ORIGINAL RESEARCH ARTICLE
Normative BREAST-Q reconstruction scores for satisfaction and well-being of the breasts and potential donor sites: what are Swedish women of the general population satisfied/dissatisfied with?
Christian Jepsena,b, Anna Paganinia,b,c, Emma Hanssona,b
aInstitute of Clinical Sciences, Department of Plastic Surgery, The Sahlgrenska Academy, Gothenburg University, Gothenburg, Sweden; bDepartment of Plastic and Reconstructive Surgery, Sahlgrenska University Hospital, Gothenburg, Sweden; cInstitute of Health and Care Sciences, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden
ABSTRACT
Background: Normative data for interpreting the BREAST-Q reconstruction module are currently limited to four populations. The primary aim of this study was to create Swedish normative values for the BREAST-Q reconstruction domains. The secondary aim was to describe what aspects of the breasts and potential donor sites that women of the general population are generally satisfied or dissatisfied with.
Methods: The BREAST-Q reconstruction module was sent to a random sample of 400 women currently living in Region Västra Götaland. Descriptive data are presented.
Results: One hundred and forty-six women answered the questionnaire (36.5%). The mean age of the cohort was 53 years, and the mean body mass index (BMI) was 25 kg/m2. Mean total scores ranged from 50 to 90. The mean score for satisfaction with breast was 57 on a 0–100 scale. Women with high BMI values seem to be less satisfied with their breasts and physical and sexual well-being. The participants were most satisfied with their breasts when clothed. Overall, the reported physical well-being related to potential donor sites was high.
Conclusions: Normative data for BREAST-Q constitute a reference point, which allows us to put another perspective on changes in scores rather than just comparing scores before and after surgery. Scores were somewhat different than scores in previously published normative populations, which indicates that there might be cultural differences in breast satisfaction.
KEYWORDS: BREAST-Q; patient-reported outcomes; PROM; quality of life; breast reconstruction; plastic surgery; normative values; breast satisfaction.
Citation: Journal of Plastic Surgery and Hand Surgery 2023; 58: 124–131 DOI: https://doi.org/10.2340/jphs.v58.15301.
Copyright: © 2023 The Author(s). Published by MJS Publishing on behalf of Acta Chirurgica Scandinavica. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material, with the condition of proper attribution to the original work.
Received: 20 June 2023; Accepted: 17 August 2023; Published: 15 November 2023
CONTACT Christian Jepsen Christian.jepsen@gu.se Department of Plastic Surgery, Sahlgrenska University Hospital, Gröna Stråket 8, SE-413 45 Gothenburg, Sweden
Competing interests and funding: The authors have no competing interests to disclose.
This study was funded by grants from The Swedish Cancer Society [21 0279 SCIA], the federal government under the ALF agreement [ALFGBG-724171 and ALFGBG-965161], The Percy Falk Foundation, Stockholm, Sweden, for research into prostate cancer and breast cancer, and The Swedish Breast Cancer Association. The funding sources had no role in the design, conduct, analysis, and reporting of the study.
Introduction
The main purpose of breast reconstruction is to increase the patient’s quality of life, and core outcomes include the woman’s experience of normality, quality of life, cosmetic satisfaction, self-esteem, emotional well-being, and physical well-being, in addition to more hard endpoints, such as complications and unplanned surgery [1]. There are three robustly validated patient-reported outcome measurement instruments (PROMs) for breast reconstruction [2], containing elements of the above-mentioned outcomes. BREAST-Q is the most widely used of them [3]. However, for the measurements of PROMs in breast reconstruction to become meaningful and interpretable, and to allow for comparison of different methods, normative values are essential [4]. Normative values are a complement to individual preoperative and postoperative data and enable us to better understand the impact of breast cancer and breast reconstruction on breast-related quality of life. Thus far, four normative populations have been described for BREAST-Q: two North-America [5,6], one Australian [7], and one Dutch [8]. Significant differences have been found between the populations, indicating that there could be cultural variations between populations, and that normative values relevant for different cultural settings and populations are required.
In women, cosmetic breast operations, such as breast augmentation, reduction, and mastopexy, and operations of the abdomen, such as abdominoplasty and liposuction, are among the top esthetic procedures [9]. This indicates that the breasts and potential donor sites in breast reconstruction might be areas of the body that many women are dissatisfied with. Nonetheless, little is known about what aspects of the breasts and potential donor sites that women are generally satisfied or dissatisfied with. Knowledge about this could prove useful when a reconstructive method following breast cancer is chosen.
The primary aim of this study was to create Swedish normative values for the BREAST-Q reconstruction domains. The secondary aim was to describe what aspects of the breasts and potential donor sites that women of the general population are generally satisfied or dissatisfied with.
Participants and methods
Study design, protocol, and ethics
This is a prospective observational cross-sectional study described in the ‘Reconstruction with back donor site flaps study and validation of quality-of-life scales’ protocol (ClinicalTrials.Gov identifier NCT04526561). The participants have previously been included in a study on Swedish normative value for BREAST-Q reduction/mastopexy [10].
This study was vetted and approved by the Regional Ethical Committee of Gothenburg (254-18) and conducted in accordance with the Helsinki Declaration and the Good Clinical Practice (GCP) guidelines. All participants gave their informed consent to participations and to publication of the results.
Setting, participants, and data collection
This study was conducted in Region Västra Götaland, with about 1.7 million inhabitants and Gothenburg as a capital city. Statens personadressregister, SPAR, which includes all residents in Sweden, made a random selection of 400 women aged 18–80 in the region. The patients were sent an envelope including information about the study, the questionnaire, and a stamped reply envelope. The only exclusion criterion was the inability to understand Swedish. Two reminders were sent after 4 and 8 weeks if the participant had not returned the questionnaire. The participants were asked to mention their age, weight, and height and to answer the BREAST-Q modules described in the next section.
BREAST-Q
The items and domains of BREAST-Q reconstruction were developed in North America with qualitative technique [11] and have been validated [12,13] and translated to Swedish. The BREAST-Q reconstruction version 1 comprises the following preoperative domains: Satisfaction with breasts (4 items), Psychosocial well-being (10 items), Physical well-being chest (16 items), Sexual well-being (6 items), Physical well-being abdomen (5 items), Satisfaction with abdomen (1 item), and Physical well-being back and shoulder (11 items). Using the preoperative questionnaire enables us to evaluate satisfaction with potential donor sites of operated women. Every item is rated from 1 to 3, 4, or 5 on a Likert scale [14]. In 2017, the Breast-Q Version 2.0 was published with some minor modifications in all domains except ‘Physical well-being chest’, where more significant changes were made [15]. For the Physical well-being domain, six questions were removed, and response options were reduced from 5 to 3. In both versions, a raw scale summed score is calculated for each domain, except ‘Satisfaction with abdomen’, thereafter transformed to Rasch logits, and finally to a standardized score between 0 and 100. A higher score indicates a better outcome/higher satisfaction [14,15]. In this study, version 1 of BREAST-Q was sent to the participants. For the domain ‘Physical well-being’, scores for both version 1.0 and 2.0 were calculated to create normative data for both versions. To calculate version 2 scores, the items only occurring in version 1.0 were removed, and response options 1 and 2 were merged to 1, 3 changed to 2, and 4 and 5 merged to 3. The use of BREAST-Q, authored by Drs. Klassen, Pusic, and Cano, was made under license from Memorial Sloan Kettering Cancer Center, New York, USA.
Statistics
QScoreTM was used to calculate summary scores for version 1.0: Satisfaction with breasts, Psychosocial well-being, Physical well-being chest, Sexual well-being, and Physical well-being abdomen. For version 2.0 Physical well-being, a summary score was calculated as described in the user manual [15]. Missing values were treated according to the instructions in the BREAST-Q manual [14]. The conversion table from sum scores to equivalent Rasch transformed scores, provided by authors of BREAST-Q, was used to calculate standardized scores for Physical well-being back and shoulder. Summary scores were considered continuous variables and presented as medians and ranges, and mean and standard deviations (SDs). Item scores were considered categorical variables and were presented as frequencies. Data were sub-analyzed into different age and body mass index (BMI) categories, as previously performed for the North American [6] and the Australian [7] normative dataset. Statistical analyses were preformed using Microsoft Excel® for Microsoft 365 MSO version 2208 and SPSS® version 27.0.0.0 for Mac (IBM, Armonk, New York, USA).
Results
From December 2021 to March 2022, 146 women answered the questionnaire, giving a response rate of 36.5% (146/400). All 146 participants answered the domains: Satisfaction with breasts, Psychosocial well-being, and Physical well-being chest, abdomen, and back and shoulder, 145 answered the domain Satisfaction with abdomen, and 134 participants answered the Sexual well-being domain.
The mean age of the cohort was 53 years (SD 16), and the mean BMI was 25 kg/m2 (SD 4). Mean total BREAST-Q scores ranged from 50 to 98, and SDs from 13 to 20. The normative total scores for the different BREAST-Q domains are given in Table 1. Women with high BMI values seem to be less satisfied with their breasts, and physical and sexual well-being (Table 2). Women between 40 and 60 years of age seemed more satisfied with their sexual well-being than younger and older women. No other clear differences in scores with age could be seen in breast-related quality of life or donor site satisfaction and well-being (Table 3). The distribution of total scores for different domains is given in Figure 1 for breasts and in Figure 2 for donor sites.
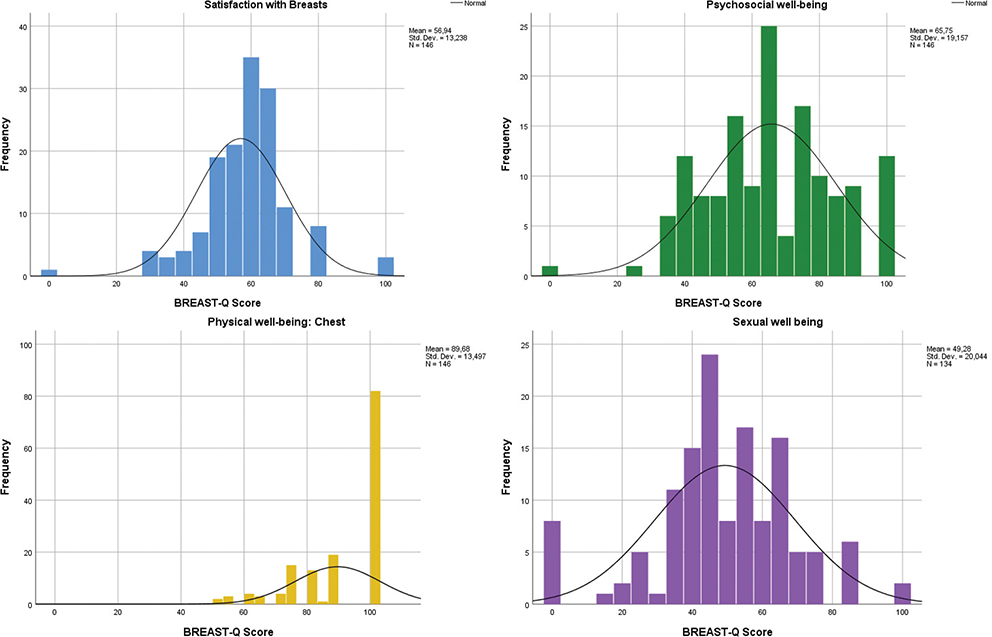
Figure 1. Distribution of BREAST-Q scores for satisfaction with breasts and breast-related quality of life.
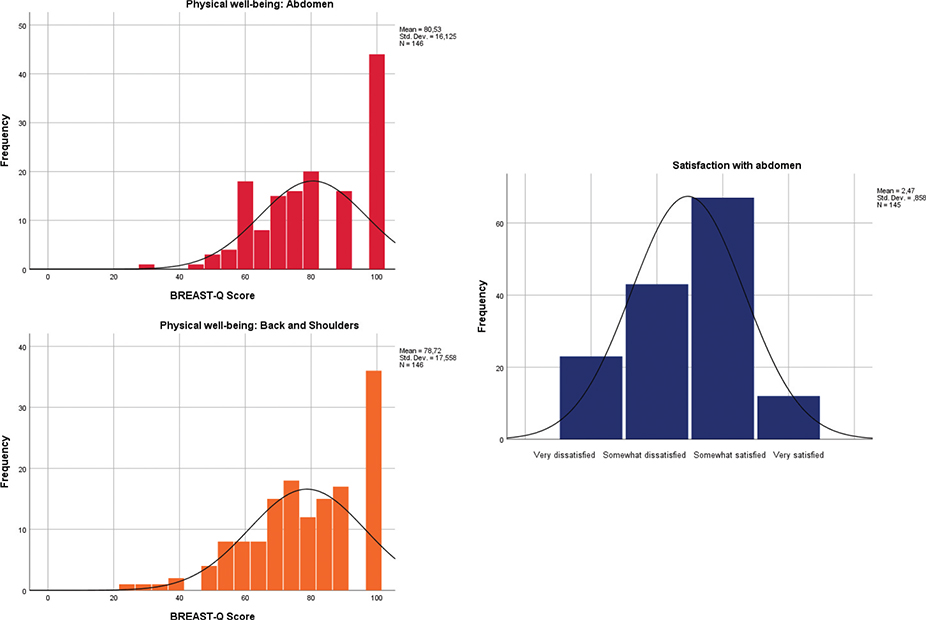
Figure 2. Distribution of BREAST-Q scores for donor sites.
Regarding specific aspects women generally are satisfied or dissatisfied with, the participants were most satisfied with their breasts when clothed, with 91% being somewhat satisfied or very satisfied compared to 60% when unclothed (Figure 3), and more than two-thirds of the women felt normal, self-confident, and emotionally healthy and able to do the things they want. Two-thirds of the women felt feminine in clothes most or all the time, but less than half of the women felt attractive (Figure 4). Only 17% of the participants (Figure 5) felt sexually attractive when clothed some or all of the time. Physical symptoms in the breast area were minimal with more than 90% of the women reporting no symptoms at all, and the most common symptoms being tenderness in breast area (5%) and difficulty lifting or moving the arms (7%) (Figure 6). Regarding donor sites, the most common physical symptom was abdominal bulging and bloating (Figure 7), and the most common back and shoulder symptoms were back and shoulder pain and shoulder stiffness (Figure 8). Overall, the reported physical well-being related to potential donor sites was high with more than two-thirds only reporting symptoms some of the time or none of the time.
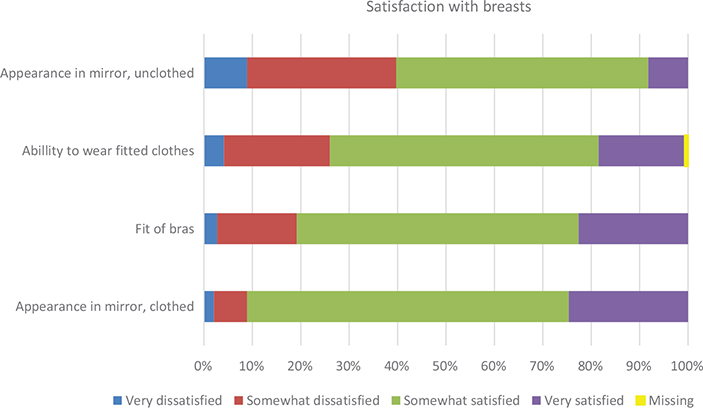
Figure 3. Answers to single items for satisfaction with breasts.
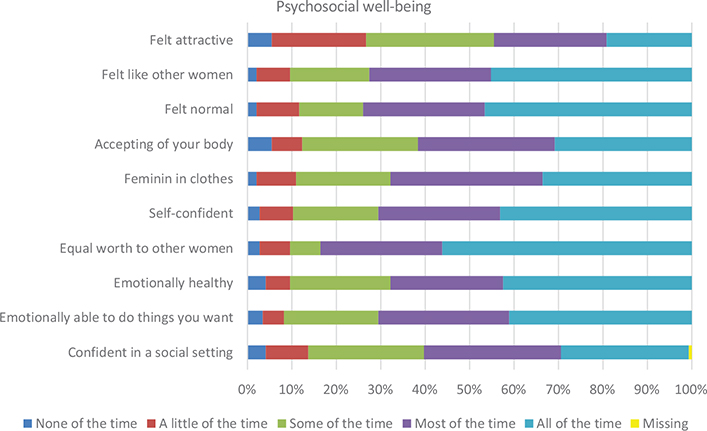
Figure 4. Distribution of BREAST-Q scores for psychosocial well-being.
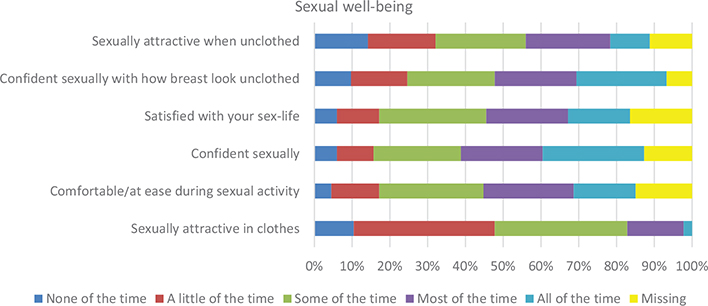
Figure 5. Distribution of BREAST-Q scores for sexual well-being.
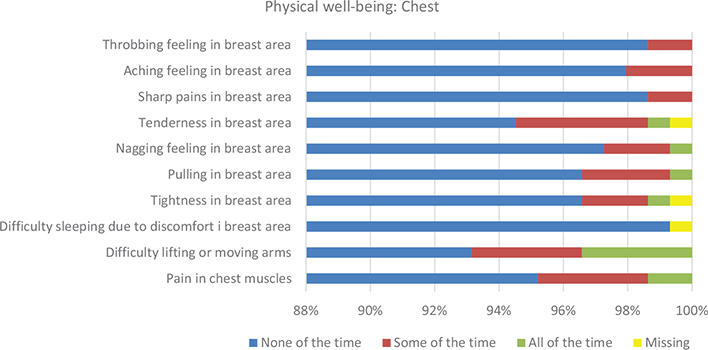
Figure 6. Distribution of BREAST-Q scores for physical well-being chest for Breast-Q version 1.
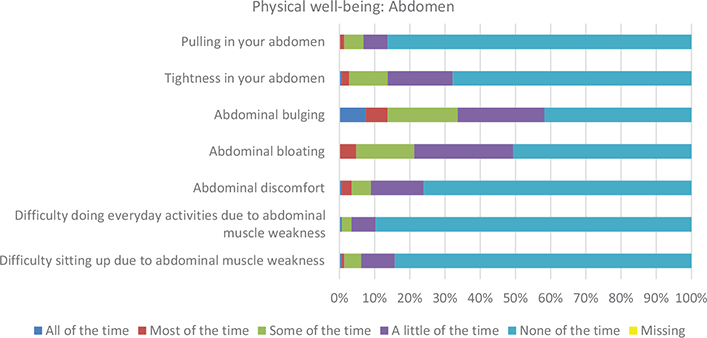
Figure 7. Distribution of BREAST-Q scores for physical well-being (donor site).
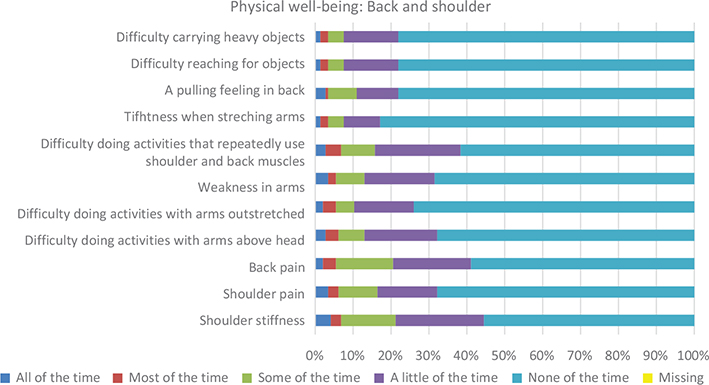
Figure 8. Distribution of BREAST-Q scores for physical well-being back and shoulder (donor site).
Discussion
This is a cross-sectional population study presenting normative data for the BREAST-Q reconstruction module generated in a randomly selected sample of the general population of Region Västra Götaland, Sweden. The population can be used as a control group in future studies on breast reconstruction after breast cancer.
Findings
BREAST-Q scores in this study were similar to both previously reported US norms [5, 6], higher than reported Australian norms [7], and lower than reported Dutch norms [8] for all domains except ‘Physical well-being’ (Table 1). Even though this could be due to sampling variations in the different populations, our findings confirm previous findings and highlight the importance of using population-specific normative data when they are used as comparison in studies. Cultural differences in breast-related quality of life and satisfaction of different donor sites warrant further investigation.
Previous studies have found that BMI affects breast-related satisfaction and quality of life. The results of this study indicate that women with a higher BMI are less satisfied with their breast and have lower sexual and physical well-being scores (Table 2). This is consistent with previous findings [5–8], except for that women with a higher BMI did not have a lower psychosocial well-being in our study. Nonetheless, the findings suggest that the patients’ BMI should be taken into consideration when evaluating the outcomes, as it can be expected that patients with a higher BMI would be less satisfied.
Age also seems to have an impact on breast-related satisfaction and quality of life. Previous studies suggest that women < 40 years of age are less satisfied with their breasts [6] and have a better psychosocial well-being [7], whereas women > 40 appear to have a lower sexual well-being [5,7]. The only association between age and BREAST-Q scores in our study was that women <40 and >60 years of age seem to have a lower sexual well-being. However, our findings are uncertain as there were few women in each group and a higher proportion of participants of older age. Even so, the Australian study [7] and one US study [5] also showed a decreased sexual well-being with increasing age. More studies regarding the effect of age on breast-related quality of life are needed to allow for a fair evaluation of breast reconstruction outcomes.
Regarding satisfaction with breast, our findings suggest that many women in the general population are dissatisfied with their breasts with an average score of only 57 out of a maximum score of 100, and almost half of the women being very or somewhat dissatisfied with their appearance unclothed. This is in accordance with the findings in both US studies [5,6] and the Australian study [7], while the Dutch study had slightly higher scores (mean score 68). These findings are also reflected in the distribution of cosmetic procedures according to the Aesthetic Plastic Surgery National Statistics 2020–2021 [16] with breast-related operations being among the most common procedures performed, that breast dissatisfaction is common. Likewise, abdominoplasty and liposuction are among the most frequently performed esthetic procedures, suggesting a similar level of dissatisfaction with abdomen among women in the general population, which is also reflected in our study with almost half of the participants being very or somewhat dissatisfied with the look of their abdomen. This should be taken into consideration when evaluating the outcome of breast reconstruction and underlines the value of normative data as a reference point. The norm cannot be that all women with reconstructed breasts after breast cancer are very satisfied with their breasts, as this is not the state in a population of women having healthy, natural breasts.
Physical well-being scores for both chest and donor sites were high and similar to the previously published US, Australian, and Dutch norms [5–8]. Physical well-being back and shoulder was not registered in these studies; however, in a previous study validating the Breast-Q latissimus dorsi questionnaire [4], the mean score for back and shoulder function from a population of 157 healthy women was 76 compared to 79 in our study. The score for physical well-being chest of the Breast-Q 2.0 version stands out with a mean score of 98 out of a maximum score of 100 compared to a mean score of 84 for the first version of Breast-Q. As stated earlier, six questions were removed from the physical well-being chest domain in the Breast-Q 2.0 version, including questions about back, shoulder, and neck pain, which, in our study, account for the lower score in version one. Considering that neck and back pain are among the most frequent reasons to visit a general practitioner or physiotherapist in primary care in Europe [17,18], and that the lifetime prevalence of low back pain is reported to be as high as 84% [19], it is reasonable to believe that this is also the case for the previous studies. Consequently, when comparing Breast-Q scores of version 2.0 with historic data from version 1.0, the above should be taken into consideration.
Methodological issues
A challenge when creating normative data is achieving scores from a population that is representative of the general population. In this study, the questionnaire was sent to a random selection of female residents in Region Västra Götaland. Hence, a truly random sample of the general female population should have received the questionnaire in contrast to previous studies. Nonetheless, this does not mean that the women responding are truly representative of the women receiving the questionnaire. As only the Swedish version of the questionnaire was distributed, this automatically excludes women of the non-Swedish speaking part of the population. Even though two reminders were sent, the response rate was only 36.5%. The exact response rate in the previous studies from the US and Australia is unknown due to the method of recruiting [5–7]. The response rate in the Dutch study was 28% [8]. Moreover, the annual survey on public health performed by Statistics Sweden by including 44,800 randomly selected people had a response rate of 37.9% in 2022 [20]. Hence, the response rate corresponds to similar surveys and is at an expected level.
Nonetheless, the low response rate might have affected the representativeness. In this study, we chose to collect data only on age, height, and weight to limit the invasion of privacy of the participants. Moreover, some demographic factors such as ethnic/cultural group cannot generally be registered in Sweden. Indeed, the mean age of the women included in this study is about 10 years above the average in Region Västra Götaland. There could be a bias regarding other sociodemographic factors, such as educational and income levels. A previous study [6] has indicated that an income < 40,000 dollars a year could affect satisfaction with breasts. However, these data did not come from a general population, but from a sample of women who are members of an organization working to strengthen breast cancer research, which could have biased the results. Three previous studies [5–7] have included bra size as a demographic variable and reported lower scores for satisfaction with breasts for women with larger breast cup sizes when compared to women with smaller cup sizes. However, we chose to omit this as bra size is a very crude indicator of breast size [21]. In summary, the scarce demographic data introduces an uncertainty regarding representativeness which makes a cautious interpretation of our results warranted.
Distribution-based minimal important differences (MIDs) were not calculated for our sample as they do not tell us much about clinically relevant differences [4]. A previous study has suggested that a MID score of 4 points on the transformed 0 to 100 scale is clinically useful when assessing a patients outcome using the reconstruction module of BREAST-Q [22]. However, these MIDs are based on statistical distribution and not on what constitutes a relevant change for the patients. Furthermore, there could be significant differences in what constitutes a clinically relevant change of score between patients depending on preoperative impairment; that is, patients who had a mastectomy prior to reconstruction might have more impairment preoperatively than women undergoing mastectomy and immediate reconstruction and therefor be more likely to have a larger difference between pre- and postoperative scores, which should be taken into consideration when establishing clinically relevant MIDs. Studies regarding clinically relevant MIDs for BREAST-Q are warranted.
Conclusions
Normative data for BREAST-Q constitute a reference point, which allows us to put another perspective on changes in scores rather than just comparing scores before and after surgery.
This is the first study of Scandinavian normative values for BREAST-Q reconstruction, and they are somewhat different than scores in previously published normative populations, which further indicates that there might be cultural differences in breast satisfaction.
Data availability
The datasets used and/or analyzed during this study are available from the corresponding author on reasonable request.
Contributions
In accordance with the ‘Vancouver protocol’, all the coauthors have made a substantial contribution to the study, the writing process, and the final manuscript. The manuscript has been seen and approved by all coauthors.
Ethics declarations
This study is one of the studies described in the ‘Reconstruction with back donor site flaps study’ protocol (ClinicalTrials.Gov identifier NCT04526561). This study was reviewed and approved by the Regional Ethical Committee of Gothenburg/Swedish Ethical Review Authority (254-18, 2021-00432, and 2022-06235-02). Procedures were followed in accordance with the Helsinki Declaration and Good Clinical Practice guidelines. Personal data were treated in accordance with the General Data Protection Regulation, and all patients provided written informed consent to participate in this study.
ORCIDs
Christian Jepsen  https://orcid.org/0009-0004-2742-1435
https://orcid.org/0009-0004-2742-1435
Anna Paganini  https://orcid.org/0000-0001-7043-0063
https://orcid.org/0000-0001-7043-0063
Emma Hansson  https://orcid.org/0000-0002-3218-0881
https://orcid.org/0000-0002-3218-0881
References
[1] Potter S, Holcombe C, Ward JA, Blazeby JM, Group BS. Development of a core outcome set for research and audit studies in reconstructive breast surgery. Br J Surg. 2015;102: 1360–1371. https://doi.org/10.1002/bjs.9883
[2] Davies CF, Macefield R, Avery K, Blazeby JM, Potter S. Patient-reported outcome measures for post-mastectomy breast reconstruction: a systematic review of development and measurement properties. Ann Surg Oncol. 2021;28:386–404. https://doi.org/10.1245/s10434-020-08736-8
[3] Cohen WA, Mundy LR, Ballard TN, et al. The BREAST-Q in surgical research: a review of the literature 2009–2015. J Plast Reconstr Aesthet Surg. 2016;69:149–162. https://doi.org/10.1016/j.bjps.2015.11.013
[4] Kamya L, Hansson E, Weick L, Hansson E. Validation and reliability testing of the Breast-Q latissimus dorsi questionnaire: cross-cultural adaptation and psychometric properties in a Swedish population. Health Qual Life Outcomes. 2021;19:174. https://doi.org/10.1186/s12955-021-01812-x
[5] Klifto KM, Aravind P, Major M, et al. Establishing institution-specific normative data for the BREAST-Q reconstruction module: a prospective study. Aesthet Surg J. 2020;40:NP348–NP355. https://doi.org/10.1093/asj/sjz296
[6] Mundy LR, Homa K, Klassen AF, Pusic AL, Kerrigan CL. Breast cancer and reconstruction: normative data for interpreting the BREAST-Q. Plast Reconstr Surg. 2017;139:1046e–1055e. https://doi.org/10.1097/PRS.0000000000003241
[7] Crittenden TA, Smallman A, Dean NR. Normative data for the BREAST-Q Reconstruction module in an Australian population and comparison with US norms and breast reconstruction patient outcomes. J Plast Reconstr Aesthet Surg. 2022;75: 2219–2228. https://doi.org/10.1016/j.bjps.2022.01.033
[8] Sadok N, Jansen L, De Zoete MD, Van der Lei B, Werker PMN, De Bock GH. A Dutch cross-sectional population survey to explore satisfaction of women with their breasts. Plast Reconstr Surg Glob Open. 2021;9:e4002. https://doi.org/10.1097/GOX.00000e00000004002
[9] Aesthetic plastic surgery national databank statistics 2020. Aesthet Surg J. 2021;41:1–16. https://doi.org/10.1093/asj/sjab178
[10] Tuna Butt S, Widmark-Jensen E, Meyer S, Hansson E. Swedish normative scores for the BREAST-Q reduction/mastopexy module. Aesthetic Plast Surg. 2023;47:73–80. https://doi.org/10.1007/s00266-022-03025-z
[11] Klassen AF, Pusic AL, Scott A, Klok J, Cano SJ. Satisfaction and quality of life in women who undergo breast surgery: a qualitative study. BMC Womens Health. 2009;9:11. https://doi.org/10.1186/1472-6874-9-11
[12] Cano SJ, Klassen AF, Scott AM, Cordeiro PG, Pusic AL. The BREAST-Q: further validation in independent clinical samples. Plast Reconstr Surg. 2012;129:293–302. https://doi.org/10.1097/PRS.0b013e31823aec6b
[13] Pusic AL, Klassen AF, Scott AM, Klok JA, Cordeiro PG, Cano SJ. Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q. Plast Reconstr Surg. 2009;124: 345–353. https://doi.org/10.1097/PRS.0b013e3181aee807
[14] BREAST-Q users’ manual. Memorial Sloan Kettering Cancer Center. Memorial Sloan Cancer Center. New York. 2015.
[15] BREAST-Q Version 2.0 users’ manual. Memorial Sloan Kettering Cancer Center. Memorial Sloan Cancer Center. New York. 2017.
[16] Aesthetic plastic surgery national databank statistics 2020–2021. Aesthet Surg J. 2022;42:1–18. https://doi.org/10.1093/asj/sjac116
[17] Bot SD, van der Waal JM, Terwee CB, et al. Incidence and prevalence of complaints of the neck and upper extremity in general practice. Ann Rheum Dis. 2005;64:118–123.
[18] Corp N, Mansell G, Stynes S, et al. Evidence-based treatment recommendations for neck and low back pain across Europe: a systematic review of guidelines. Eur J Pain. 2021;25:275–295. https://doi.org/10.1002/ejp.1679
[19] Balague F, Mannion AF, Pellise F, Cedraschi C. Non-specific low back pain. Lancet. 2012;379:482–491. https://doi.org/10.1016/S0140-6736(11)60610-7
[20] Officiel statistik [Internet]. Available from: https://www.folkhalsomyndigheten.se/folkhalsorapportering-statistik/officiell-statistik/ [2023 August 19]
[21] Ringberg A, Bageman E, Rose C, Ingvar C, Jernstrom H. Of cup and bra size: reply to a prospective study of breast size and premenopausal breast cancer incidence. Int J Cancer. 2006; 119:2242–2243; author reply 2244. https://doi.org/10.1002/ijc.22104
[22] Voineskos SH, Klassen AF, Cano SJ, Pusic AL, Gibbons CJ. Giving meaning to differences in BREAST-Q scores: minimal important difference for breast reconstruction patients. Plast Reconstr Surg. 2020;145:11e–20e. https://doi.org/10.1097/PRS.0000000000006317