REVIEW ARTICLE
A systematic review of differences in outcome between one and two stage palate repair in cleft lip and palate
Måns Cornefjord, MDa,b, Kristina Arnebrant, PhDc, Henrik Guné, MDa, Jan Holst, MD, PhDc,d, Kristina Klintö, SLP, PhDe,f, Mia Stiernman, MD, PhDa,b, Henry Svensson,a,b, Anna Paulina Wiedel, DDS, PhDb,g and Magnus Becker, MD, PhDa,b
aDepartment of Plastic and Reconstructive Surgery, Skåne University Hospital, Malmö, Sweden; bDepartment of Clinical Sciences in Malmö, Lund University, Malmö, Sweden; cDepartment of HTA Studies South, Skåne University Hospital, Lund, Sweden; dVascular Center, Skåne University Hospital, Malmö, Sweden; eDivision of Speech Language Pathology, Department of Otorhinolaryngology, Division of Speech and Language Pathology, Skåne University Hospital, Malmö, Sweden; fDivision of Speech Language Pathology, Phoniatrics and Audiology, Department of Clinical Sciences in Lund, Lund University, Lund, Sweden; gDepartment of Oral and Maxillofacial Surgery, Skåne University Hospital, Malmö, Sweden
ABSTRACT
The aim of this systematic review was to determine whether one-stage palatoplasty for children born with cleft lip and palate shows overall advantages in outcome compared with two-stage palatoplasty. The included studies were controlled studies of syndromic and non-syndromic children born with unilateral cleft lip and palate, bilateral cleft lip and palate, or isolated cleft palate. The interventions studied were one-stage palatoplasty and two-stage palatoplasty starting with the soft palate. The outcomes were facial growth, speech, hearing, presence of fistulae, other complications related to surgery, health-related quality of life, and health economics. In total, 14 original studies were included. Results were dichotomized into showing advantage for one- or two-stage palatoplasty for the respective outcome and compared with the results from six included systematic reviews. No overall advantage for either surgical strategy was found for any of the outcome measures. The certainty of evidence was highest for the presence of fistulae, followed by facial growth and speech. For several outcomes, the quality of the existing evidence was too low to allow for any conclusions to be drawn. Neither one- nor two-stage palatoplasty showed significant advantages in clinical outcomes compared with the other. Other aspects such as ethics, economics, or surgeon’s preference might hence be of more importance. Homogenous choices of outcome measures and defined minimal clinically important differences would facilitate further research.
KEYWORDS: Systematic review; cleft; cleft lip and palate; cleft palate; palatoplasty; palate repair; one-stage; two-stage; outcome
Citation: Journal of Plastic Surgery and Hand Surgery 2023; 58: 132–141. DOI: https://doi.org/10.2340/jphs.v58.13368.
Copyright: © 2023 The Author(s). Published by MJS Publishing on behalf of Acta Chirurgica Scandinavica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Received: 19 May 2023; Accepted: 10 October 2023; Published: 14 December 2023.
CONTACT Måns Cornefjord mans.cornefjord@med.lu.se Department of Plastic and Reconstructive Surgery, Skåne University Hospital, Malmö, Sweden and Department of Clinical Sciences in Malmö, Lund University, Malmö, Sweden. Jan Waldenströms gata 18, SE21428, Malmö, Sweden.
Competing interests and funding: The authors have no conflicts of interest to declare.
Funding for this study was provided by the foundation Stiftelsen för plastikkirurgisk forskning.
Introduction
Cleft lip and/or palate (CL/P), in its different variations, is the most common facial congenital malformation worldwide, occurring in approximately 1 in 1,000 live births (1). The malformation can affect several different areas including feeding, dental development, facial growth, speech development, hearing, aesthetics, and psychosocial well-being. Clefts including the palate are typically associated with problems concerning feeding, hearing, speech, and facial growth.
A vast number of techniques for primary palate repair have been described, as well as different strategies regarding the timing of surgery. Although the field has been studied extensively, the optimal technique and timing of surgical palate repair remain in debate. Several studies, both older and more recent ones, have indicated that the palate needs to be closed, at least partly if not completely, before an age of approximately 12–18 months for speech development to be satisfactory (2–5). However, it has also long been known that the surgical trauma and scarring that occurs as a result of the palatoplasty can affect facial growth in a negative way (6, 7). For this reason, staged surgical strategies have been developed more than 100 years ago (6), with one-stage techniques having been described even earlier (8). To facilitate speech development when using a staged technique, the soft palate is commonly repaired first, and the hard palate repair is delayed to allow optimal facial growth. The timing of both stages has varied greatly over the years (9–12). Today, we remain unsure of the optimal timing for staged palate repair, and whether a staged approach yields different end results compared with one-stage repair.
The aim of this study was to systematically review the existing scientific literature regarding one- versus two-stage palatoplasty. This was done in order to determine whether one strategy has significant advantages over the other, and hence should be preferred in a clinical setting. There are existing systematic reviews on the subject (13–17), but those have mostly focused only on children born with unilateral cleft lip and palate, and on certain outcomes such as fistula formation or facial growth. In this review we aim to include all patients born with a cleft in the palate and several relevant outcomes.
For two-stage palatoplasty, the soft palate is most often closed before the hard palate. Techniques for closing the hard palate first exist, for example through first closing the lip and hard palate with a vomerine flap in the first stage followed by soft palate closure in the second stage (18). In this review, however, only techniques where the soft palate was repaired first were considered.
Materials and methods
This review based on the results of a more extensive health technology assessment (HTA) report written by members of the project group and published by HTA Syd, part of the Swedish Agency for Health Technology Assessment and Assessment of Social Service in 2022 (19). The report is written in Swedish but includes a summary in English. The review protocol and data used in this review can be found in the report. The review was not registered.
Research question
A focused research question was designed using the Patient, Intervention, Comparison and Outcome (PICO) model (20). The research question was: Does one-stage palatoplasty show overall advantages compared with two-stage palatoplasty? To further focus the research question, several inclusion criteria were established. The PICO and inclusion criteria are shown in Table 1. All studies complying with the PICO and inclusion criteria were included. No other outcomes than the ones included in the PICO were studied.
Literature search
The search strategies were developed by two experienced information specialists in close collaboration with the rest of the project group. Databases used were Medline, Embase and Cochrane Library. The first searches were performed in February 2020 and were last updated in February 2023. Search terms used were the diagnoses of the patient population (cleft, palate, cleft palate, cleft and palate), the intervention, and the comparison (one phase, 1 phase, two phase, 2 phase, single stage, single phase, dual stage, dual phase, one stage, 1 stage, two stage, 2 stage, first stage, first phase, second stage, second phase, closure, repair, palate, palatal, palatoplasty, early, late, delayed, timing, first, primary, second, secondary). Results were limited to controlled human studies and systematic reviews published after 1970 and at the latest in December 2022. More detailed information concerning the search strategies can be found in Appendix B in a Swedish HTA-report written by members of the project group and published by HTA Syd in 2022 (19).
Study selection
The systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (21, 22). Database searches generated 5,775 records available for inclusion in the review. This number decreased to 3,540 after removal of duplicates. Two librarians screened the records and removed the obviously irrelevant ones. This left 841 abstracts to be screened by the rest of the project group. The abstracts were divided into two groups and each group was screened by two persons from the project group. The screening was unblinded and done independently using the screening tool Rayyan (23). Senior investigator M.B. screened all records. Consensus decisions in the project group were used for inclusion or exclusion of abstracts when the two persons screening judged the abstract differently. Screening of abstracts resulted in 195 full-text manuscripts for further processing. These full text manuscripts were assessed for relevance by the same project group members who had assessed the abstracts. If the same author had published several studies of the same patient group and outcome, but with different lengths of follow-up, only the study with the longest follow up was included. A total of 166 full-text manuscripts were deemed irrelevant, as they were outside the PICO and/or inclusion criteria, and were therefore excluded. The remaining 29 articles were assessed for quality including risk of bias according to the Swedish Agency for Health Technology Assessment and Assessment of Social Service’s handbook (24). The conventional domains for risk of bias (selection, performance, detection, attrition, reporting bias and conflict of interest) were evaluated on a three-grade scale (high, moderate, or low risk of bias) for each domain. Based on the evaluation from each domain an overall risk of bias for the entire study was obtained in consensus. Only studies with low or moderate total risk of bias were used in the narrative synthesis. Nine studies were excluded due to high overall risk of bias. The remaining 20 studies were included in the review: 14 original studies and six systematic reviews. The screening process is shown in a flowchart in Figure 1 and characteristics of the included studies are shown in Table 2. The table includes the population studied, type of study, and the measure used for a specific outcome. Details regarding the bias assessments of the included studies can be found in Appendix C of the aforementioned HTA report written by HTA Syd (19). Details on the assessment of studies that were excluded can be found in Appendix D in the same report (19). It should be noticed that the searches were updated after the publication of the HTA report, and hence some of the studies assessed in this review were not included in the report.
| Study | Year of publication | Study type, acronym | Population studied | Number of participants | Outcome studied |
| Willadsen et al. | 2017 | RCT, Scandcleft | P1a | 399* | O4 |
| Willadsen et al. | 2022 | RCT, Scandcleft | P1a | 399* | O2 |
| Heliövaara et al. | 2017 | RCT, Scandcleft | P1a | 399* | O1 |
| Lohmander et al. | 2017 | RCT, Scandcleft | P1a | 399* | O2, O4 |
| Rautio et al. | 2017 | RCT, Scandcleft | P1a | 399* | O4, O5 |
| Karsten et al. | 2020 | RCT, Scandcleft | P1a | 399* | O1 |
| Küseler et al. | 2020 | RCT, Scandcleft | P1a | 399* | O1 |
| Lundeborg-Hammarström et al. | 2020 | RCT, subgroup analysis from Scandcleft | P1a | 151 | O2, O4 |
| Pereira et al. | 2018 | RCT | P1a | 64 | O1, O4 |
| Reddy et al. | 2018 | RCT | P1a | 100 | O2, O4 |
| Jakobsson & Pontén | 1990 | Non-RCT | P1a, P1b, P2a, P2b | 237 | O4, O5 |
| Vedung et al. | 1995 | Non-RCT | P1a, P2a, P3a | 520 | O4 |
| Mikoya et al. | 2015 | Non-RCT | P1a | 68 | O1 |
| Otsuki et al. | 2022 | Non-RCT | P1a | 86 | O1 |
| *Including Arms A, B, C. Arm D excluded as it does not fulfill this study’s PICO. | |||||
| RCT: randomized controlled trial; P1a: Unilateral cleft lip and palate, without comorbidities/syndromes; P1b: Unilateral cleft lip and palate, with comorbidities/syndromes; P2a: Isolated cleft palate, without comorbidities/syndromes; P2b: Isolated cleft palate, with comorbidities/syndromes; P3a: Bilateral cleft lip and palate, without comorbidities/syndromes; O1: Facial growth; O2: Speech; O4: Presence of fistulae; O5: Other complications related to surgery. | |||||
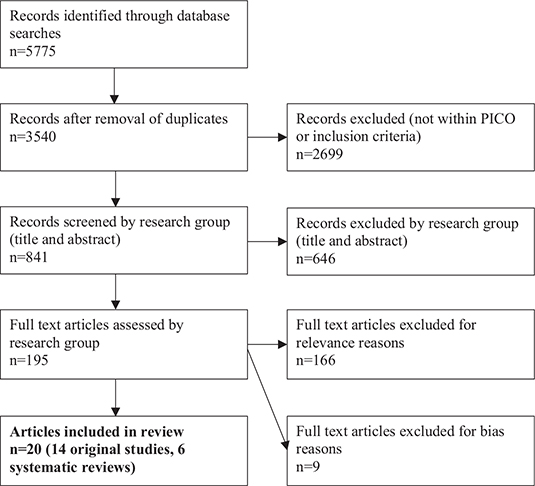
Figure 1. Flowchart illustrating the study selection process.
Data extraction
All 14 included original studies were thoroughly examined to determine whether they reported any significant differences in between one-and two-stage primary palate repair for the outcomes included in our PICO. This was done by the two project group members who had selected the particular study for inclusion. If a study included several of the included outcomes, assessment was performed separately for every outcome. No data were extracted from the six systematic reviews. The information and conclusions from these reviews were used to mirror and reflect the conclusions drawn from the data synthesis in the present systematic review.
Data analysis
Due to the nature of the published data, no meta-analysis could be performed (25). The main reasons for this were that many studies did not report confidence intervals, the heterogeneity in the methods of measuring outcomes, and the lack of definitions of minimal clinically important differences for many outcomes. Hence, a narrative analysis was performed for every outcome separately using the data extracted from the 14 included original publications. This analysis was obtained through extensive discussions within the project group to reach true consensus. The certainty of evidence was determined for every outcome separately using “The Grading of Recommendations Assessment Development and Evaluation System” (GRADE) classification (26).
Ethics
As the study is a systematic review of the existing scientific literature, meaning no new patients were included, ethical approval has not been obtained.
Results
Characteristics of the included original studies are presented in Table 2. It should be observed that some studies included multiple subpopulations and outcomes, where some of these were relevant for this review while others were outside of our defined PICO. Some studies also included several relevant outcomes but included too small population sizes or had too many patients lost to follow-up for certain outcomes to be included in the narrative analysis. In these cases, the studies were only included in the review for the populations and outcomes fulfilling the inclusion criteria. The study protocol for the Scandcleft trials (27) did not include any results and was hence not included in this study. However, it describes the methodology of the Scandcleft trials and should be read if the other Scandcleft trials are to be fully understood. Statistically significant differences were dichotomized into showing an advantage for either one-stage or two-stage palatoplasty, presented in Table 3. The results found in the included systematic reviews are discussed separately later in this review.
Outcome O1: Facial growth
Facial growth was reported in six original studies. Three of these were Randomized controlled trials (RCT) within the Scandcleft trials (28–30), one was an independent RCT (31), and two were non-RCTs (32, 33). It is worth observing that the studies that are part of the Scandcleft trials all included the same patient population, although the number of patients lost to follow-up differed slightly. Different outcome measures were used in the studies. Heliövaara et al. (28) and Pereira et al. (31) used 5-year-old index (5Y index) evaluations of dental relationships. Karsten et al. (29) used the Modified Huddart-Bodenham index (MHB index) for evaluating dental relationships and Mikoya et al. (32) used the 5Y index and the Huddart-Bodenham index (HB index). Küseler et al. (30) evaluated facial growth through cephalometric measurements. Otsuki et al. (33) used both cephalometric measurements and Great Ormond Street, London, and Oslo (GOSLON) yardstick assessments of dental relationships. All studies focused on non-syndromic children born with unilateral cleft lip and palate (UCLP) (P1a). Pereira et al. (31) showed significantly better scores for the 5-year-old index for the two-stage group, as did Mikoya et al. (32). The latter, however, only noticed a difference in transversal growth and not in sagittal growth. Otsuki et al. (33) found longer anterior-posterior length of the maxilla, lower posterior facial height, larger angle between the nasal floor plane and the SN plane, and better GOSLON yardstick scores in the two-stage group. They conclude that the two-stage approach resulted in better dental relationships and anterior-posterior maxillary growth than the one-stage protocol. The three remaining original studies showed no significant differences between one- and two-stage palatoplasty.
Narrative synthesis
Results from the included studies were somewhat disparate. Three out of six showed an advantage for the two-stage group. However, these three studies (31–33) were rather small (n = 64, n = 68, and n = 86, respectively) and follow-up was limited to between 5 and 8 years of age. Furthermore, in one of them (32) differences were only found for transversal growth. The conclusion drawn by the project group was that no overall advantages were seen for either approach when it comes to growth outcomes in the non-syndromic UCLP population, however a tendency toward favorable results for the two-stage group was seen. As all studies focused on the non-syndromic children born with UCLP, no conclusions could be drawn regarding the other patient groups included in our PICO.
Outcome O2: Speech
Speech outcomes were reported in four original studies. Two of these were RCTs within the Scandcleft trials (34, 35), one was a subgroup analysis within the Scandcleft trials (36), and one was an independent RCT (37). In all the studies, speech was evaluated through perceptual speech assessment. However, the assessments focused on various aspects of cleft palate speech. Willadsen et al. (34) studied consonant proficiency and velopharyngeal competence, Lohmander et al. (35) studied hypernasality and velopharyngeal competence, while Lundeborg-Hammarström et al. (36) evaluated velopharyngeal competency and consonant proficiency. All were part of the Scandcleft trials and included the same patient population, although Lundeborg-Hammarström et al. (36) only focused on a subgroup, namely trial 2 in the Scandcleft trials. Reddy et al. (37) reported hypernasality in an independent RCT. All studies focused on non-syndromic children born with UCLP (P1a). In one of the studies published by Willadsen et al. (34), the one-stage group performed significantly better than the two-stage group when it came to consonant proficiency, but conversely velopharyngeal competence was significantly better in the two-stage group. No significant differences between one- and two-stage palatoplasty were found in the other studies.
Narrative synthesis
In all studies but one, no differences in speech outcomes were seen between one- and two-stage palatoplasty in the UCLP group. One study showed better consonant proficiency in the one-stage group but better velopharyngeal competence in the two-stage group. Hence, the conclusion drawn by the project group was that no overall advantages were seen for either approach when it comes to speech outcomes. No conclusions could be drawn regarding the other patient groups included in our PICO.
Outcome O3: Hearing
Hearing was reported in a few of the screened studies, but none of these fulfilled the other inclusion criteria. Hence, no studies reporting hearing outcomes were included in this review.
Narrative synthesis
No conclusions could be drawn, as no studies reporting hearing outcomes were included.
Outcome O4: Presence of fistulae
Eight original studies reporting the presence of fistulae were included. Of these, three were RCTs within the Scandcleft trials (35, 38, 39), one was a subgroup analysis within the Scandcleft trials (36), two were independent RCTs (31, 37), and two were cohort studies (40, 41). The three studies that were part of the Scandcleft trials reported surgically repaired fistulae (35, 38, 39). So did Lundeborg-Hammarström et al. (36) in a subgroup analysis of the Scandcleft patient population, namely Scandcleft trial 2. Vedung (41) also reported fistulae requiring surgical repair. In Reddy et al. (37) the type of fistula was not specified. The other included studies (31, 40) reported all fistulae (repaired and non-repaired). In all studies, the patient population was non-syndromic children born with UCLP (P1a). Vedung (41) also included children with iCP and BCLP (P1a, P2a and P3a), and Jakobsson & Pontén (40) included both children with UCLP and iCP with and without comorbidities/syndromes (P1a, P1b, P2a, and P2b). Vedung (41) noticed significantly fewer fistulae in the two-stage group for children born with BCLP, but conversely fewer fistulae in the one-stage group for children with iCP. All the other original studies reported no significant differences between one- and two-stage palatoplasty.
Narrative synthesis
The conclusion drawn by the project group was that no clear overall differences in presence of fistulae were seen between one- and two-stage palatoplasty for non-syndromic patients born with UCLP. Other patient groups were included in two of the studies, but the scientific evidence was deemed to be too limited to draw any conclusions for these groups.
Outcome O5: Other complications related to surgery
Complications related to surgery were reported in two studies (39, 40). One was an RCT within the Scandcleft trials (39), and the other was a cohort study (40). In Rautio et al.’s (39) study only children with UCLP (P1a) were included. They reported frequency of perioperative airway problems, bleeding, and rates of infection. Significantly fewer airway problems were seen in the one-stage group, but no differences were seen for the other outcome measures. Jakobsson & Pontén (40) included syndromic and non-syndromic patients with UCLP or iCP (P1a, P1b, P2a, and P2b) and reported bleeding, need for blood transfusion and rates of infection. No statistical analysis was performed in Jakobsson & Pontén’s study (40), and hence no statistically significant differences between one- and two-stage palatoplasty were reported in this study.
Narrative synthesis
The conclusion drawn by the project group was that no clear overall differences in rates of complications related to surgery were seen between one- and two-stage for non-syndromic children born with UCLP. Although one study (39) found a difference in rates of transient airway problems, this was only reported in one single study, and the difference was only seen for one of the studied potential complications. Other patient groups were included in two of the studies, but the scientific evidence was deemed to be too limited to draw any conclusions for these groups.
Outcome O6: Health-related quality of life
Health-related quality of life was not reported in any of the included studies.
Narrative synthesis
No conclusions could be drawn, as no studies reporting health-related quality of life were included.
Outcomes O7a and O7b: Health economics
No aspects of health economics were reported in any of the included studies.
Narrative synthesis
No conclusions could be drawn, as no studies reporting outcomes related to health economics were included.
Certainty of evidence according to GRADE
The only patient group included in all studies was children born with UCLP without comorbidities/syndromes (P1a). No other patient group was included in more than two studies. GRADE assessment of the certainty of evidence for the non-syndromic UCLP group for the respective outcomes is shown in Table 4.
The highest certainty of evidence was found for the presence of fistulae (O4). The scientific certainty was deemed to be moderate (⊕⊕⊕○) for the conclusion that there is no difference in presence of fistulae between groups of children born with UCLP, without comorbidities/syndromes, operated with one- or two-stage palatoplasty. For the outcomes facial growth (O1) and speech (O2), the scientific certainty of the conclusion that there is no difference in these outcomes between groups of children born with UCLP, without comorbidities/syndromes, operated with one- or two-stage palatoplasty, was deemed to be low (⊕⊕○○). The certainty of scientific evidence for the rate of complications related to surgery (O5) was deemed to be very low (⊕○○○). Hence, no conclusions could be drawn regarding the differences between groups of children born with UCLP, without comorbidities/syndromes, operated with one- or two-stage palatoplasty when it comes to complications related to surgery. No conclusions could be drawn regarding hearing (O3), health-related quality of life (HRQoL) (O6), or health economics (O7a and O7b) as these outcomes were not reported in any of the included studies.
Comparison with results from systematic reviews
The conclusions and quality of evidence presented above were compared with the findings from the included systematic reviews. For facial growth, the two systematic reviews (13, 14) evaluated facial growth using cephalometric measurements, and found no differences between one- and two-stage palatoplasty. This was in accordance with our synthesis. For the presence of fistulae, two systematic reviews (15, 16) showed no differences between one- and two-stage palatoplasty, while one (17) found better results (fewer fistulae) in the one-stage group. This fit well with the conclusions drawn from the original studies. One systematic review by Wadde et al. evaluated several aspects of cleft care (42), with fistula formation and hypernasality being the outcomes relevant to this review. Only one study was included in the review with regard to these outcomes, the RCT performed by Reddy et al. (37), which is also included in our systematic review. The findings from the systematic reviews, and comparisons with the present review, are shown in Table 5.
Discussion
Whether or not cleft palate should be repaired in one or two stages has been discussed for a long time, with both one- and two-stage techniques being described more than 100 years ago (6, 8). Several studies have indicated that the palate needs to be repaired at least in part before 2 years of age for speech development to be adequate (2–5). It has also been shown that closure of the hard palate in adolescence gives superior results when it comes to facial growth (11), but at the cost of worse speech development (3). However, whether two-stage repair with early closure of the hard palate gives different results than one-stage repair remains a point of discussion. In this review we defined early closure as repairing the hard palate before 5 years of age. This is older than in many of the included studies, which was a way of ensuring that no relevant studies were excluded.
This review showed no clear advantages in favor of either one- or two-stage palatoplasty with regard to facial growth, speech and presence of fistulae. The evidence was strongest when it came to the presence of fistulae, but weaker for speech and facial growth. For the remaining outcomes; hearing, complications related to surgery, and HRQoL, the available scientific evidence was simply too limited to draw any conclusions. The same went for groups other than UCLP without additional comorbidities/syndromes (P1a), who represent a very limited number of the included patients in this review (15–17, 40, 41). This was in spite of the fact that children with UCLP only represent around 40% of the total CL/P population (43), and that approximately 30% of clefts are associated with additional comorbidities/syndromes (44, 45).
The limited quality of the studies and the relatively small number of studies were the main reasons for the low reliability of the existing scientific evidence. All the included studies were assessed for bias, and only studies that were deemed to have a low or moderate risk of bias were included. In fact, none of the included studies was deemed to have low risk of bias.
The risks of reporting bias, performance bias, and detection bias in particular decreases the quality of the included studies and the scientific evidence. The largest studies were the Scandcleft trials (28–30, 34, 35, 38, 39) and the studies by Jakobsson & Pontén (40) and Vedung (41). Even though these studies are large and ambitious, especially the Scandcleft trials, they are few and not free of risks of bias, which limits the conclusions that can be drawn. This is discussed further next.
The patient selection process was well described in the included RCTs (27, 31, 37) indicating a low risk of selection bias. The non-RCTs were deemed to have a moderate risk of selection bias. Jakobsson & Pontén (40) and Vedung (41) retrospectively assessed patient records and divided the subjects into a one-stage and a two-stage group depending on the surgical technique used. The technique chosen depended on when the patients were operated and the surgical protocol that was in use at that certain point in time. In Mikoya et al. (32) the two groups were treated parallelly, and the technique used depended on to which department the patient was referred, hence there was no randomization.
Many of the studies came from the Scandcleft trials (28–30, 34–36, 38, 39), meaning that many of the included children were the same in several studies, decreasing the number of unique patients. Also, the Scandcleft articles were written by the same research group, increasing the uncertainty of the published data as it is yet to be reproduced by other research groups in different settings.
Several of the included studies were RCTs (28–31, 34–39) but understandably had to use unblinded operators, which inherently increases the risk of performance bias. This is a weakness that is difficult to avoid when conducting research on surgical techniques and outcomes, as it is impossible to use blinded surgeons and patients. Assessors of outcome may be blinded, however this may also be difficult as, for example, the pattern of scarring may provide a hint regarding which technique has been used. Hence, most of the included studies presented with a rather high risk of detection bias. Assessors were blinded in most RCTs, but in one study the surgeon was the one doing the follow-up assessment (37). In the study by Reddy et al. (37) information on documentation of speech was missing, and the methods for calculation of reliability and reporting of hypernasality were vaguely described. One cohort study (40) did not conduct any statistical analysis, and hence the significance of the findings was difficult to assess.
One factor that may influence outcomes, other than the choice of surgical technique, is age at repair(s). The timing of surgery differed between the included studies, and within studies. According to the Scandcleft study protocol (27), one-stage repair was performed at an age of around 12 months. The first stage of two-stage repairs was performed at 3–4 months, and the second stage at 12 months (Arm A) or 36 months (Arm B). A rather similar approach was used by Pereira et al. (31) and Reddy et al. (37) with one-stage repairs being performed at 9–13 months, and 2-stage repairs at approximately 11–13 months (first stage) and 24–39 months (second stage). Mikoya et al. (32) used an approach with later repairs; one-stage surgery and the first stage of two-stage repair at 18 months, and the second surgery of the two-stage repairs at an age of 5–7 years. Jakobsson & Pontén (40) and Vedung (41) presented results from a long period of time, where the surgical strategies had varied. One-stage repair was performed at around 18–24 months, but the timing of the two-stage repairs varied between approximately 6 and 18 months (first stage), and 2 and 6 years (second stage). As it has been shown that a late closure of the palate may lead to better facial growth (11), this may explain the superior transversal growth outcomes in the two-stage group shown by Mikoya et al. (32). Unfortunately, neither of the studies where the hard palate was closed at the oldest age reported speech outcomes, which theoretically could have been affected by the late closure (2–5). Interestingly, one of the Scandcleft trials saw inferior speech outcomes in the two-stage group where the hard palate was repaired at 36 months (Arm B) compared with when it was repaired at 12 months (Arm A) (38). However, this difference was only seen for one speech outcome, namely PCC score (Percent Consonants Correct).
As argued in the Scandcleft trials, the operating surgeon’s experience and familiarity with the chosen surgical strategy may play a more important role for the outcome than the choice of surgical technique (46). Furthermore, even though the same technique is used, other factors such as the lines of incision and area of dissection may differ between surgeons. In these trials, many of the operating surgeons had to use one technique they were familiar with, and one new technique (39). The research group tried to minimize the effect of learning curve by allowing the surgeons to use the unfamiliar technique for 1 year before the commencement of the study. However, this relative lack of experience may explain, for example, the higher rates of fistulae when using the unfamiliar technique (although the differences where not statistically significant) (39). When it comes to the other included studies, Mikoya et al. (32), Reddy et al. (37), and Pereira et al. (31) describe the operating surgeons as experienced with the techniques used, whilst the experience is not discussed in Jakobsson & Pontén’s (40) and Vedung’s (41) studies. Therefore, it is difficult to draw any conclusions regarding the effect of surgical experience on outcomes from these studies.
Factors such as ethics and health economics become more important if, as the present review showed, there are no differences in strictly medical outcome between one- and two-stage palatoplasty. One may claim that it is ethically and economically favorable to repair the palate in one stage rather than two, as the psychological stress on the child is likely to be smaller (47) as well as the costs. Furthermore, another ethical aspect is the displacement effect, meaning that more surgical interventions per patient might restrict other patients’ access to surgery even more in a setting where resources are limited.
Difficulties encountered when performing this review included a relatively small number of included studies, that many of the studies were from the same research project and group, the heterogeneity in outcome measures and reporting, and the lack of clearly defined minimal clinically important differences for the studied outcomes. However, this was a calculated risk when forming the research question and inclusion criteria. We chose to only include studies with a minimum of 25 patients in each group (one- and two-stage palatoplasty) as smaller studies are associated with a higher risk of bias (48). Analyzed outcomes were heterogenous. To avoid this, however, we would have had to include only one measurement/assessment method per outcome, which would have decreased the number of appropriate studies even further. Whether, and how, the choice of outcome measures in the included studies might have affected the results is challenging to assess. Certain studies chose to dichotomize results, such as the studies by Lohmander et al. (35) and Lundeborg-Hammarström et al. (36) where velopharyngeal competence was calculated on a 0–4 and 0–6 scale, respectively, but dichotomized into velopharyngeal competence or incompetence. When results are simplified in such a manner, it will be more difficult to detect small statistically significant differences between the groups. One the one hand, when results are simplified in such a manner, it will be more difficult to detect small statistically significant differences between the groups. Comparing completely different measures for the same outcome, such as the cephalometric measurements presented in one study (30), the (M)HB index scores presented in two studies (29, 32), and the 5Y index scores presented in three studies (28, 31, 32), is even more difficult. The fact that the majority of the included studies did not find any significant differences in outcome between the groups, however, makes this assessment more reliable. Had differences been observed for certain outcome measures, but not for others, one would have had to analyze the reasons for this even more thoroughly. This goes not only for facial growth but also for the other outcomes studied. For instance, when it comes to fistula formation, some studies assessed all fistulae (31, 40), whilst others assessed fistulae requiring surgical repair (35, 36, 38, 39, 41). Whether or not a fistula needs to be surgically repaired is a subjective assessment that can differ from surgeon to surgeon. One the one hand, whether or not a fistula needs to be surgically repaired is a subjective assessment that can differ from surgeon to surgeon.
Another limitation that needs to be addressed is the fact that very few of the included studies had followed the patients through adolescence, and it is known that facial growth continues until 15 years of age or longer (49). Hence, it is possible that a longer follow-up time would show differences in facial growth that were not found in this review.
Strengths include the extensive literature search that was designed by librarians with extensive experience in this type of research and a thorough study selection process that was performed according to well-established guidelines (20–22).
Further research needs to be carried out in the field if reliable conclusions are to be drawn, especially for groups of CLP patients other than UCLP without additional comorbidities/syndromes. A more homogenous choice of outcome measures would greatly facilitate comparisons between studies and metanalysis, as would clearly defined minimal clinically important outcomes. The Scandcleft trials have shown that it is challenging to design an RCT that can answer our research question, and alternative approaches could include, for example, studies that are based on the extensive cleft registries that exist in some countries. Barriers towards conducting further research to try to answer the research question exist. Firstly, in order to assess the final outcomes, very long follow-up times are needed especially for facial growth. This presents a challenge in itself and increases the risk of a large proportion of patients being lost to follow-up, which would in turn decrease the reliability of the scientific evidence. Secondly, deciding on minimal clinically important outcomes is difficult as there are no clear-cut definitions of when, for example, hampered maxillary growth or mild hypernasality affects the daily life of the patient. This is also most certainly dependent on the individual patient’s experience. The issue of heterogenous outcome measures is perhaps a bit easier to handle. If the international community of cleft care could agree on certain validated and reliable outcome measures to use, comparison between studies would be greatly facilitated. However, most outcome measures have certain disadvantages, such as subjectivity of assessments or the need of specialized and experiences assessors.
In conclusion, we found some evidence suggesting that there are no differences in facial growth, speech, and presence of fistulae between one- and two-stage palatoplasty for children born with UCLP without comorbidities/syndromes. Other factors such as ethical considerations, health economics, and the surgeons’ familiarity with the different techniques may thus play a more important role for a surgeon’s choice of surgical strategy.
Acknowledgments
The authors would like to thank Hans Mark, Laura Dines and Ragnheidur Steingrimmsdottir for their various contributions to the research project.
ORCID
Måns Cornefjord  https://orcid.org/0000-0003-4281-8858
https://orcid.org/0000-0003-4281-8858
Kristina Arnebrant  https://orcid.org/0000-0001-7480-0746
https://orcid.org/0000-0001-7480-0746
Henrik Guné  https://orcid.org/0000-0002-0307-0739
https://orcid.org/0000-0002-0307-0739
Jan Holst  https://orcid.org/0000-0001-6861-7662
https://orcid.org/0000-0001-6861-7662
Kristina Klintö  https://orcid.org/0000-0002-7044-9386
https://orcid.org/0000-0002-7044-9386
Mia Stiernman  https://orcid.org/0000-0002-2563-7679
https://orcid.org/0000-0002-2563-7679
Henry Svensson  https://orcid.org/0000-0002-1876-5971
https://orcid.org/0000-0002-1876-5971
Magnus Becker  https://orcid.org/0000-0002-1915-1736
https://orcid.org/0000-0002-1915-1736
References
[1] Oner DA, Tastan H. Cleft lip and palate: epidemiology and etiology. Otorhinolaryngol Head Neck Surg. 2020; 5: 1–5. https://doi.org/10.15761/OHNS.1000246
[2] Dorf DS, Curtin JW. Early cleft palate repair and speech outcome. Plast Reconstr Surg. 1982; 70(1): 74–81. https://doi.org/10.1097/00006534-198207000-00015
[3] Rohrich RJ, Rowsell AR, Johns DF, et al. Timing of hard palatal closure: a critical long-term analysis. Plast Reconstr Surg. 1996; 98(2): 236–246. https://doi.org/10.1097/00006534-199608000-00005
[4] Shaffer AD, Ford MD, Losee JE, et al. The association between age at palatoplasty and speech and language outcomes in children with Cleft Palate: an observational chart review study. Cleft Palate Craniofac J. 2020; 57(2): 148–160. https://doi.org/10.1177/1055665619882566
[5] Haapanen ML, Rantala SL. Correlation between the age at repair and speech outcome in patients with isolated cleft palate. Scand J Plast Reconstr Surg Hand Surg. 1992; 26(1): 71–78. https://doi.org/10.3109/02844319209035186
[6] Gillies HD, Fry WK. A new principle in the surgical treatment of ‘congenital cleft palate’, and its mechanical counterpart. Br Med J. 1921; 1(3140): 335–338. https://doi.org/10.1136/bmj.1.3140.335
[7] Herfert O. Fundamental investigations into problems related to cleft palate surgery. Br J Plastic Surg. 1958; 11: 97–105. https://doi.org/10.1016/S0007-1226(58)80014-4
[8] Von Langenbeck B. Die Uranoplastik mittelst Ablösung des mucös-periostalen Gaumenüberzuges. Berlin: August Hirschwald; 1861.
[9] Rohrich RJ, Love EJ, Byrd HS, Johns DF. Optimal timing of cleft palate closure. Plast Reconstr Surg. 2000; 106(2): 413–21; quiz 22; discussion 23–25. https://doi.org/10.1097/00006534-200008000-00026
[10] Gaggl A, Feichtinger M, Schultes G, et al. Cephalometric and occlusal outcome in adults with unilateral cleft lip, palate, and alveolus after two different surgical techniques. Cleft Palate Craniofac J. 2003; 40(3): 249–255. https://doi.org/10.1597/1545-1569(2003)040<0249:CAOOIA>2.0.CO;2
[11] Schweckendiek W, Doz P. Primary veloplasty: long-term results without maxillary deformity. a twenty-five year report. Cleft Palate J. 1978; 15(3): 268–274.
[12] Crowley JS, Friesen TL, Gabriel RA, et al. Speech and audiology outcomes after single-stage versus early 2-stage cleft palate repair. Ann Plast Surg. 2021; 86(5S Suppl 3): S360–S366. https://doi.org/10.1097/SAP.0000000000002747
[13] Kappen I, Yoder WR, Mink van der Molen AB, Breugem CC. Long-term craniofacial morphology in young adults treated for a non-syndromal UCLP: a systematic review. J Plast Reconstr Aesthet Surg. 2018; 71(4): 504–517. https://doi.org/10.1016/j.bjps.2017.12.007
[14] Salgado KR, Wendt AR, Fernandes Fagundes NC, Maia LC, Normando D, Leão PB. Early or delayed palatoplasty in complete unilateral cleft lip and palate patients? A systematic review of the effects on maxillary growth. J Craniomaxillofac Surg. 2019; 47(11): 1690–1698. https://doi.org/10.1016/j.jcms.2019.06.017
[15] Hardwicke JT, Landini G, Richard BM. Fistula incidence after primary cleft palate repair: a systematic review of the literature. Plast Reconstr Surg. 2014; 134(4): 618e–627e. https://doi.org/10.1097/PRS.0000000000000548
[16] Tache A, Mommaerts MY. On the frequency of oronasal fistulation after primary cleft palate repair. Cleft Palate Craniofac J. 2019; 56(10): 1302–1313.
[17] Stein MJ, Zhang Z, Fell M, Mercer N, Malic C. Determining postoperative outcomes after cleft palate repair: a systematic review and meta-analysis. J Plast Reconstr Aesthet Surg. 2019; 72(1): 85–91. https://doi.org/10.1016/j.bjps.2018.08.019
[18] Smarius BJ, Breugem CC. Use of early hard palate closure using a vomer flap in cleft lip and palate patients. J Craniomaxillofac Surg. 2016; 44(8): 912–918. https://doi.org/10.1016/j.jcms.2016.05.011
[19] Syd H. Är en- eller tvåstegsoperation att föredra vid rekonstruktion av gommen för läpp-käk-gomspalt? [Is there a difference in outcome between closing the palate in one or two stages?] Region Skåne. 2022.
[20] O’Connor D, Green S, Higgins JP. Defining the review question and developing criteria for including studies. In: Julian PT Higgins, Sally Green, editors. Cochrane handbook for systematic reviews of interventions. Chichester (UK): John Wiley & Sons Ltd.; 2008. p. 81–94.
[21] Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009; 6(7): e1000097. https://doi.org/10.1371/journal.pmed.1000097
[22] Page MJ, Moher D, Bossuyt PM, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021; 372: n160. https://doi.org/10.1136/bmj.n160
[23] Ouzzani M, Hammady H, Fedorowicz, Z, et al. Rayyan – a web and mobile app for systematic reviews. Syst Rev. 2016; 5(1): 210. https://doi.org/10.1186/s13643-016-0384-4
[24] SBU. Utvärdering av metoder i hälso- och sjukvården: en handbok. 2nd ed. Stockholm: Statens beredning för medicinsk utvärdering; 2014.
[25] Verbeek J, Ruotsalainen J, Hoving JL. Synthesizing study results in a systematic review. Scand J Work Environ Health. 2012; 38(3): 282–290. https://doi.org/10.5271/sjweh.3201
[26] Schünemann H BJ, Guyatt G, Oxman A, editors. GRADE handbook for grading quality of evidence and strength of recommendations. Updated October 2013: The GRADE Working Group; 2013.
[27] Semb G, Enemark H, Friede H, et al. A Scandcleft randomised trials of primary surgery for unilateral cleft lip and palate: 1. Planning and management. J Plast Surg Hand Surg. 2017; 51(1): 2–13. https://doi.org/10.1080/2000656X.2016.1263202
[28] Heliövaara A, Küseler A, Skaare P, et al. Scandcleft randomised trials of primary surgery for unilateral cleft lip and palate: 6. Dental arch relationships in 5 year-olds. J Plast Surg Hand Surg. 2017; 51(1): 52–57. https://doi.org/10.1080/2000656X.2016.1221352
[29] Karsten A, Marcusson A, Rizell S, et al. Scandcleft randomized trials of primary surgery for unilateral cleft lip and palate: occlusion in 8-year-olds according to the Modified Huddart and Bodenham index. Eur J Orthod. 2020; 42(1): 15–23.
[30] Küseler A, Mølsted K, Marcusson A, et al. Scandcleft randomized trials of primary surgery for unilateral cleft lip and palate: maxillary growth at eight years of age. Eur J Orthod. 2020; 42(1): 24–29. https://doi.org/10.1093/ejo/cjz078
[31] Pereira RMR, Siqueira N, Costa E, et al. Unilateral cleft lip and palate surgical protocols and facial growth outcomes. J Craniofac Surg. 2018; 29(6): 1562–1568. https://doi.org/10.1097/SCS.0000000000004810
[32] Mikoya T, Shibukawa T, Susami T, et al. Dental arch relationship outcomes in one- and two-stage palatoplasty for Japanese patients with complete unilateral cleft lip and palate. Cleft Palate Craniofac J. 2015; 52(3): 277–286. https://doi.org/10.1597/13-285
[33] Otsuki K, Yamanishi T, Enomoto A, et al. Maxillary development and dental arch relationships following early two-stage palatoplasty: a comparative study. Cleft Palate Craniofac J. 2022. Published 18th October 2022: 10556656221129751. https://doi.org/10.1177/10556656221129751
[34] Willadsen E, Jørgensen LD, Alaluusua S, et al. Scandcleft randomized trials of primary surgery for unilateral cleft lip and palate: speech proficiency at 10 years of age. Int J Lang Commun Disord. 2022; 58: 892–909. https://doi.org/10.1111/1460-6984.12830
[35] Lohmander A, Persson C, Willadsen E, et al. Scandcleft randomised trials of primary surgery for unilateral cleft lip and palate: 4. Speech outcomes in 5-year-olds – velopharyngeal competency and hypernasality. J Plast Surg Hand Surg. 2017; 51(1): 27–37. https://doi.org/10.1080/2000656X.2016.1254645
[36] Hammarström IL, Nyberg J, Alaluusua S, et al. Scandcleft project trial 2-comparison of speech outcome in 1- and 2-stage palatal closure in 5-year-olds with UCLP. Cleft Palate Craniofac J. 2020; 57(4): 458–469.
[37] Reddy RR, Gosla Reddy S, Chilakalapudi A, et al. Effect of one-stage versus two-stage palatoplasty on hypernasality and fistula formation in children with complete unilateral cleft lip and palate: a randomized controlled trial. Plast Reconstr Surg. 2018; 142(1): 42e–50e. https://doi.org/10.1097/PRS.0000000000004486
[38] Willadsen E, Lohmander A, Persson C, et al. Scandcleft randomised trials of primary surgery for unilateral cleft lip and palate: 5. Speech outcomes in 5-year-olds – consonant proficiency and errors. J Plast Surg Hand Surg. 2017; 51(1): 38–51.
[39] Rautio J, Andersen M, Bolund S, et al. Scandcleft randomised trials of primary surgery for unilateral cleft lip and palate: 2. Surgical results. J Plast Surg Hand Surg. 2017; 51(1): 14–20. https://doi.org/10.1080/2000656X.2016.1254646
[40] Jakobsson OP, Pontén B. Closure of the cleft palate in one or two stages: the surgical methods. Scand J Plast Reconstr Surg Hand Surg. 1990; 24(2): 149–155. https://doi.org/10.3109/02844319009004535
[41] Vedung S. Pharyngeal flaps after one- and two-stage repair of the cleft palate: a 25-year review of 520 patients. Cleft Palate Craniofac J. 1995; 32(3): 206–215; discussion 15–16. https://doi.org/10.1597/1545-1569(1995)032<0206:PFAOAT>2.3.CO;2
[42] Wadde K, Chowdhar A, Venkatakrishnan L, et al. Protocols in the management of cleft lip and palate: a systematic review. J Stomatol Oral Maxillofac Surg. 2022; 124: 1–5. https://doi.org/10.1016/j.jormas.2022.11.014
[43] Mai CT, Isenburg JL, Canfield MA, et al. National population-based estimates for major birth defects, 2010–2014. Birth Defects Res. 2019; 111(18): 1420–1435. https://doi.org/10.1002/bdr2.1589
[44] Calzolari E, Pierini A, Astolfi G, Bianchi F, et al. Associated anomalies in multi-malformed infants with cleft lip and palate: an epidemiologic study of nearly 6 million births in 23 EUROCAT registries. Am J Med Genet A. 2007; 143a(6): 528–537. https://doi.org/10.1002/ajmg.a.31447
[45] Aspelin E, Cornefjord M, Klintö K, et al. Additional diagnoses in children with cleft lip and palate up to five years of age. J Plast Surg Hand Surg. 2023; 57: 1–7. https://doi.org/10.1080/2000656X.2022.2164292
[46] Shaw W, Semb G. The Scandcleft randomised trials of primary surgery for unilateral cleft lip and palate: 11. What next? J Plast Surg Hand Surg. 2017; 51(1): 88–93. https://doi.org/10.1080/2000656X.2016.1254644
[47] Turgoose DP, Kerr S, De Coppi P, et al. Prevalence of traumatic psychological stress reactions in children and parents following paediatric surgery: a systematic review and meta-analysis. BMJ Paediatr Open. 2021; 5(1): e001147. https://doi.org/10.1136/bmjpo-2021-001147
[48] Warlow C. Advanced issues in the design and conduct of randomized clinical trials: the bigger the better? Stat Med. 2002; 21(19): 2797–2805. https://doi.org/10.1002/sim.1283
[49] Langford RJ, Sgouros S, Natarajan K, et al. Maxillary volume growth in childhood. Plast Reconstr Surg. 2003; 111(5): 1591–1597. https://doi.org/10.1097/01.PRS.0000057971.87632.37