ORIGINAL RESEARCH ARTICLE
Prevalence of women with breast implants in Sweden: a study based on the population-based mammography screening programme
Emma Hanssona,b, Sarah Zayac, Susanne Meyerb, Alexa Freiin von Wrangelc, Fredrik Wärnbergd,e and Sophia Zackrissonf,g
aDepartment of Plastic Surgery, Institute of Clinical Sciences, The Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden; bRegion Västra Götaland, Sahlgrenska University Hospital, Department of Plastic Surgery, Gothenburg, Sweden; cRegion Västra Götaland, Sahlgrenska University Hospital, Department of Radiology and Mammography, Gothenburg, Sweden; dDepartment of Surgery, Institute of Clinical Sciences, The Sahlgrenska Academy, University of Gothenburg, Göteborg, Sweden; eRegion Västra Götaland, Department of Surgery, Sahlgrenska University Hospital, Göteborg, Sweden; fDepartment of Translational Medicine, Diagnostic Radiology, Lund University, Malmö, Sweden; gDepartment of Medical Imaging and Physiology, Skåne University Hospital, Malmö, Sweden
ABSTRACT
Background: Knowledge about the prevalence of women with breast implants is paramount in calculations of risks and in estimations of effects on screening and breast cancer treatment. Most of the estimations of prevalence made to date are rough and often based on sales data. The main aim of this study was to calculate the prevalence of breast implants in Swedish women. The secondary aim was to investigate if it is feasible to establish the occurrence of breast implants with the help of the public mammography screening programme, in a country with a publicly funded welfare-type healthcare system and with a clear documentation of screening.
Methods: Information on implants was prospectively collected from all screening attendants from 1st of February 2022 to 1st of August 2022 based on a question from the radiographer to the woman and later verified on the mammogram.
Results: During the study period 4,639 women were screened, of which 182 had implants (3.9%). The frequency varies between 1.6 and 6.4% in different age groups.
Conclusion: The prevalence of breast implants in Swedish women is estimated to be around 4%. The population-based mammography screening programme in countries with a publicly funded welfare-type healthcare system and a clear documentation of mammography screening attendance, seems to be a feasible way to establish the prevalence of breast implants in the population. The large number of women with breast implants warrants further studies regarding the best diagnostic and treatment alternatives for this group.
Pre-registration: ClinicalTrials.Gov identifier NCT05222100.
KEYWORDS: Breast implant prevalence; mammography; plastic surgery
Citation: Journal of Plastic Surgery and Hand Surgery 2023; 58: 96–100. DOI: https://doi.org/10.2340/jphs.v58.15298.
Copyright: © 2023 The Author(s). Published by MJS Publishing on behalf of Acta Chirurgica Scandinavica. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material, with the condition of proper attribution to the original work.
Received: 19 June 2023; Accepted: 17 August 2023; Published: 20 September 2023.
CONTACT Emma Hansson emma.hansson.2@gu.se Department of Plastic Surgery, Sahlgrenska University Hospital, Gröna Stråket 8, SE-413 45 Gothenburg, Sweden.
Competing interests and funding: The authors report no conflicts of interest.
The study was funded by grants from the Swedish Cancer Society [210279 SCIA] and the federal government under the ALF agreement [ALFGBG-965161]. The sources of funding had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Introduction
Knowledge about the prevalence of women with breast implants is paramount in calculations of risks of breast implant-related disease, such as breast implant associated anaplastic large cell lymphoma (BIA-ALCL) [1], as well as in estimations of effects on mammography screening and on breast cancer treatment, in terms of best choice of methods, development of techniques, and costs [2,3]. Breast augmentation is one of the most common cosmetic operations performed [4] and implants are also used to reconstruct breasts after cancer, resulting in an implantation frequency of more than 450,000 devices a year in North America alone [5].
Most of the estimations of prevalence of implants made to date are rough and often based on sales data. During the last decade, a number of national implant registries, for example in the Netherlands (DBIR), Australia (ABDR), the UK (BCIR), USA (NBIR), and Sweden (BRIMP), have been established, which will facilitate prevalence calculations. However, the robustness of the data of the registries is affected by factors such as incompleteness of records and lack of reporting, unregulated cosmetic markets in many countries, and cosmetic tourism [1]. Moreover, it takes many years to establish reliable prevalence numbers based on the registries as the popularity of breast augmentation is likely to have fluctuated over time and therefore incidence numbers cannot be used to calculate prevalence.
A suggested method to establish prevalence of breast implants is radiologic estimates based on available x-rays [1]. Two recent studies, performed in the Netherlands [6] and in Italy [7], respectively, used available chest radiographs, performed for example due to pulmonary and cardiac conditions, suspicion of pneumonia, screening for tuberculosis, pre- and post-operative assessments, trauma, autoimmune diseases, and malignancies, to examine the presence of implants [6,7] (Table 1). The two studies found a sensitivity of 57 to 96% and specificity of 82 to 98%, as sometimes only indirect radiological signs of the presence of an implant can be used [6,7]. Other than an unperfect sensitivity and specificity there is a risk of bias due to a possibly unrepresentative sample [6]. Moreover, there are two previous studied reporting prevalence of implants based on screening mammography populations (Table 1) [8,9]. One was performed in California, USA [9], where it is recommended that women between 50 and 74 years of age attend mammography screening, but it is not accessible to all due to sociodemographic and geographical barriers [10–12]. The other was performed in Norway [8] based on national registry data, but it is not stated how the presence of implants was established.
| Study | Kam, 2015, USA [9] | De Boer, 2020, The Netherlands [6] | Sondén, 2020, Norway [9] | Santanelli, 2023, Italy [7] | Swedish study (present study) |
| Number of included women | 1,863 | 3,050 | 785,706 | 3,537 | 4,639 |
| Female population of the country (according to https://www.worldometers.info/world-population/world-population-gender-age.php accessed 17.03.2023, figures from 2013) | 167.5 million | 8.5 million | 2.5 million | 8.7 million | 4.8 million |
| Period of inclusion | 01.03.2013–30.10.2013 | 01.2015–12.2015 | 2006–2016 | 01.01.2019–31.12.2019 | 01.02.2022–01.08.2022 |
| Place of inclusion | Loma Linda, California Loma Linda University Medical Centre |
Enschede, Overijssel and Maastricht, Limburg Medical spectrum Twente Hospital and Maastricht University Medical Centre |
Norway. All screening mammographies are registered in a national registry (Kreftregisteret www.kreftregisteret.no/screeningprogrammene/ ) |
Rome, Lazio Sant’Andrea Hospital |
Gothenburg, Västra Götaland Sahlgrenska University Hospital |
| Base of study | Women undergoing mammography screening | Chest X-rays | Population based screening mammography | Chest X-rays | Population based screening mammography |
| Sensitivity | Not reported | 72% (range 42–85%) | Not reported | Median 87% (range 57–96%) | >99% |
| Specificity | Not reported | 95% (range 73–98%) | Not reported | Median 97% (range 90–98%) | >99% |
| Risk of bias |
|
|
|
|
A direct measurement of ratio of women with breast implants participating in the screening mammography programme has never been performed in a country with a publicly funded welfare-type healthcare system, with a strong emphasis on equal access to healthcare and a population-based screening programme with a high attendance rate. We hypothesise that in such a system direct registration of occurrence of implants in the screened population can be used to estimate the national prevalence of breast implants.
The main aim of this study was to calculate the prevalence of breast implants in Swedish women. The secondary aim was to investigate if it is feasible to establish the occurrence of breast implants with the help of the public mammography screening programme, in a country with a publicly funded welfare-type healthcare system and with a clear documentation of mammography screening.
Patients and methods
Study design, protocol, and ethics
This is a cross-sectional observational study. It is one of the studies described in the ‘Effect of Breast Implants on Mammography Screening’ protocol (ClinicalTrials.Gov identifier NCT05222100). The Swedish Ethical Review Authority reviewed and approved the study (2021-01534). The authority decided that there was no need for informed consent from the women. The study is reported according to the STROBE guidelines [13].
Setting
Sweden has a population-based mammography screening programme for women aged 40 to 74 years, recommended since 1985 and fully implemented since 1997 [14, 15]. Attendance in the screening programme is free, without out-of-pocket fees [16]. The study was performed in Sahlgrenska University Hospital, Gothenburg, in Region Västra Götaland, where the screening attendance is about 84% [17] and where approximately 10,000 women are screened every year. According to the Swedish breast implant registry (BRIMP), 9,936 breast implants were implanted in Region Västra Götaland between 2014 and 2021, ranging from 929 to 1,317 per year (data extraction made 09 February 2022 by Bröstimplantatregistret (BRIMP), Centre of Registers Västra Götaland, SE-413 45 Gothenburg). The majority of breast augmentations in Sweden are performed in private healthcare.
Participants, data collection and variables
The Picture Archive and Communications System (PACS) Sectra IDS7 and the Radiology Information Systems & Picture Archiving & Communications System (RIS-PACS) (Sectra AB, Linköping, Sweden) were used to prospectively collect information from all screening attendants from 1st of February 2022 to 1st of August 2022. The registration was made in the PACS just before the digital screening mammogram was acquired, based on a question from the radiographer to the woman, and later verified on the mammogram by the radiographer. Two cohorts were created: implant and no implant. Data on number of screened women with and without breast implants were extracted from the PACS on group level without personal data, to ensure the participants’ anonymity. A consecutive cohort of 6 months of participants in the population-based mammography screening programme was estimated to be sufficient to eliminate the risk of recruiting a skewed population as regards age and sociodemographic factors.
Results
During the study period 4,639 women were screened, of which 182 had implants (3.9%). The number of women screened with and without implants are given in Figure 1. The frequency varies between 1.6 % and 6.4% in different age groups (Figure 1). The highest frequency was found in the women aged 40–45 and the lowest in women over 70 (Figure 1). A comparison between this study and other studies using radiologic estimates to calculate prevalence is given in Table 2.
| North American prevalence [9] Loma Linda, California | Dutch prevalence [6] Twente, Maastricht (reported separately) | Norwegian prevalence [9] National registry (Kreftregisteret https://www.kreftregisteret.no ) | Italian prevalence [7] Rome | Swedish prevalence (present study) Gothenburg | |
| Total prevalence (years) | 4.8% (90/1,863) | 2.8% (84/3,050) | 1.3% (10,086/786,529) | 4.0% (140/3,537) | 3.9% (182/4,639) |
| 20–30 | - | 1.0%, 2.3% | - | 2.1% | - |
| 31–40 | - | 3.6%, 3.6% | - | 4.4% | - |
| 41–50 | - | 3.3%, 3.9% | - | 5.2% | 5.5% |
| 51–60 | - | 3.0%, 3.3% | - | 4.9% | 3.9% |
| 61–70 | - | 1.6%, 2.0% | - | 2.9% | 1.8% |
| 71–74 | - | - | - | - | 1.6% |
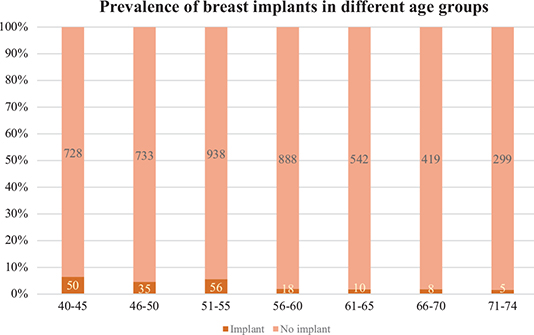
Figure 1. Frequency of breast implants in different age groups participating in the population-based mammography screening.
Discussion
This is the first study measuring the prevalence of women with breast implants that is based on direct measurements in a population-based mammography screening in a country with a publicly funded welfare-type healthcare system. It indicates that the prevalence of breast implants in the population is around 4%. The prevalence is similar to the prevalence previously found in existing chest x-rays in Italy [7] and slightly higher than that found in the Netherlands [6] (Table 2); whereas, it is slightly lower than that found in the screening mammography in California [9] and considerably higher than that found in Norway [8] (Table 2).
A strength of the present study is that the data were generated directly from women attending the screening programme. The data were created both by asking the women before the examination and confirmed on the mammograms by the radiographer. The women were advised that information on implants is necessary to enable correct mammogram projections. The information from the women in combination with the possibility to confirm on mammograms gave an almost perfect sensitivitiy and specificity. The only source of error could be that the mammographer accidently registered the wrong information in Sectra and that physician evaluating the mammogram missed correcting it. The risk of this happening in more than very sporadic cases is evaluated as very low. Therefore, the sensitivity and specificity, and thereby the accuracy of data, have to be considered higher in this study than in studies based on existing chest x-rays, were sensitivities of 42–96% (median 76 and 87%) and specificities of 73–98% (median 95 and 97%) have been reported [6, 7] (Table 1).
Nonetheless, there are several weaknesses with the usage of the screening mammography to estimate the prevalence of breast implants in the general population, the major one being risk of an unrepresentative sample. Factors that might affect the representativeness include variation in attendance in different sociodemographic groups [17], the geographical location of where the study was performed [6], that women under 40 and over 74 years of age are not screened [15], and that breasts operated on with a mastectomy, and possibly implant-based reconstruction, are excluded from the screening programme [18].
In Västra Götaland, the attendance in the screening programme is 84% [17]. However, there are differences between the women attending and those who are not as the women not attending are more likely to live without a partner, have a low income, be a non-nordic woman born outside Scandinavia, living on social assistance or benefits, not own a home or have a low level of education. Women who have several of these sociodemographic characteristics are more unlikely to attend [17]. The differences between participating and non-participating women might have affected the prevalence of breast implants as these factors may also influence the choice to have a breast augmentation [19]. Moreover, the authors of the Dutch prevalence study, stated that although the attendance rate of the screening programme is 80% in the Netherlands, the prevalence of implants cannot be calculated directly from it as women with implanted medical devices attend mammography less than women without devices [6]. The hypothesis is that women with implants have a lower attendance as they have a fear that the mammography might damage the implant or make the examination more difficult [6]. However, the assumption is based on a study on women with implantable cardioverter defibrillators, pacemakers, heart rhythm monitors, or port-a-caths [20], and the transferability to women with breast implants can be questioned. In summary, it is unknown if there is a difference in screening attendance between women with and without implants in Sweden, but if the Dutch hypothesis [6] is valid and if women with certain sociodemographic characteristics have a lower attendance [17] it could be an indication that our prevalence numbers are falsely low.
This study was conducted in an urban region, which might have affected the prevalence, as was illustrated in the Dutch study [6]. However, it is difficult to predict how, as registrations in the Swedish breast implant registry are based on location of the operating clinic, not the patient’s place of residence. More cosmetic clinics are located in urban areas and therefore they also serve the majority of the urban population. The lack of registration of the patient’s place of residence in the implant registry makes it impossible to know if the prevalence of breast implants is higher or lower in rural regions than in urban regions in Sweden. Nevertheless, data from the Swedish Breast Implant Registry (BRIMP) have indicated that there are clear geographic differences in breast implant surgery in Sweden and that the incidence is higher in the regions where the two biggest cities, Stockholm and Gothenburg, are located [21]. Therefore, we do not know if the location of this study has affected the prevalence of implants, which is a clear study weakness.
The population-based screening programme does not include women under 40 and over 74 years of age. According to Swedish implant registry data, most primary augmentations are indeed performed in women aged 21–40 [22]. This is accordance with data from the Dutch registry, were about 70% of the operated patients were under the age of 40 [23]. However, although the implant incidence is higher in patients under 40, the prevalence is accumulating and should therefore not be higher in the group under 40 than in the group over 40, if the practice of breast augmentation is reasonably stable over the years. Looking at North American statistics, 212,500 women having augmentation were reported in 2000 and 193,075 in 2020, indicating a relative stability [4]. In the studies based on chest x-rays, the prevalence was 1–2% in women aged 20 to 30 years and 3.3–5.2% in women aged 41 to 50 years. Based on this, the Swedish prevalence in women under the age of 40 should be lower than the 6.8% found in women aged 40–45 years (Figure 1). However, the lack of data for women under the age of 40 years might have resulted in a falsely low overall prevalence as older women (>61 years), who were 20–40 years old before breast augmentation became commonplace, were included (Table 2).
Many women with breast implants because of breast cancer might have been missed in the current prevalence estimation as breasts operated on with a mastectomy due to cancer or an increased risk of breast cancer is excluded from the population-based screening programme [18]. This implies that a group of women who often have breast implants, are excluded from our population, which might have given a falsely low prevalence.
In brief, prevalence calculations estimated on population-based mammography screening are not perfect, as they have weakness regarding sample representativeness. However, compared with samples based on existing chest x-rays we know more about how the sample might be biased when screening mammography is used. Moreover, the sensitivity and specificity of detecting breast implants in connection with screening mammography far exceeds that of using indirect signs on chest x-rays. Therefore, we conclude that direct registration of occurrence of implants in connection with screening mammography is a feasible way to generate a fairly accurate breast implants prevalence in different regions and countries.
Our results demonstrate that a not significant number of women have breast implants, which have different clinical implications. If 3.9% of the Swedish female population truly have breast implants, there are 187,200 women with implants in Sweden alone. If the average number were true for the entire European Union, there would be about 9 million women with breast implants (229 million women1 × 3.9%) in the region. The number of affected women warrants more studies on the exact prevalence in different regions to calculate risk of implant-based disease, as well as of other effects of implants. For example, if women with breast implants should be screened with a different protocol, inlcluding more projections [2, 24], than women without implants, if breast implants affect the attendance of mammography screening [20], and if breast cancer surgery needs to be developed tor women who have implants, and want to keep their implants post-treatment.
Conclusion
The prevalence of breast implants in Swedish women is estimated to be around 4%. The population-based mammography screening programme in countries with a publicly funded welfare-type healthcare system and a clear documentation of mammography screening attendance, seems to be a feasible way to establish the prevalence of breast implants in the population.
Acknowledgements
We are grateful to the Centre of Registers Västra Götaland: Rebecka Bertilsson, Peter Gidlund, and Martin Halle, for data extractions from the Swedish breast implant registry (Bröstimplantatregistret -BRIMP, https://brimp.registercentrum.se).
ORCIDs
Emma Hansson  https://orcid.org/0000-0002-3218-0881
https://orcid.org/0000-0002-3218-0881
Fredrik Wärnberg  https://orcid.org/0000-0002-6274-2435
https://orcid.org/0000-0002-6274-2435
Sophia Zackrisson  https://orcid.org/0000-0001-5678-3882
https://orcid.org/0000-0001-5678-3882
References
[1] Collett DJ, Rakhorst H, Lennox P, et al. Current risk estimate of breast implant-associated anaplastic large cell lymphoma in textured breast implants. Plast Reconstr Surg. 2019; 143(3S A Review of Breast Implant-Associated Anaplastic Large Cell Lymphoma): 30S–40S. https://doi.org/10.1097/PRS.0000000000005567
[2] Miglioretti DL, Rutter CM, Geller BM, et al. Effect of breast augmentation on the accuracy of mammography and cancer characteristics. JAMA. 2004; 291(4): 442–450. https://doi.org/10.1001/jama.291.4.442
[3] Tang SS, Gui GP. A review of the oncologic and surgical management of breast cancer in the augmented breast: diagnostic, surgical and surveillance challenges. Ann Surg Oncol. 2011; 18(8): 2173–2181. https://doi.org/10.1245/s10434-011-1578-6
[4] American Society of Plastic Surgeons. Plastic surgery statistics report. ASPS National Clearinghouse of Plastic Surgery Procedural Statistics. 2020. Available from: https://www.plasticsurgery.org/documents/News/Statistics/2020/plastic-surgery-statistics-full-report-2020.pdf
[5] Cosmetic Surgery National Data Bank Statistics. Aesthet Surg J. 2018; 38: 1–24. https://doi.org/10.1093/asj/sjy132
[6] de Boer M, van Middelkoop M, Hauptmann M, et al. Breast implant prevalence in the Dutch female population assessed by chest radiographs. Aesthet Surg J. 2020; 40(2): 156–164. https://doi.org/10.1093/asj/sjz136
[7] Santanelli di Pompeo F, Firmani G, Paolini G, et al. Determining breast implant prevalence: a population study of Italian chest radiographs. Aesthetic Plast Surg. 2023; 47: 957–965. https://doi.org/10.1007/s00266-023-03290-6
[8] Sonden ECB, Sebuodegard S, Korvald C, et al. [Cosmetic breast implants and breast cancer]. Tidsskr Nor Laegeforen. 2020; 140(3). https://doi.org/10.4045/tidsskr.19.0266
[9] Kam K, Lee E, Pairawan S, et al. The effect of breast implants on mammogram outcomes. Am Surg. 2015; 81(10): 1053–1056. https://doi.org/10.1177/000313481508101028
[10] Kim E, Moy L, Gao Y, et al. City patterns of screening mammography uptake and disparity across the United States. Radiology. 2019; 293(1): 151–157. https://doi.org/10.1148/radiol.2019190647
[11] Heller SL, Rosenkrantz AB, Gao Y, et al. County-level factors predicting low uptake of screening mammography. AJR Am J Roentgenol. 2018; 211(3): 624–629. https://doi.org/10.2214/AJR.18.19541
[12] Schueler KM, Chu PW, Smith-Bindman R. Factors associated with mammography utilization: a systematic quantitative review of the literature. J Womens Health (Larchmt). 2008; 17(9): 1477–1498. https://doi.org/10.1089/jwh.2007.0603
[13] von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007; 370(9596): 1453–1457. https://doi.org/10.1016/S0140-6736(07)61602-X
[14] Olsson S, Andersson I, Karlberg I, et al. Implementation of service screening with mammography in Sweden: from pilot study to nationwide programme. J Med Screen. 2000; 7(1): 14–18. https://doi.org/10.1136/jms.7.1.14
[15] Socialstyrelsen, editor. Screening för bröstcancer. Rekommendation och bedömningsunderlag. Stockholm: Socialstyrelsen; 2015.
[16] Lagerlund M, Akesson A, Zackrisson S. Change in mammography screening attendance after removing the out-of-pocket fee: a population-based study in Sweden (2014–2018). Cancer Causes Control. 2021; 32(11): 1257–1268. https://doi.org/10.1007/s10552-021-01476-4
[17] Lagerlund M, Akesson A, Zackrisson S. Population-based mammography screening attendance in Sweden 2017–2018: a cross-sectional register study to assess the impact of sociodemographic factors. Breast. 2021; 59: 16–26. https://doi.org/10.1016/j.breast.2021.05.011
[18] Swedish Confederation of Regional Cancer Centres. National guidelines for breast cancer [Nationellt vårdprogram bröstcancer] [Internet]. Stockholm; 2020. [Cited: 9th of August 2023] Available from: https://kunskapsbanken.cancercentrum.se/diagnoser/brostcancer/vardprogram/
[19] von Soest T, Torgersen L, Kvalem IL. Mental health and psychosocial characteristics of breast augmentation patients. J Health Psychol. 2020; 25(9): 1270–1284. https://doi.org/10.1177/1359105318754645
[20] Paap E, Witjes M, van Landsveld-Verhoeven C, et al. Mammography in females with an implanted medical device: impact on image quality, pain and anxiety. Br J Radiol. 2016; 89(1066): 20160142. https://doi.org/10.1259/bjr.20160142
[21] Swedish Breast Implant Registry (BRIMP). Annual report 2021. [BRIMP – Bröstimplantatregistret Årsrapport 2021] [Internet]. Centre of Registers Västra Götaland. Gothenburg. 2022. [ Cited: 9th of August 2023] Available from: https://registercentrum.blob.core.windows.net/brimp/r/BRIMP_annual-report-2021-SkeNVyrX1h.pdf
[22] Swedish Breast Implant Registry (BRIMP). Annual report 2019. [BRIMP – Bröstimplantatregistret Årsrapport 2019] [Internet]. Centre of Registers Västra Götaland. Gothenburg; 2020. Available from: https://registercentrum.blob.core.windows.net/brimp/r/BRIMP-Annual-Report-2019-HJeBIdtlJP.pdf
[23] Spronk PER, Becherer BE, Hommes J, et al. How to improve patient safety and quality of care in breast implant surgery? First outcomes from the Dutch Breast Implant Registry (2015–2017). J Plast Reconstr Aesthet Surg. 2019; 72(10): 1607–1615. https://doi.org/10.1016/j.bjps.2019.06.023
[24] Sa Dos Reis C, Gremion I, Richli Meystre N. Study of breast implants mammography examinations for identification of suitable image quality criteria. Insights Imaging. 2020; 11(1): 3. https://doi.org/10.1186/s13244-019-0816-5
[25] Larsen M, Moshina N, Sagstad S, et al. Factors associated with attendance and attendance patterns in a population-based mammographic screening program. J Med Screen. 2021; 28(2): 169–176. https://doi.org/10.1177/0969141320932945
Footnote
1https://ec.europa.eu/eurostat/cache/digpub/demography/bloc-1b.html?lang=en Accessed 17.03.2013