreed that they felt normal and feminine and had a high self-esteem were higher in the DIEP group, albeit only statistically significant for normality (Figure 3).
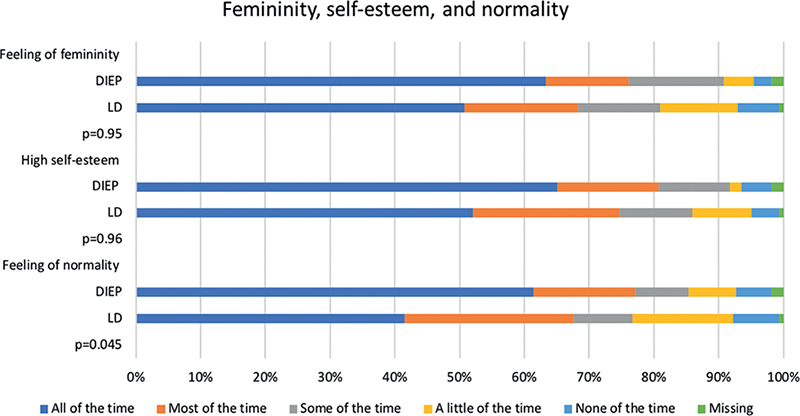
Figure 3. The patients’ feeling of femininity, self-esteem, and normality in the two groups. Femininity, self-esteem, and normality are part of the core outcome set of breast reconstruction [12]. Items from the BREAST-Q domain ‘Psycho-social well-being’ were used to evaluate femininity (item f), self-esteem (item e), and normality (item h). Differences between the two groups were performed with Pearson’s Chi-squared test (χ2).
Breast-related factors that patients were particularly satisfied/dissatisfied with
The breast aspects that most women were very satisfied or somewhat satisfied with were the same in both groups, that is, feeling normal in clothes (93% in the DIEP group and 89% in the LD and implant group, p = 0.004), appearance in the mirror clothed (95 and 81%, p > 0.001), and the shape of the reconstructed breast wearing a bra (90 and 78%, p < 0.001) (Figure 2). Similarly, the aspects that most women were very or somewhat dissatisfied with were the same in the two groups, including how closely the two breasts match each other (31% in the DIEP group and 61% in the LD and implant group, p > 0.001), appearance in the mirror naked (27 and 54%, p > 0.001), and how equal the breasts are in size (25 and 53%, p < 0.001) (Figure 2).
Discussion
This study evaluated long-term core outcomes of breast reconstruction with LD and implant and DIEP flaps, using validated PROMs. The results show that the DIEP group displays statistically significant higher score in five out of six BREAST-Q domains, with the exception being Physical well-being chest. These results strengthen the hypothesis that the DIEP flap is superior than the LD and implant flap in terms satisfaction with the reconstructed breast. The differences between the groups well exceeded the distribution-based MIDs in satisfaction with breasts, psychosocial well-being, and sexual well-being, which indicate that difference is beyond the measurement error. The findings support that of previous studies comparing the two methods [8–11]. The differences between groups shown in the present study also indicate that differences that seen previously between DIEP flaps and techniques using implants [26,27] seem to linger for many years after the reconstruction (Table 2), which is an important factor to consider when the reconstructive method is chosen. The overall 5-year survival rate of breast cancer of about 90% [28] implies that a breast reconstruction should be durable for many years.
The dimensions evaluated with BREAST-Q are influenced by a number of factors completely unrelated to breast reconstruction, such as social network, psychological factors, and income [29–32], as well as other physical circumstances, such as BMI [22,33–35], smoking [36,37], and comorbidity [38]. Factors such as ‘their feelings for the healthcare staff’, ‘if they felt cared for during the process’ and if feel they received a subpar pre- and postoperative information seem to play an important role [39]. Patient got a subpar pre- and postoperative information, thus misguided expectations.
Delayed breast reconstruction in irradiated patients is challenging since the breast footprint is often distorted or obliterated. Even if the aim is to recreate an identical twin of the contralateral breast, the result rarely approximates this, especially since a large skin paddle usually is needed for skin envelope. The BREAST-Q items ‘Shape of reconstructive breast wearing a bra’, ‘Appearance in the mirror clothed’, and ‘Feeling normal in clothes’ are goals that are more realistic to reach with breast reconstruction, and the majority of the patients in this study were satisfied with these items. However, the score for items as ‘Appearance in the mirror naked’ or ‘How closely matched the breasts are to each other’ displayed higher rates of dissatisfaction. The delayed nature of the reconstruction, with loss of skin envelope and nipple-areola complex in contrast to an immediate skin-sparing reconstruction, likely has a part in this, as mentioned earlier, but there might also be an information gap that is not preoperatively properly filled, suggesting a shortcoming in managing the patients’ expectations.
In the present study, the core outcomes of quality of life, women’s cosmetic satisfaction, and normality [12] were used to compare different reconstructive techniques. Even though they are considered core outcomes, the concepts are not straightforward to evaluate. The usage of ‘level of normality’ as an important outcome measure also coincides with patients often evaluating their breast reconstructions based on how ‘normal’ it makes them feel [39]. However, there are questions regarding what constitutes normality and how it should be measured, and there are no validated methods to measure ‘normality’ in breast reconstruction.
The definition of quality of life is not straightforward, as it can be health, health-related quality of life, and quality of life [40]. Previous studies have revealed that it is difficult to evaluate breast reconstruction with generic quality of life instruments as those instruments generally are not detailed enough to detect postoperative changes [26], and therefore, a disease-specific instrument was chosen in the present study. Nonetheless, experiences and feelings are complex to quantify scientifically and are affected by factors unrelated to the breast reconstruction, which makes it difficult to base the choice of method merely on patient reported outcomes. Other factors than the breast itself must be taken into consideration when the reconstructive method is chosen. One must also bear in mind that an autologous reconstruction involves a donor site, with subsequent donor site morbidity. The BREAST-Q domains analyzed in this study cover breast-specific and breast-related aspects. A head-to-head comparison of the donor site morbidity of different autologous methods would be useful in order to encompass all aspects of the breast reconstruction.
The long follow-up time of the present study is a major strength. There is no consensus regarding when breast reconstruction should be evaluated, and how long it is reasonable that the satisfaction with a breast reconstruction lasts, given that aging inevitably takes a toll on all parts of the body, including a breast reconstruction. Many studies have a follow-up of about 1–2 years, which could be considered short, given the high survival rates of breast cancer and the sustainability demands this should infer on breast reconstructions over the years. Weaknesses of this study include its retrospective design and there could be differences in the patients offered a DIEP flap and an LD flap with an implant, although the patient decided on technique herself if both options were technically possible. Moreover, another weakness of the this study is the lack of information on preoperative breast satisfaction, body-image, and other factors that could have affected the result and created a baseline difference between the two groups. Nonetheless, such factors should be less important for a long follow-up than for a short, as they are inevitably dynamic throughout most patients’ lives [41].
Conclusion
The result of the present study demonstrates that after a median of 7 years after the reconstruction, irradiated women seem to be more satisfied with a DIEP flap than an LD flap in combination with an implant. Moreover, the breast-related quality of life is higher in the DIEP group, and the other core outcomes of femininity, normality, and self-esteem also appear to favor the DIEP flap. The breast aspects that most women were very satisfied or somewhat satisfied with were similar in both groups. The findings imply that when technically possible and medically sound, a DIEP flap is a better option than an LD flap with an implant.
Acknowledgments
This study was funded by grants from The Swedish Cancer Society [21 0279 SCIA], the federal government under the ALF agreement [ALFGBG-724171 and ALFGBG-965161], and The Percy Falk Foundation (Stockholm, Sweden) for research into prostate cancer and breast cancer. The sources of funding had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
References
[1] Reaby LL. Reasons why women who have mastectomy decide to have or not to have breast reconstruction. Plast Reconstr Surg. 1998;101(7):1810–1818. https://doi.org/10.1097/00006534-199806000-00006
[2] Schmidt JL, Wetzel CM, Lange KW, Heine N, Ortmann O. Patients’ experience of breast reconstruction after mastectomy and its influence on postoperative satisfaction. Arch Gynecol Obstet. 2017;296(4):827–834. https://doi.org/10.1007/s00404-017-4495-5
[3] Henry M, Baas C, Mathelin C. Reconstruction mammaire apres cancer du sein : les motifs du refus [Why do women refuse reconstructive breast surgery after mastectomy?]. Gynecol Obstet Fertil. 2010;38(3):217–223. https://doi.org/10.1016/j.gyobfe.2009.10.003
[4] Zahedi S, Colvill K, Lopez M, Phillips LG. Implications of demographics and socioeconomic factors in breast cancer reconstruction. Ann Plast Surg. 2019;83(4):388–391. https://doi.org/10.1097/SAP.0000000000001919
[5] Elder EE, Brandberg Y, Bjorklund T, et al. Quality of life and patient satisfaction in breast cancer patients after immediate breast reconstruction: a prospective study. Breast. 2005;14(3): 201–208. https://doi.org/10.1016/j.breast.2004.10.008
[6] Flitcroft K, Brennan M, Costa D, Wong A, Snook K, Spillane A. An evaluation of factors affecting preference for immediate, delayed or no breast reconstruction in women with high-risk breast cancer. Psychooncology. 2016;25(12):1463–1469. https://doi.org/10.1002/pon.4087
[7] Rowland JH, Holland JC, Chaglassian T, Kinne D. Psychological response to breast reconstruction. Expectations for and impact on postmastectomy functioning. Psychosomatics. 1993;34(3):241–250. https://doi.org/10.1016/S0033-3182(93)71886-1
[8] Lindegren A, Halle M, Docherty Skogh AC, Edsander-Nord A. Postmastectomy breast reconstruction in the irradiated breast: a comparative study of DIEP and latissimus dorsi flap outcome. Plast Reconstr Surg. 2012;130(1):10–18. https://doi.org/10.1097/PRS.0b013e3182547aaf
[9] Yueh JH, Slavin SA, Adesiyun T, et al. Patient satisfaction in postmastectomy breast reconstruction: a comparative evaluation of DIEP, TRAM, latissimus flap, and implant techniques. Plast Reconstr Surg. 2010;125(6):1585–1595. https://doi.org/10.1097/PRS.0b013e3181cb6351
[10] Pluvy I, Bellidenty L, Ferry N, Benassarou M, Tropet Y, Pauchot J. Le lambeau perforant abdominal (DIEP) et grand dorsal autologue en reconstruction mammaire. Etude retrospective comparative a propos des 60 premieres patientes d’un meme operateur [Abdominal perforator flap (DIEP) and autologous latissimus dorsi in breast reconstruction. A retrospective comparative study about the first 60 cases of a same surgeon]. Ann Chir Plast Esthet. 2014;59(2):103–114. https://doi.org/10.1016/j.anplas.2013.10.004
[11] Thorarinsson A, Frojd V, Kolby L, Ljungdal J, Taft C, Mark H. Long-term health-related quality of life after breast reconstruction: Comparing 4 different methods of reconstruction. Plast Reconstr Surg Glob Open. 2017;5(6):e1316. https://doi.org/10.1097/GOX.0000000000001316
[12] Potter S, Holcombe C, Ward JA, Blazeby JM, Group BS. Development of a core outcome set for research and audit studies in reconstructive breast surgery. Br J Surg. 2015;102(11):1360–1371. https://doi.org/10.1002/bjs.9883
[13] Elander A, Lundberg J, Karlsson P, et al. Indikation för bröstrekonstruktion med kroppsegen vävnad med fri lambå. Report 2011:03. The guidelines were created by The Swedish Association of Local Authorities and Regions, The Swedish National Board of Health and Welfare, and The Swedish Society of medicine. Stockholm 2011. https://docplayer.se/3032093-Indikation-for-brostrekonstruktion-med-kroppsegen-vavnad-med-fri-lamba.html
[14] Brorson F, Thorarinsson A, Kolby L, Elander A, Hansson E. Early complications in delayed breast reconstruction: a prospective, randomized study comparing different reconstructive methods in radiated and non-radiated patients. Eur J Surg Oncol. 2020;46(12):2208–2217. https://doi.org/10.1016/j.ejso.2020.07.010
[15] Klassen AF, Pusic AL, Scott A, Klok J, Cano SJ. Satisfaction and quality of life in women who undergo breast surgery: a qualitative study. BMC Womens Health. 2009;9:11. https://doi.org/10.1186/1472-6874-9-11
[16] Cano SJ, Klassen AF, Scott AM, Cordeiro PG, Pusic AL. The BREAST-Q: further validation in independent clinical samples. Plast Reconstr Surg. 2012;129(2):293–302. https://doi.org/10.1097/PRS.0b013e31823aec6b
[17] Pusic AL, Klassen AF, Scott AM, Klok JA, Cordeiro PG, Cano SJ. Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q. Plast Reconstr Surg. 2009;124(2):345–353. https://doi.org/10.1097/PRS.0b013e3181aee807
[18] Weick L, Brorson F, Jepsen C, Lidén M, Jensen EW, Hansson E. Giving meaning to patient reported outcomes in breast reconstruction after mastectomy – a systematic review of available scores and suggestions for further research. Breast. 2021;61: 91–97. https://doi.org/10.1016/j.breast.2021.11.008
[19] Guyatt GH, Osoba D, Wu AW, Wyrwich KW, Norman GR, Clinical significance consensus meeting G. Methods to explain the clinical significance of health status measures. Mayo Clin Proc. 2002;77(4):371–383. https://doi.org/10.4065/77.4.371
[20] Crosby RD, Kolotkin RL, Williams GR. Defining clinically meaningful change in health-related quality of life. J Clin Epidemiol. 2003;56(5):395–407. https://doi.org/10.1016/S0895-4356(03)00044-1
[21] Voineskos SH, Klassen AF, Cano SJ, Pusic AL, Gibbons CJ. Giving meaning to differences in BREAST-Q scores: minimal important difference for breast reconstruction patients. Plast Reconstr Surg. 2020;145(1):11e–20e. https://doi.org/10.1097/PRS.0000000000006317
[22] Mundy LR, Homa K, Klassen AF, Pusic AL, Kerrigan CL. Breast cancer and reconstruction: normative data for interpreting the BREAST-Q. Plast Reconstr Surg. 2017;139(5):1046e–1055e. https://doi.org/10.1097/PRS.0000000000003241
[23] Klifto KM, Aravind P, Major M, et al. Establishing institution-specific normative data for the BREAST-Q reconstruction module: a prospective study. Aesthet Surg J. 2020;40(6):NP348–NP355. https://doi.org/10.1093/asj/sjz296
[24] Cano SJ, Klassen AF, Pusic AL. From BREAST-Q to Q-score: Using Rasch measurements to better capture breast surgery. Joint International IMEKO TC1+ TC7+ TC13 Symposium August 31st-September 2nd 2011; Jena, Germany; 2011.
[25] Longo B, D’Orsi G, Vanni G, Gagliano E, Buonomo CO, Cervelli V. Secondary breast reconstruction in small to medium-sized irradiated breasts: could Fat-Augmented LD (FALD) flap be a reliable alternative? Plast Reconstr Surg. 2023. https://doi.org/10.1097/PRS.0000000000010480
[26] Phan R, Hunter-Smith DJ, Rozen WM. The use of patient reported outcome measures in assessing patient outcomes when comparing autologous to alloplastic breast reconstruction: a systematic review. Gland Surg. 2019;8(4):452–460. https://doi.org/10.21037/gs.2019.07.04
[27] Eltahir Y, Krabbe-Timmerman IS, Sadok N, Werker PMN, de Bock GH. Outcome of quality of life for women undergoing autologous versus alloplastic breast reconstruction following mastectomy: a systematic review and meta-analysis. Plast Reconstr Surg. 2020;145(5):1109–1123. https://doi.org/10.1097/PRS.0000000000006720
[28] Mattiuzzi C, Lippi G. Current cancer epidemiology. J Epidemiol Glob Health. 2019;9(4):217–222. https://doi.org/10.2991/jegh.k.191008.001
[29] Sores A, Peto K. Measuring of subjective quality of life. Proc Econ Finan. 2015;32:809–816. https://doi.org/10.1016/S2212-5671(15)01466-5
[30] Katz SJ, Lantz PM, Paredes Y, et al. Breast cancer treatment experiences of Latinas in Los Angeles County. Am J Public Health. 2005;95(12):2225–2230. https://doi.org/10.2105/AJPH.2004.057950
[31] Alderman AK, Hawley ST, Janz NK, et al. Racial and ethnic disparities in the use of postmastectomy breast reconstruction: results from a population- based study. J Clin Oncol. 2009;27(32):5325–5330. https://doi.org/10.1200/JCO.2009.22.2455
[32] Mehta SK, Sheth AH, Olawoyin O, et al. Patients with psychiatric illness report worse patient-reported outcomes and receive lower rates of autologous breast reconstruction. Breast J. 2020;26(10):1931–1936. https://doi.org/10.1111/tbj.13936
[33] Erdmann-Sager J, Wilkins EG, Pusic AL, et al. Complications and patient-reported outcomes after abdominally based breast reconstruction: Results of the mastectomy reconstruction outcomes consortium study. Plast Reconstr Surg. 2018;141(2): 271–281. https://doi.org/10.1097/PRS.0000000000004016
[34] Ochoa O, Garza R, 3rd, Pisano S, Chrysopoulo M, Ledoux P, Arishita G, et al. Prospective longitudinal patient-reported satisfaction and health-related quality of life following DIEP flap breast reconstruction: Relationship with body mass index. Plast Reconstr Surg. 2019;143(6):1589–1600. https://doi.org/10.1097/PRS.0000000000005616
[35] Kamel GN, Mehta K, Nash D, et al. Patient-reported satisfaction and quality of life in obese patients: a comparison between microsurgical and prosthetic implant recipients. Plast Reconstr Surg. 2019;144(6):960e–966e.
[36] Cereijo-Garea C, Pita-Fernandez S, Acea-Nebril B, Rey-Villar R, Garcia-Novoa A, Varela-Lamas C, et al. Predictive factors of satisfaction and quality of life after immediate breast reconstruction using the BREAST-Q((c)). J Clin Nurs. 2018;27(7–8):1464–1474. https://doi.org/10.1111/jocn.14291
[37] Fracon S, Renzi N, Manara M, Ramella V, Papa G, Arnez ZM. Patient satisfaction after breast reconstruction: implants vs. autologous tissues. Acta Chir Plast. 2017;59(3–4):120–128.
[38] Mehta SK, Olawoyin O, Chouairi F, et al. Worse overall health status negatively impacts satisfaction with breast reconstruction. J Plast Reconstr Aesthet Surg. 2020;73(11):2056–2562. https://doi.org/10.1016/j.bjps.2020.08.093
[39] Beesley H, Ullmer H, Holcombe C, Salmon P. How patients evaluate breast reconstruction after mastectomy, and why their evaluation often differs from that of their clinicians. J Plast Reconstr Aesthet Surg. 2012;65(8):1064–1071. https://doi.org/10.1016/j.bjps.2012.03.005
[40] Karimi M, Brazier J. Health, health-related quality of lfie, and quality of life: what is the difference? Parmacoeconomics. 2016;34(7):645–649. https://doi.org/10.1007/s40273-016-0389-9
[41] Lee M, Damhorst ML. Women’s body image throughout the adult life span: a living history approach. J Women Aging. 2021;34(6):810–827.