ORIGINAL RESEARCH ARTICLE
Single or double Kirschner wire fixation: which provides better outcomes for pediatric proximal phalanx base fractures?
Chan Ju Park, Kyung Jin Lee, Jin Soo Kim, Sung Hoon Koh, Dong Chul Lee, Si Young Roh
Department of Plastic and Reconstructive Surgery, Gwangmyeong Sungae General Hospital, Gwangmyeong, Republic of Korea
ABSTRACT
Purpose: The most common hand fracture in children is seen at the base of the proximal phalanx. This study aims to compare clinical outcomes of single versus double Kirschner wire pinning for pediatric proximal phalanx base fractures.
Patients and Methods: The retrospective study enrolled patients who underwent closed K-wire pinning for proximal phalanx base fractures from January 2016 to February 2022. We divided patients into two groups based on the number of K-wire inserted (single versus double). Demographics, removal of implant, complication rate were analyzed. Patients were asked to answer the Michigan Hand Outcomes Questionnaire (MHQ) by telephone. Data including fracture type, diaphyseal axis-metacarpal head angle (DHA) and Total Active Flexion Scale (TAFS) were analyzed.
Results: This study included 37 pediatric patients with proximal phalanx base fractures, treated with either single (n = 10) or double K-wire (n = 27) fixation. The mean operation time was significantly shorter for the single K-wire group. No significant differences were observed in complication rates, TAFS, implant removal times, MHQ, or pre- and post-operative DHA between the two groups.
Conclusion: The single K-wire technique demonstrates similar effectiveness to the double K-wire technique in treating pediatric proximal phalanx base fractures, with the added benefit of shorter operation time. Therefore, the choice between using one or two K-wires should be determined based on the surgeon’s proficiency and preference.
KEYWORDS: Pediatrics; Kirschner wire; fracture; finger phalanges; fracture fixation.
Citation: Journal of Plastic Surgery and Hand Surgery 2023; 58: 82–88. DOI: https://doi.org/10.2340/jphs.v58.13425.
Copyright: © 2023 The Author(s). Published by MJS Publishing on behalf of Acta Chirurgica Scandinavica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Received: 6 June 2023; Accepted: 1 August 2023. Published: 1 September 2023.
CONTACT Si Young Roh psczero@gmail.com Department of Plastic and Reconstructive Surgery, Gwangmyeong Sungae General Hospital, 36 Digital-ro, Gwangmyeong 14241, Republic of Korea.
Competing interests and funding: The authors declared no potential conflicts of interest with respect to the research, authorship, or publication of this article.
Introduction
The base of the proximal phalanx is a frequent site of fractures in children, as noticed by multiple studies [1,2]. These fractures often fall into three categories: epiphyseal, juxta-epiphyseal, and metaphyseal [3]. They usually involve the small finger, resulting in an abduction deformity known as the extra-octave fracture due to ulnar angulation. Proper management of pediatric proximal phalanx base fractures is of importance, as improper treatment can lead to significant remodeling due to the proximity to the physis and the multiplanar motion of the metacarpophalangeal (MCP) joints [4]. This can result in deformities that impair hand function [5], potentially necessitating surgical intervention [6]. While closed reduction with casting or splinting is often successful, open reduction may be required for displaced fractures with soft tissue involvement or unstable fractures. Various fixation approaches have been documented in previous study [7], with closed reduction and percutaneous pinning (CRPP) being a common treatment for unstable fractures [8]. Al-Qattan et al. [9] demonstrated successful treatment of mildly displaced juxta-epiphyseal fractures using closed reduction and splinting without complications.
The choice regarding the number of K-wires used for pediatric proximal phalanx base fractures is primarily guided by the surgeon’s discretion or the nature of the fracture. Nonetheless, the influence of the number of K-wires on clinical outcomes remains a topic of ongoing uncertainty. This study aims to evaluate and compare the complications and outcomes associated with the treatment of displaced proximal phalanx fractures in children using single versus double K-wire pinning.
Materials and methods
Patients
A single institutional retrospective chart review of all pediatric patients under the age of 16 years old with closed fractures of the base of the proximal phalanx from January 2016 to February 2022 was performed. Inclusion criteria were patients with three types of commonly encountered proximal phalanx base fracture, epiphyseal (the fracture line goes through the growth plate as well as a small metaphyseal fragment at the ulnar or radial corner), juxta-epiphyseal (the fracture line is transverse along the metaphyseal subchondral bone, 1–2 mm distal to the growth plate) and metaphyseal (the fracture line is through the metaphysis distal to the juxta-epiphyseal fracture line), as classified in study by Al-Qattan et al. [3]. Patients who were treated with closed pinning technique with single or double K-wires with complete clinical and radiographic data were included in this study. We excluded patients treated with closed reduction alone or open reduction. Those with open fractures and other associated conditions such as tendon or neurovascular injuries were also excluded (Table 1). The following demographic data were documented: age, sex, laterality, injured finger, mechanism of injury and operation time (Tables 2 and 3). All patients underwent anteroposterior, both oblique and lateral radiographs of both affected and unaffected fingers to assess the type of fracture (epiphyseal, metaphyseal or juxta-epiphyseal) and the amount of displacement on the coronal plane by measuring the diaphyseal axis-metacarpal head angle (DHA). Hand radiographs were obtained during each follow-up appointment. Fractures were considered healed when radiographic evidence showed the fracture line had disappeared and distinct bony trabeculae were visible across the fracture site. Once bone union was determined to be achieved, the K-wire was manually removed in the outpatient clinic, and the splint was taken off.
Surgical method
All surgical procedures were conducted under general endotracheal anesthesia. A pneumatic tourniquet was positioned on the upper arm and inflated following the elevation of the upper limb. In the operating room, the fractures of the proximal phalanx base were reduced and their stability was evaluated. Real-time C-arm fluoroscopy was employed to assist in fracture reduction via manual longitudinal traction and manipulation in all operations.
The affected finger was positioned in the intrinsic-plus position, and two crossed K-wires (sizes: 0.7–1.0 mm) were inserted from the radial and ulnar aspects of the proximal phalanx and drilled into the opposite cortex to achieve bicortical fixation. If cross fixation was not possible, two K-wires were inserted from ulnar side in lateral divergent configuration for adequate stabilization.
In cases where the surgeon opted for the single K-wire pinning method, a retrograde single K-wire was inserted from the ulnar side of the proximal phalanx to stabilize the fracture site. Care was taken to avoid penetrating the articular surface while inserting the K-wires. The pins were left protruding from the skin to facilitate removal during a clinic visit.
Postoperatively, patients were placed in a cast while still in the operating room and admitted for intravenous antibiotic treatment using first-generation cephalosporin, along with daily pin dressings. Following discharge, patients visited the outpatient clinic every 2–3 days for pin dressings, and X-rays were taken once a week. Once bone union was observed in radiograph images, the cast and K-wires were removed at the outpatient clinic. Afterwards, patients were instructed to progressively mobilize the MCP joint as tolerated.
Assessment
Diaphysial axis–metacarpal head angle
The DHA is the angle formed between the longitudinal axis of the proximal phalanx diaphysis and the central point of the metacarpal head. Normal DHA values range from 177.1° to 180.0°. An abnormal value suggests that the fracture displacement requires surgical intervention and may be accompanied by conditions such as finger deviation or scissoring. This angle has been employed in previous study to evaluate fracture displacement at presentation, assess reduction adequacy post-management, and determine the extent of remodeling during follow-up [10].
Two physicians, not involved in the operation, measured the DHA for each finger using antero-posterior view radiographs. All radiographs were accessed through the hospital’s computer system, and measurements were conducted using the ‘angle’ icon on the computer. The researchers placed three points on the screen at the center of the proximal phalanx head, the center of the phalangeal metaphysis base, and the center of the metacarpal head, in that order. The computer calculated the DHA, which was displayed on the screen. Both the initial radiographic image and the most recent follow-up image were used to measure the patient’s DHA. The improvement in DHA was then calculated and subjected to statistical analysis (Figure 1).
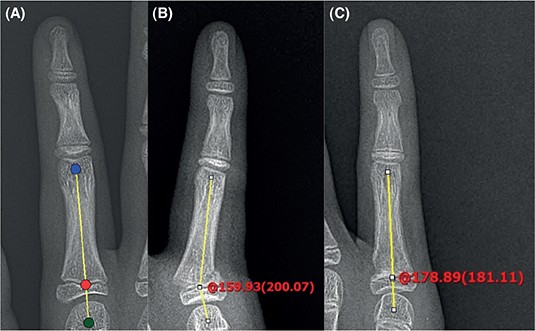
Figure 1. (A) DHA is measured using three points on the plain anteroposterior radiograph. The green circle indicates the center of the metacarpal head. The red circle indicates the center of the base of the phalangeal metaphysis. The blue circle indicates the center of the head of the proximal phalanx. (B) A case with epiphyseal fracture presenting with a preoperative DHA of 159.93° (C) Improved DHA (178.89°) shows successful treatment of proximal phalanx base fracture.
Total Active Flexion Scale
The Total Active Flexion Scale (TAFS), introduced by the American Society for Surgery of the Hand, is a widely utilized anatomical evaluation system [11] . Total active hand motion is calculated by summing the active flexion of the MCP, proximal interphalangeal, and distal interphalangeal joints (subtracting extension deficits of each joint). The resulting scores are classified as good (total: 220°–270°), fair (180°–220°), or poor (<180°) (Table 3). One year after the surgery, patients’ injured hands were assessed for total active range of motion (ROM) using the TAFS during their outpatient clinic visit.
Michigan Hand Outcomes Questionnaire
Patients completed the Michigan Hand Outcomes Questionnaire (MHQ) in the outpatient clinic or by phone one-year post-procedure. The MHQ is a self-reported survey with six scales: (1) overall hand function, (2) daily activities, (3) work performance, (4) pain, (5) aesthetics, and (6) satisfaction. Participants rate items on a 1 (very good) to 5 (very poor) scale [12].
Final scores for each scale are calculated and an overall MHQ score is obtained by dividing the sum of the scores by 6. Ranging from 0 (very poor) to 100 (very good), the MHQ score assesses overall hand performance.
Statistical analysis
The statistical difference was calculated using the Student’s t-test for continuous variables, which followed a normal distribution and Mann–Whitney test for those not following a normal distribution. A p-value of less than 0.05 was taken as significant. Statistical analysis was conducted using IBM SPSS Statistics-Version 26.0 for Windows (IBM Corp., Armonk, NY, USA).
Ethics
This study was performed in accordance with the Declaration of Helsinki. The need for patient consent was waived owing to the study’s retrospective nature, and the study design was approved by the Institutional Review Board of Gwangmyeong Sungae Hospital. (No. KIRB-2023-N-005).
Results
In this study, a total of 37 pediatric patients with proximal phalanx base fractures were treated surgically, 30 (81.1%) males and 7 (18.9%) females. The patients were divided into two groups based on the fixation method: single K-wire (n = 10) and double K-wire (n = 27). The distribution of gender was similar in both groups, with 80.0% males in the single K-wire group and 81.5% males in the double K-wire group. The mean age at the time of injury was 8.7 ± 3.3 years (range, 3 ~ 13) in single K-wire group and 10.2 ± 3.3 years (range, 4 ~ 16) in double K-wire group. The difference in age was not statistically significant (p = 0.2)
The primary mechanisms of injury were falls (n = 17, 45.9%) and sports activities (n = 20, 54.1%). In the single K-wire group, 50.0% of the injuries were due to falls, while in the double K-wire group, 44.4% were attributed to falls. Sports activities accounted for 50.0% of the injuries in the single K-wire group and 55.6% in the double K-wire group.
The right to left ratio of injured hands was 4:6 for the single K-wire group and 11:16 for the double K-wire group. The most commonly injured finger was the little finger, accounting for 90.0% of cases in the single K-wire group and 88.9% in the double K-wire group. Ring finger injuries represented 10.0% of cases in the single K-wire group and 3.7% in the double K-wire group. No middle finger injuries were observed in the single K-wire group, while 7.4% of cases in the double K-wire group involved middle finger injuries.
Regarding the type of fracture, 40.0% were epiphyseal, 50.0% juxta-epiphyseal, and 10.0% meta-epiphyseal in the single K-wire group. In contrast, the double K-wire group had 48.1% epiphyseal, 29.6% juxta-epiphyseal, and 22.2% meta-epiphyseal fractures.
The mean operation time for the single K-wire group was 27.50 ± 8.25 min while the double K-wire group had a longer operation time of 33.74 ± 5.61 min. The difference was statistically significant, with a p-value of 0.012. (Table 4)
In terms of complications, 1 (10%) patient in the single K-wire group experienced malrotation, while 2 (7.4%) patients in the double K-wire group had stiffness. The difference in complication rates between the two groups was not statistically significant.
Regarding the TAFS, the single K-wire group had 10 (100%) patients with good outcomes, while the double K-wire group had 25 (92.6%) patients with good outcomes and 2 (7.4%) patients with fair outcomes. No poor outcomes were observed in either group. The difference in TAFS between the two groups was not statistically significant, with a p-value of 0.38.
All patients achieved bone union of the fracture site. The average time for implant removal was 3.90 weeks in the single K-wire group and 4.06 weeks in the double K-wire group. The difference was not statistically significant, with a p-value of 0.729.
The mean MHQ score for the single K-wire group was 99.7 ± 3.00, while for the double K-wire group, it was 99.74 ± 4.50. There was no significant difference in the MHQ scores between the two groups, with a p-value of 0.8. (Table 5)
The DHA was assessed pre- and post-operatively for both single and double K-wire groups. In the single K-wire group, the pre-operative DHA was 165.93 ± 8.48, and the post-operative DHA improved to 177.07 ± 1.99. This improvement was statistically significant, with a t-value of -5.44 and a p-value of <0.001.
In the double K-wire group, the pre-operative DHA was 163.69 ± 9.17, and the post-operative DHA increased to 177.67 ± 1.75. This change was also statistically significant, with a p-value of <0.001.
When comparing the pre-operative DHAs between the single and double K-wire groups, there was no significant difference (p = 0.484). Similarly, there was no significant difference in the post-operative DHAs between the two groups (p = 0.417). (Table 6)
Case 1
A 7-year-old male patient sustained a juxta-epiphyseal fracture of the base of the proximal phalanx of his right little finger after sports activity. Preoperative radiographs and DHA revealed a significant displacement of 160.70° and a poor TAFS of 90° due to severe pain and swelling. The patient underwent a closed pinning procedure with a single K-wire. The operation time was 15 min. Four weeks postoperatively, bone union was observed, and the implant was removed at the outpatient clinic, allowing the patient to commence self ROM exercises. At the 1-year follow-up, the patient demonstrated significant improvement, with a postoperative DHA of 176.13°, a MHQ score of 100, and a TAFS of 260°, which falls into the ‘good’ category. No complications were reported during the course of treatment and recovery (Figure 2).
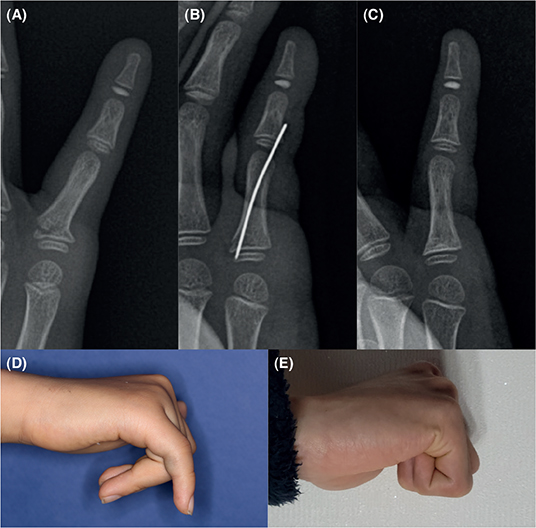
Figure 2. (A) Preoperative X-ray image (B) Postoperative X-ray image (C) Follow-up X-ray image at postoperative 1 year (D) Preoperative range of motion (E) Postoperative range of motion.
Case 2
A 10-year-old male patient presented with an epiphyseal fracture at the base of the proximal phalanx of his right little finger, incurred as a result of a fall down injury. Preoperative radiographic imaging and DHA indicated a displacement of 160.05° and a TAFS of 135°. The patient underwent a closed pinning intervention employing dual Kirschner wires, with the procedure lasting 25 min. Bone union was observed radiographically at 3 weeks postoperation, at the K-wire was removed at this point in the outpatient clinic. The patient initiated self-directed ROM exercises. At the 1-year postoperative follow-up, the patient displayed notable improvements, as evidenced by a DHA of 177.52°, a MHQ score of 100, and a TAFS of 265°, which corresponds to the ‘good’ classification. No complications were reported throughout the treatment and recovery process (Figure 3).
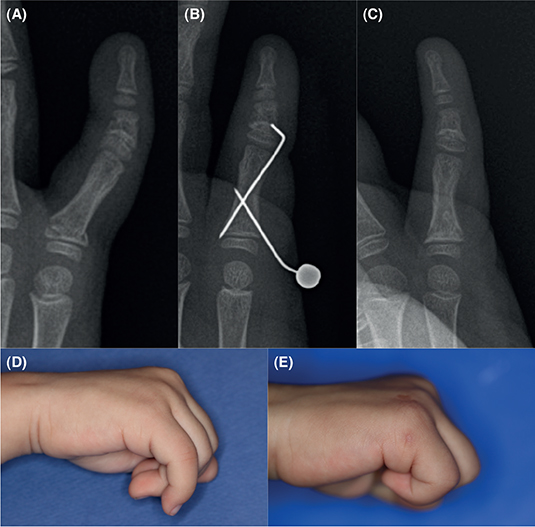
Figure 3. (A) Preoperative X-ray image (B) Post-operative X-ray image (C) Follow-up X-ray image at postoperative 1 year (D) Preoperative range of motion (E) Postoperative range of motion.
Discussion
In this study, we compared the outcomes of two fixation methods for pediatric proximal phalanx base fractures: single K-wire and double K-wire. Our results indicate that both methods provide satisfactory outcomes in terms of functional recovery and patient satisfaction. There were no significant differences in TAFS, MHQ scores, and DHA improvements between the two groups. However, the single K-wire group had a shorter operation time compared with the double K-wire group.
The patient demographics were similar between the two groups, with a higher proportion of males and little finger injuries. This finding is consistent with previous studies on hand injuries, which have reported a higher incidence of hand fractures in males and little finger injuries being the most common [4, 13,14]. The primary mechanisms of injury were falls and sports activities, reflecting the high level of physical activity in the pediatric population [15]. Antero-posterior and true lateral X-rays are pivotal and generally provide precise information for diagnosis of fracture and dislocation [16]. In our study, we conducted serial routine X-rays for all patients, which helped prevent cases of misdiagnosis or delayed diagnosis.
Malone et al. [17] has stated that bone healing may differ depending on the age of the pediatric patient. Their result has shown that children aged between 0 and 1 year exhibit faster healing times in fractures accompanied by the absence of bridging and callus formation compared with children aged between 4 and 5 years. In our study, however, we did not observe a significant age difference between the two groups, and the age difference was not statistically significant. Therefore, it is difficult to interpret that the age difference between the two groups in our study significantly influenced the outcomes. It is worth noting that the age range of the target group in the previous study tends to be lower than that of the patient population in our study. Therefore, for the accurate application of research results, the age groups should be expanded in future studies. This would allow for the inclusion of older children and adolescents in the investigation of the influence of age on bone healing in pediatric fractures.
The shorter operation time in the single K-wire group can be attributed to the simpler surgical procedure, as only one K-wire is used for fixation. This finding is important as shorter operation times during fracture operation have been associated with reduced blood loss, lower infection rates, and faster recovery [18,19]. All surgical procedures were conducted under general endotracheal anesthesia, but local anesthesia can also be encouraged in pediatric patients according to specific surgical settings and organizational models [20,21].
Furthermore, the single K-wire technique can minimize unnecessary radiation exposure during surgery. Due to the closed nature of this study’s surgical procedures, C-arm fluoroscopy was inevitably used, exposing patients to radiation during surgery. The importance of radiation safety during intraoperative use of fluoroscopy has been emphasized in previous study [22]. The single K-wire technique could be beneficial not only for patients but also for surgeons, particularly orthopedic surgeons and operating room staff. Orthopedic surgeons have been shown to have an increased incidence risk of cancer compared with non-exposed workers [23]. Using this surgical method could reduce the total radiation dose, alleviating concerns and potential risks for medical staffs. Additionally, the pediatric patients’ guardians may be more satisfied with the surgery, knowing that the radiation exposure to their child is minimized. It is essential to have thorough discussions with the guardians regarding these matters before the surgery.
One interesting point to note is the role of patient age and bone quality in the choice of fixation method. The patterns of bone formation and joining in pediatric skeleton lead to variations in fracture susceptibility and the healing duration for specific bone areas. Moreover, the enhanced blood supply and specific characteristics of the periosteal layer contribute to a quicker healing process in pediatric bones [24], which may influence the decision to use a single or double K-wire fixation. It cannot be guaranteed that the same results can be obtained in the adult population. Our study did not specifically investigate this factor, and future research may be warranted to explore the impact of patient age and bone quality on the choice of fixation method.
Our results demonstrate no significant differences in TAFS and patient satisfaction (MHQ scores) between the two groups. This finding suggests that both single and double K-wire fixation methods provide satisfactory results in terms of hand function and patient satisfaction.
In terms of complications, the rates were relatively low in both groups, with only one patient experiencing malrotation in the single K-wire group and two patients having stiffness in the double K-wire group. Complications related to K-wire fixation in the hand and wrist are relatively rare, with most issues involving minor, superficial pin track infections [25]. Pediatric proximal phalanx fractures can present complications such as pain, reduced ROM, minor deformity, internal rotation, extensor lag, and premature closure of the growth plate [26]. The low complication rates in our study are encouraging and demonstrate the effectiveness of both fixation methods in managing pediatric proximal phalanx base fractures. The number of K-wires used does not appear to have a significant relationship with the complication rate, so considering this factor may not be necessary.
K-wire removal in the clinic is a common practice, and previous research suggests that removing K-wires in an office setting is safe and acceptable [27]. In our study, all patients underwent manual K-wire removal during outpatient follow-ups after bone union was observed on X-rays. The K-wires were removed using a gentle twist and pull motion with pliers. No issues related to the K-wire removal procedure occurred at our institution, and patient compliance was generally acceptable. Unfortunately, we could not objectively compare these using methods such as Children’s Hospital of Eastern Ontario Pain Scale (CHEOPS) and future research using such objective tools to study the relationship between factors such as pain and the K-wire removal process in our patient population would be beneficial. Using only one K-wire might provide potential benefits in terms of cost and patient satisfaction, as the removal process is shorter and requires less dressing. However, further objective research is needed to confirm this.
Early mobilization is advised for adult phalanx fractures to reduce the risk of stiffness. Immobilizing fingers for more than 3 weeks can result in stiffness, so patients typically begin an early therapy program. However, many adults still experience stiffness post-surgery, as evidenced by a 52% complication rate in a prior study [28]. In contrast, our study showed low complication rates and satisfactory outcomes in pediatric patients, even with 3–4 weeks of immobilization. Notably, our pediatric patients did not participate in a formal rehabilitation program due to the lack of pediatric physical therapy in our clinic and low compliance rate of pediatric population; they self-rehabilitated through manual exercises after pin removal. This indicates that inherent qualities of pediatric bone, such as faster bone healing and higher bone remodeling capacity, contribute to achieving outcomes and stability with just one K-wire that are comparable to those achieved with two K-wires. We attribute this to children’s increased likelihood of avoiding stiffness and adhesions following surgeries [29]. However, physical therapy may still yield better results in pediatric patients, and including it as an independent variable in future research could potentially reveal new findings.
Biomechanical study by Fyfe et al. [30] has revealed that single intramedullary K-wire fixation method for proximal phalanx fracture provided the least stability compared with other fixation methods including double K-wire pinning, intraosseous wiring and oblique K-wire, lateral plating and dorsal plating. However, this study is limited to moistened human cadaveric study. Biomechanical evaluations do not sufficiently examine aspects such as the scope of necessary soft tissue dissection or the potential demand for subsequent hardware extraction [31]. Therefore, it seems that previous studies have not adequately reflected the physiological characteristics of pediatric bones. The result of our comparative study has shown that single K-wire technique achieved high stability, sufficient fixation, and satisfiable ROM in all patients comparable to double K-wire technique. Nevertheless, our comparison was limited to single and double fixation methods, and it appears that further comparisons with other techniques are necessary in the pediatric patient population.
Another limitation of our study is the relatively small number of patients, with the single K-wire group having fewer participants compared with the double K-wire group. As a result, our findings are preliminary, and additional research with extended follow-up periods and larger cohorts is recommended. Moreover, the study’s retrospective nature presented certain limitations. In addition, potential errors and bias may arise from human-scored evaluations, even when using objective assessment tools.
Conclusion
Our study demonstrates that both single and double K-wire fixation techniques yield satisfactory functional outcomes and patient satisfaction in pediatric proximal phalanx base fractures. However, the single K-wire approach offers the benefits of reduced operation time while still providing comparable stability. When selecting the most suitable number of K-wires for treating pediatric patients with proximal phalanx base fractures, surgeons should consider these factors, as well as their own preferences and proficiency.
Acknowledgments
The authors declare that they have no financial interests in any of the products or devices mentioned in this article. No funding source was received for this study. The article processing charge was paid for by the authors. This manuscript has not been published or presented elsewhere in part or in its entirety and is not under consideration by another journal.
ORCID
Si Young Roh  https://orcid.org/0000-0002-8625-6124
https://orcid.org/0000-0002-8625-6124
Chan Ju Park  https://orcid.org/0000-0001-6161-7985
https://orcid.org/0000-0001-6161-7985
Jin Soo Kim  https://orcid.org/0000-0003-3369-2974
https://orcid.org/0000-0003-3369-2974
Sung Hoon Koh  https://orcid.org/0000-0002-8094-2561
https://orcid.org/0000-0002-8094-2561
Dong Chul Lee  https://orcid.org/0000-0003-4211-6901
https://orcid.org/0000-0003-4211-6901
Kyung Jin Lee  https://orcid.org/0000-0002-9448-8291
https://orcid.org/0000-0002-9448-8291
References
[1] Worlock PH, Stower MJ. The incidence and pattern of hand fractures in children. J Hand Surg Br. 1986;11(2):198–200. https://doi.org/10.1016/0266-7681_86_90259-7
[2] Fischer MD, McElfresh EC. Physeal and periphyseal injuries of the hand. Patterns of injury and results of treatment. Hand Clin. 1994;10(2):287–301. https://doi.org/10.1016/S0749-0712(21)01291-9
[3] Al-Qattan MM, Al-Zahrani K, Al-Boukai AA. The relative incidence of fractures at the base of the proximal phalanx of the fingers in children. J Hand Surg Eur. 2008;33(4):465–468. https://doi.org/10.1177/1753193408090146
[4] Cornwall R, Ricchetti ET. Pediatric phalanx fractures: unique challenges and pitfalls. Clin Orthop Relat Res. 2006;445:146–156. https://doi.org/10.1097/01.blo.0000205890.88952.97
[5] Hastings H 2nd, Simmons BP. Hand fractures in children. A statistical analysis. Clin Orthop Relat Res. 1984;188:120–130. https://doi.org/10.1097/00003086-198409000-00015
[6] Büchler U, Gupta A, Ruf S. Corrective osteotomy for post-traumatic malunion of the phalanges in the hand. J Hand Surg Br. 1996;21(1):33–42. https://doi.org/10.1016/S0266-7681(96)80009-X
[7] Page SM, Stern PJ. Complications and range of motion following plate fixation of metacarpal and phalangeal fractures. J Hand Surg Am. 1998;23(5):827–832. https://doi.org/10.1016/S0363-5023(98)80157-3
[8] Karl JW, White NJ, Strauch RJ. Percutaneous reduction and fixation of displaced phalangeal neck fractures in children. J Pediatr Orthop. 2012;32(2):156–161. https://doi.org/10.1097/BPO.0b013e3182423124
[9] Al-Qattan MM. Juxta-epiphyseal fractures of the base of the proximal phalanx of the fingers in children and adolescents. J Hand Surg Br. 2002;27(1):24–30. https://doi.org/10.1054/JHSB.2001.0661
[10] Al-Qattan MM, Al-Motairi MI, Al-Naeem HA. The diaphysial axis-metacarpal head angle in the management of fractures of the base of the proximal phalanx in children. J Hand Surg Eur. 2013;38(9):984–990. https://doi.org/10.1177/1753193413480311
[11] Kleinert HE, Verdan C. Report of the Committee on Tendon Injuries (International Federation of Societies for Surgery of the Hand). J Hand Surg. 1983;8(5 Pt 2):794–798. https://doi.org/10.1016/S0363-5023(83)80275-5
[12] Chung KC, Hamill JB, Walters MR, Hayward RA. The Michigan Hand Outcomes Questionnaire (MHQ): assessment of responsiveness to clinical change. Ann Plast Surg. 1999;42(6):619–622. https://doi.org/10.1097/00000637-199906000-00006
[13] Barton NJ. Fractures of the phalanges of the hand in children. Hand. 1979;11(2):134–143. https://doi.org/10.1016/S0072-968X(79)80025-X
[14] Beatty E, Light TR, Belsole RJ, Ogden JA. Wrist and hand skeletal injuries in children. Hand Clin. 1990;6(4):723–738. https://doi.org/10.1016/S0749-0712(21)01068-4
[15] Battiston B, Letiacciaro A, De leo A. Bedeutung des FESSH Hand Trauma Komitees in Europa. Handchirurgie, Mikrochirurgie, plastische Chirurgie : Organ der Deutschsprachigen Arbeitsgemeinschaft für Handchirurgie : Organ der Deutschsprachigen Arbeitsgemeinschaft für Mikrochirurgie der Peripheren Nerven und Gefässe : Organ der Vereinigung der Deutschen Plastischen Chirurgen. 2013;45:326–331.
[16] Starnoni M, Colzani G, De Santis G, Leti Acciaro A. Management of locked volar radio-ulnar Joint Dislocation. Plast Reconstr Surg Glob Open. 2019;7(10):e2480. https://doi.org/10.1097/GOX.0000000000002480
[17] Malone CA, Sauer NJ, Fenton TW. A radiographic assessment of pediatric fracture healing and time since injury. J Forensic Sci. 2011;56(5):1123–1130. https://doi.org/10.1111/j.1556-4029.2011.01820.x
[18] Xie H, Xie L, Wang J, Chen C, Zhang C, Zheng W. Intramedullary versus extramedullary fixation for the treatment of subtrochanteric fracture: a systematic review and meta-analysis. Int J Surg. 2019;63:43–57. https://doi.org/10.1016/j.ijsu.2019.01.021
[19] Xu R, Ru J, Ji F, et al. Comparison of efficacy, complications and TGF‑β2 expression between DHS and PFNA in elderly patients with osteoporotic femoral intertrochanteric fracture. Exp Ther Med. 2018;16(1):394–399. https://doi.org/10.3892/etm.2018.6177
[20] Leti Acciaro A, Pilla F, Faldini C, Adani R. The carpal tunnel syndrome in children. Musculoskelet Surg. 2018;102(3):261–265. https://doi.org/10.1007/s12306-017-0527-3
[21] Leti Acciaro A, Ramponi L, Adani R. Outpatient paediatric hand surgery: strategy in healthcare implementation and cost-efficient manner. Musculoskelet Surg. 2022;106(4):449–455. https://doi.org/10.1007/s12306-021-00723-w
[22] Kaplan DJ, Patel JN, Liporace FA, Yoon RS. Intraoperative radiation safety in orthopaedics: a review of the ALARA (As low as reasonably achievable) principle. Patient Saf Surg. 2016;10(1):27. https://doi.org/10.1186/s13037-016-0115-8
[23] Mastrangelo G, Fedeli U, Fadda E, Giovanazzi A, Scoizzato L, Saia B. Increased cancer risk among surgeons in an orthopaedic hospital. Occup Med. 2005;55(6):498–500. https://doi.org/10.1093/occmed/kqi048
[24] Ogden JA. Skeletal injury in the child. 3rd ed. New York, NY: Springer-Verlag Inc.; 2000.
[25] Hsu LP, Schwartz EG, Kalainov DM, Chen F, Makowiec RL. Complications of K-wire fixation in procedures involving the hand and wrist. J Hand Surg Am. 2011;36(4):610–616. https://doi.org/10.1016/j.jhsa.2011.01.023
[26] Boyer JS, London DA, Stepan JG, Goldfarb CA. Pediatric proximal phalanx fractures: outcomes and complications after the surgical treatment of displaced fractures. J Pediatr Orthop. 2015;35(3):219–223. https://doi.org/10.1097/BPO.0000000000000253
[27] Sorenson SM, Hennrikus W. Pain during office removal of K-wires from the elbow in children. J Pediatr Orthop. 2015;35(4):341–344. https://doi.org/10.1097/BPO.0000000000000269
[28] Faruqui S, Stern PJ, Kiefhaber TR. Percutaneous pinning of fractures in the proximal third of the proximal phalanx: complications and outcomes. J Hand Surg Am. 2012;37(7):1342–1348. https://doi.org/10.1016/j.jhsa.2012.04.019
[29] Bae DS. Hand, wrist and forearm fractures in children. In: Green DP, Hotchkiss RN, Pederson WC, Wolfe SW, eds. Green’s operative hand surgery. 6th ed. Philadelphia, PA: Elsevier; 2005.
[30] Fyfe IS, Mason S. The mechanical stability of internal fixation of fractured phalanges. Hand. 1979;11(1):50–54. https://doi.org/10.1016/S0072-968X(79)80009-1
[31] Black DM, Mann RJ, Constine RM, Daniels AU. The stability of internal fixation in the proximal phalanx. J Hand Surg Am. 1986;11(5):672–677. https://doi.org/10.1016/S0363-5023(86)80010-7