ORIGINAL RESEARCH ARTICLE
Speech in 7- and 10-year-olds born with a unilateral cleft lip and palate: a continued prospective Swedish intercentre study
Christina Havstama,b, Karin Brunnegårdc, Emilie Hagbergd,e, Cecilia Nellif, Åsa Okhiriag and Kristina Klintöh,i
aDepartment of Otorhinolaryngology, Speech and Language Pathology, Sahlgrenska University Hospital, Gothenburg, Sweden; bInstitute of Neuroscience and Physiology, Department of Health and Rehabilitation, Speech and Language Pathology Unit, Sahlgrenska Academy, University of Gothenburg, Sweden; cDepartment of Clinical Sciences, Speech and Language Pathology, Umeå University, Sweden; dMedical Unit Speech and Language Pathology and Stockholm Craniofacial Team, Karolinska University Hospital, Stockholm, Sweden; eDivision of Speech and Language Pathology, Department of Clinical Science, Intervention and Technology, Karolinska Institutet, Stockholm, Sweden; fSpeech and Language Pathology Unit, Otorhinolaryngology Clinic, University Hospital Linköping, Sweden; gDepartment of Surgical Sciences, Plastic Surgery, Uppsala University, Uppsala, Sweden; hDivision of Speech Language Pathology, Department of Otorhinolaryngology, Skåne University Hospital, Malmö, Sweden; iDivision of Speech Language Pathology, Phoniatrics and Audiology, Department of Clinical Sciences in Lund, Lund University, Sweden
ABSTRACT
The aim of this study was to report longitudinal speech results in consecutively selected children from each of the six cleft centres in Sweden and to compare the results between centres. The children were born with a non-syndromic unilateral cleft lip and palate, and results from the same cohort at 5 years of age have previously been reported. Background data on medical care in terms of surgery, speech therapy, and hearing between 5 and 10 years of age were collected. Speech recordings of 56 children at 7 years and 54 at 10 years of age were blindly and independently assessed by four speech-language pathologists experienced in cleft palate speech. This resulted in measures of percent consonant correct (PCC) and perceived velopharyngeal competence rated on a three-tier scale. No statistically significant differences were found between centres. PCC scores at 7 years of age ranged from 44 to 100% (median 97.5) and at 10 years of age from 86 to 100% (median 100). Competent or marginally incompetent velopharyngeal function was found in 95% of the 7-year-olds and 98% of the 10-year-olds. Speech results were slightly better than previous reports of speech in children born with a unilateral cleft lip and palate.
KEYWORDS: Speech; unilateral cleft lip and palate; intercentre study
Citation: Journal of Plastic Surgery and Hand Surgery 2023; 58: 149–154. DOI: https://doi.org/10.2340/jphs.v58.15766.
Copyright: © 2023 The Author(s). Published by MJS Publishing on behalf of Acta Chirurgica Scandinavica. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material, with the condition of proper attribution to the original work.
Received: 30 June 2023; Accepted: 10 October 2023; Published: 18 December 2023.
CONTACT: Christina Havstam christina.havstam@vgregion.se Department of Otorhinolaryngology, Speech and Language Pathology, Sahlgrenska University Hospital, SE-413 45, Gothenburg, Sweden
Competing interests and funding: The authors report no conflicts of interest and are fully and solely responsible for the content of this article.
The study was performed as an evaluation of results within the clinical context without any external funding.
Introduction
Speech results constitute one of the most important outcome measures of surgical success in children born with a cleft involving the palate. Previously, speech results in 57 consecutively selected 5-year-olds treated at the six cleft centres in Sweden were reported, and no statistically significant differences in speech were found between centres [1]. The present study is a continued follow-up of the same cohort at ages 7 and 10 years.
Percent consonants correct (PCC) is a common outcome measure to describe a child’s speech production, which was first introduced by Shriberg and Kwiatkowski in 1982 [2]. It has subsequently been adapted to evaluate articulation proficiency in individuals born with a cleft palate [3, 4]. PCC has been recommended by the International Consortium of Health Outcome Measures (ICHOM) as one of two important outcomes in perceptual cleft palate speech evaluation [5]. The second recommended outcome measure is rating of velopharyngeal competence (VPC), using the scale VPC-R which has been validated [6]. In the previous article on speech at age 5 years in the same cohort as in this study, the term perceived VPC was used for the same variable [1]. VPC is an overall estimate of velopharyngeal function based on speech symptoms such as hypernasality, nasal air leakage and reduced pressure in consonants requiring high intra-oral pressure. Hypernasality is sometimes analysed separately but often with low reliability in the assessments [7], whereas assessments of VPC have achieved better reliability [8].
Several studies of cleft palate speech have focused on the timing of hard palate closure, however few studies have assessed speech after 5 years of age. The Scandcleft trials recruited 448 patients born with a unilateral cleft lip and palate, who were randomised into two different surgical protocols at each centre, where one of the alternatives was a method common for all participating centres [9]. In children treated with two-stage closure of the palate, with soft palate closure at 3 to 4 months, articulation proficiency at 5 years of age was significantly better after hard palate closure at 12 months of age than after hard palate closure at 36 months of age [9]. No significant differences in velopharyngeal competency (evaluated with the composite variable VPC-sum) and hypernasality were found [10]. At 10 years of age, the results indicated that children treated with two-stage closure with hard palate closure at 36 months had lower PCC than children treated with simultaneous hard and soft palate closure at 12 months of age, whereas the proportion of children with primary VPC (without secondary surgery to improve function) was higher in the group with delayed hard palate closure [11]. A national survey from New Zealand included 56 children with cleft lip and palate at 10 years of age and found adequate velopharyngeal function in 66% and a need for further investigation or therapy in 25% [12].
In Sweden, about 175 children are diagnosed with a cleft palate and/or cleft lip every year [13]. They are treated at one of the six regional multidisciplinary cleft centres, where the surgical procedures differ in technique, staging, and timing.
The aim of this study was to report speech results in terms of PCC and VPC at 7 and 10 years of age, in a consecutive series of children born with unilateral cleft lip and palate in Sweden, and to compare these between the six cleft centres.
Materials and methods
Ethical considerations
The study was approved by the Regional Ethical Review Board in Stockholm, Sweden (Dnr: 2012/1991-31/3 and 2015/250-32). Caregivers of all participants gave their written informed consent for participation.
Participants
The original aim was to include 10 consecutive patients born from 2008 to 2010 from each of the six Swedish cleft centres. In total, 58 children were recruited, but one recording from Linköping failed at the age of 5 years. This resulted in recordings of 57 children, and speech results at 5 years of age have been previously reported [1]. Recruited children who attended their routine follow-up visits at the cleft centres at 7 years ± 4 months and 10 years ± 1 year were included in the continued study. This resulted in 56, 7-year-olds (mean age 6.94 years; range 6.67–7.17) and 54, 10-year-olds (mean age 10.06 years; range 9.83–10.58). See Table 1 for details on numbers and sex distribution at the six centres.
Hearing
Data on hearing were routinely collected at 7 and 10 years of age in connection with the speech assessment, but data were missing for four children at the age of 7 years and for five children at age 10 years. See Table 2 for results of audiometry where the threshold level for normal hearing was set to ≤ 20 dB. Sixty-seven percent of the children with available hearing data were found to have normal hearing at the age of 7 years and 74% at the age of 10 years.
Primary palatal surgery
In Gothenburg, primary soft palate surgery was performed at mean age 7.2 months (range 5–12), and hard palate surgery in nine children at 24 months (range 20–27). One child with a wide palatal cleft had hard palate surgery in two stages at 24 and 36 months of age. In all, four surgeons performed the primary palatal surgery. In Linköping, soft and hard palate surgery was performed in one stage at mean age 19.5 months (range 16–30) by one surgeon, in Malmö at mean age 11.3 months (range 10–12) by one surgeon, and in Stockholm at mean age 12.5 months (range 12–13) by three different surgeons. In Umeå, soft palate surgery was performed at mean age 5.6 months (range 5–10) and hard palate surgery at mean age 25.8 (range 24–31) by one surgeon. In Uppsala, soft palate surgery was performed at mean age 7.1 months (range 6–8) and hard palate surgery at mean age 26.2 months (range 24–39) by three different surgeons. For further details on primary palatal surgery and lip-nose surgery, see the previously reported results at the age of 5 years [1].
Alveolar bonegrafting
All children from Linköping and Umeå had undergone their alveolar bonegrafting before 10 years of age. One child at each of the centres in Gothenburg, Malmö, and Uppsala, and four children from Stockholm, had unoperated alveolar clefts at the speech assessment at 10 years of age. One child from Gothenburg and one from Malmö had received a reoperation of the alveolar cleft.
Secondary surgery
Number and type of surgical interventions to improve velopharyngeal function, and palatal fistula closure are presented in Table 3, with the previously reported surgical procedures [1] included. One child treated in Malmö had a large residual cleft in the alveolar process that was extended into the hard palate, which was closed with secondary surgery. This procedure was included in the palate re-repair category (Table 3). A total of 14 children (24%) had received some type of secondary surgery of the palate by the age of 10 years. The median number of secondary surgeries at the different centres was three (range 0–8).
Speech reviews and treatment
Number of speech-language pathologist (SLP) visits was collected via the SLPs at the cleft centres and at the local hospitals. This includes all direct contact between child and SLP, both assessments and therapy. Contact with SLPs in a school setting was not included as speech therapy is mainly administered via hospitals in Sweden (Table 4).
Documentation
The children were audio recorded in a quiet room at one of the cleft centres, using audio recorders of high quality (Zoom H4n, Hauppauge, NY, or TASCAM HD-P2, Montebello, California), and a condenser microphone (Røde NT4, Sydney, Australia, or Sony ECM-MS957, Tokyo, Japan). The Swedish test for articulation and nasality, SVANTE, [14] was used. It contains single words and sentences sensitive for cleft speech characteristics, such as high-pressure consonants, nasals, and combinations of nasals and high-pressure consonants [14]. In addition, the children produced connected speech by re-telling the Bus-story [15, 16], describing pictures, or participating in conversation.
Editing
All recordings were saved in .wav-format and edited in Audacity (Free Software). Information that could lead to identification of the patient was removed. Each speech sample was arranged in the same sequence, first the isolated words, then the sentences and lastly the connected speech sample. Three speech samples from each centre and age, a total of 36 samples (33%), were duplicated to enable calculation of intra-judge agreement. The speech samples were compiled in random order.
Perceptual assessment and analysis
Four SLPs, from four different cleft centres, performed independent blinded assessments of all speech samples, using headphones of good quality (AKG K271, Vienna, Austria; Bang & Olufsen Beoplay HX, Struer, Denmark; Sennheiser HD 280 Pro, Wedemark, Germany; Sony MDR-V700, Tokyo, Japan). The SLPs had 6–23 years of experience with cleft palate speech. Firstly, they assessed the speech of the 7-year-olds, and then of the 10-year-olds. Target consonants in the single words were phonetically transcribed with ‘semi-narrow’ transcription according to the International Phonetic Alphabet [17]. VPC was assessed on a three-tier rating scale (0 = competent, 1 = marginally incompetent, 2 = incompetent) [14]. PCC was calculated by dividing the number of target consonants produced with correct manner and place of articulation with the total number of elicited consonants for each child [14].
Reliability
Intra-judge agreement was calculated on the 36 randomly chosen speech samples, and inter-judge agreement on the assessments of all speech samples. The results on reliability were interpreted according to Cicchetti [18]. Absolute agreement for PCC was calculated with the Intraclass Correlation Coefficient (ICC), using a two-way mixed effect model. Intra-judge reliability calculated with average measures ICC ranged from 0.919 to 0.987 (confidence interval [CI] 0.841 – 0.993), indicating excellent agreement. Inter-judge agreement was also excellent (ICC 0.955; CI 0.934–0.969). The median PCC values of the four judges for each child were reported as results of PCC. Intra- and inter-judge agreement of VPC was calculated with percentage exact agreement and linear weighted Kappa. Percentage exact intra-judge agreement ranged from 78 to 94%, and with exclusion of the judge with lowest intra-judge agreement, it was 92–94%. Kappa values for intra-judge agreement ranged from 0.464–0.888 (CI 0.166–1) with all judges included, and with exclusion of the judge with the lowest intra-judge agreement it was 0.779–0.888 (CI 0.595–1), which qualifies as excellent. Inter-rater reliability for the three judges with the highest intra-judge agreement was calculated pairwise with linear weighted Kappa and ranged from 0.439 to 0.705 (CI 0.295–0.834), indicating fair to good agreement. The results presented on VPC were based on the median of the three judges with the highest intra-judge agreement.
Statistical analysis
SPSS (the IBM Statistical Package for the Social Sciences, version 28) was used for statistical analysis. Non-parametric statistics were used due to small samples and skewed data. Comparisons between centres were performed with the Kruskal-Wallis test for independent samples. The level of statistical significance was set to p < 0.05 (two-tailed).
Results
Percent consonants correct
Results on PCC at 7 and 10 years of age are presented in Table 5. No statistically significant differences in PCC between centres were found at any age.
Velopharyngeal competence
VPC was rated as competent or marginally incompetent in 95% of the 7-year-olds and 98% of the 10-year-olds (Figure 1). There were no statistically significant differences in VPC between centres at any age.
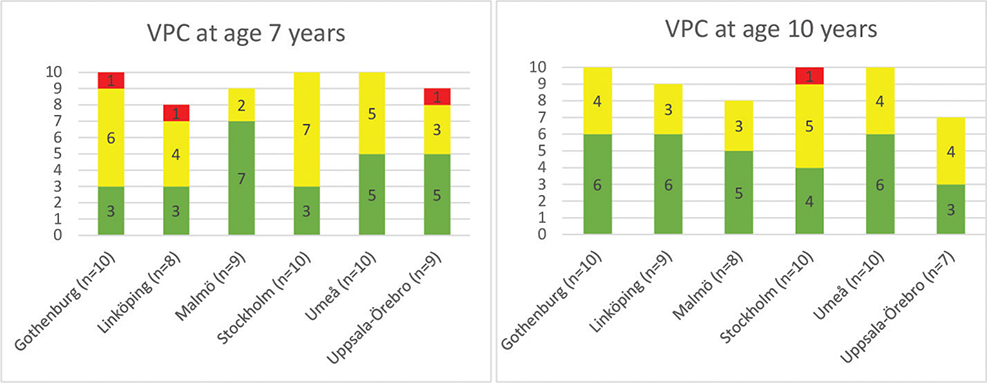
Figure 1. Velopharyngeal competence (VPC) at 7 and 10 years of age. The bars represent number of children with competent (green), marginally incompetent (yellow) and incompetent (red) function at each centre.
Discussion
The aim of this study was to report and compare speech results in consecutively selected children born with a unilateral cleft lip and palate, treated at the six cleft centres in Sweden. In the previous study of the same cohort at 5 years of age, PCC-A (percent consonant correct adjusted for age) was used to investigate whether the children with cleft achieved the norms of children without a cleft [1]. Age-appropriate consonant processes at 5 years of age, that is, simplification of /s/, were scored as correct. The median PCC-A score at 5 years of age was 93.9% [1]. The corresponding median PCC scores at 7 and 10 years of age in the present study were 97.5 and 100, respectively. It is well-known that children born with a cleft palate often are delayed in their speech development and that they more often have phonological disorders than peers without a cleft at age 5 years [19]. Furthermore, 82.5 % of the children were perceived to have competent or marginally incompetent velopharyngeal function at 5 years of age [1], compared with 95% at 7 years and 98% at 10 years of age. Most children with cleft palate with speech disorders in their earlier years improve their speech with increasing age [20] and this was confirmed in this study.
There were no statistically significant differences between centres in the present study, however the groups were small. Individual variation was evident. The child with the lowest PCC scores (44% at 7, and 86% at 10 years of age) had a language disorder that influenced the results. The mean PCC score of the total group at 10 years of age (98.4) was higher than the mean PCC score of 10-year-olds with unilateral cleft lip and palate in the Scandcleft trials, where the mean scores varied between 86 and 92% in the different trial arms [11]. In the Scandcleft trials, 50–73% of children in the different trial arms achieved age-appropriate norms of children without a cleft (a PCC score > 91%) [9], compared with 92.6% (50 out of 54) of the 10-year-olds in this study. Thus, the 10-year-olds in this study had better consonant proficiency than the 10-year-olds in the Scandcleft described as overall PCC [11].
About 80% of the 10-year-olds in the Scandcleft trials had a competent or a marginally incompetent velopharyngeal function according to the composite score VPC-sum, which is a lower proportion than in this study (98%), although the outcomes are not fully comparable since velopharyngeal function in this study was estimated using the measure VPC-R. Another complicating factor is the differences in size as the Scandcleft study included 448 10-year-olds and our study only 54. In a previous Swedish study of 69 children born with unilateral cleft lip and palate, 93% had competent velopharyngeal function at 10 years of age [21], which is a somewhat lower proportion than in this study (98%). In the nation-wide study of 56 10-year-olds born with complete cleft lip and palate treated in New Zealand, 66% had adequate velopharyngeal function and 25% were in need for further investigation or therapy [12]. In their study, bilateral and unilateral complete clefts were not separated, which complicates the comparison with our data. However, compared with studies with equivalent variables for speech evaluation, the speech results at the age of 10 years in this study were relatively good.
The overall burden of care for children born with a unilateral cleft lip and palate is an important aspect to address. However, incomplete and inconsistent data collection about speech therapy often make comparisons between centres difficult [20]. The amount of SLP visits is sometimes seen as an indication of a child’s speech problem but is probably more related to availability of services and different criteria used for therapy inclusion.
Based on studies of peers’ perceptions of cleft palate speech [22, 23], we concluded that a marginally incompetent velopharyngeal function, which is noticed by SLPs experienced in assessing cleft palate speech, often goes unnoticed by other children. Incompetent velopharyngeal function and articulation disorders are more important to identify and treat, as this may be commented on in rather negative terms by 7- and 10-year-olds without a cleft palate [22, 23]. We therefore considered both competent and marginally incompetent velopharyngeal function a satisfactory speech result. All but one child in our study achieved a competent or marginally incompetent velopharyngeal function at 10 years of age. That child was judged to have a marginally incompetent function at 7 years of age. It is well known that velopharyngeal function may change as a child grows, and this finding highlights the need for repeated speech assessments during childhood and adolescence.
There are challenges in conducting a prospective longitudinal multicentre study, without any external funding. Several factors, such as children moving from their original regions, financial restrictions in healthcare, staff shortage, and staff replacement where relevant information is not passed on to new staff, jeopardise adequate data collection and the possibility to participate in time-consuming speech assessments. Even though SLPs experienced in cleft palate speech assessed the speech samples, with the same assessment methods and scales that they regularly use in their clinical work, reliability of VPC was lower than expected. This was solved by using the median score of the three SLPs with the highest intra-judge reliability.
Based on the experiences of this study, we have created guidelines for future clinical national studies on cleft palate speech, with a recommendation to appoint an SLP in charge for regularly checking that relevant information is passed on to the other SLPs about the agreed protocol, to make sure it is followed continuously. Furthermore, structured listener calibration is recommended before the perceptual assessment starts, to optimise listener agreement.
In this study, small numbers of participants and missing data made it difficult to identify any systematic differences between the six cleft centres. However, a majority of the participating children did follow through from 5 to 10 years of age and had data on all agreed variables, presenting valid speech data from a consecutive series of children born with a unilateral cleft lip and palate in Sweden.
Acknowledgements
The authors wish to thank Professor Anette Lohmander who initiated this study and applied for ethical approval, and Jan-Olof Malmborn who performed speech analyses.
ORCID
Christina Havstam  https://orcid.org/0000-0003-0015-9364
https://orcid.org/0000-0003-0015-9364
References
[1] Klintö K, Brunnegård K, Havstam C, et al. Speech in 5-year-olds born with unilateral cleft lip and palate: a prospective Swedish intercenter study. J Plast Surg Hand Surg. 2019; 53: 309–315. https://doi.org/10.1080/2000656X.2019.1615929
[2] Shriberg LD, Kwiatkowski J. Phonological disorders III: a procedure for assessing severity of involvement. J Speech Hear Disord. 1982; 47: 256–270. https://doi.org/10.1044/jshd.4703.256
[3] Lohmander A, Persson C. A longitudinal study of speech production in Swedish children with unilateral cleft lip and palate and two-stage palatal repair. Cleft Palate Craniofac J. 2008; 45: 32–41. https://doi.org/10.1597/06-123.1
[4] Sell D, Sweeney T. Percent consonant correct as an outcome measure for cleft speech in an intervention study. Folia Phoniatr Logop. 2020; 72: 143–151. https://doi.org/10.1159/000501095
[5] Allori AC, Kelley T, Meara JG, et al. A standard set of outcome measures for the comprehensive appraisal of cleft care. Cleft Palate Craniofac J. 2017; 54: 540–554. https://doi.org/10.1597/15-292
[6] Lohmander A, Hagberg E, Persson C, et al. Validity of auditory perceptual assessment of velopharyngeal function and dysfunction – the VPC-Sum and the VPC-Rate. Clin Linguist Phon. 2017; 31: 589–597. https://doi.org/10.1080/02699206.2017.1302510
[7] Brunnegård K, Lohmander A. A cross-sectional study of speech in 10-year-old children with cleft palate: results and issues of rater reliability. Cleft Palate Craniofac J. 2007; 44: 33–44. https://doi.org/10.1597/05-164
[8] Brunnegård K, Hagberg E, Havstam C, et al. Reliability of speech variables and speech related quality indicators in the Swedish cleft lip and palate registry. Cleft Palate Craniofac J. 2020; 57: 715–722. https://doi.org/10.1177/1055665619894497
[9] Willadsen E, Lohmander A, Persson C, et al. Scandcleft randomised trials of primary surgery for unilateral cleft lip and palate: 5. Speech outcomes in 5-year-olds – consonant proficiency and errors. J Plast Surg Hand Surg. 2017; 51: 38–51. https://doi.org/10.1080/2000656X.2016.1254647
[10] Lohmander A, Persson C, Willadsen E, et al. Scandcleft randomised trials of primary surgery for unilateral cleft lip and palate: 4. Speech outcomes in 5-year-olds – velopharyngeal competency and hypernasality. J Plast Surg Hand Surg. 2017; 51: 27–37. https://doi.org/10.1080/2000656X.2016.1254645
[11] Willadsen E, Jørgensen LD, Alaluusua S, et al. Scandcleft randomised trials of primary surgery for unilateral cleft lip and palate: speech proficiency at 10 years of age. Int J Lang Com Disord. 2023; 58: 892–909. https://doi.org/10.1111/1460-6984.12830
[12] Morrison MM, Mason NT, Forde BL, et al. Speech outcomes of a national cohort of children with orofacial cleft at 5 and 10 years of age. Cleft Palate Craniofac J. 2022; 59: 1400–1412. https://doi.org/10.1177/10556656211044939
[13] Klintö K, Eriksson M, Abdiu A, et al. Inter-centre comparison of data on surgery and speech outcomes at 5 years of age based on the Swedish quality registry for patients born with cleft palate with or without cleft lip. BMC Pediatr. 2022; 22: 303. https://doi.org/10.1186/s12887-022-03367-2
[14] Lohmander A, Lundeborg I, Persson, C. SVANTE – The Swedish Articulation and Nasality Test – normative data and a minimum standard set for cross-linguistic comparison. Clin Linguist Phon. 2017; 31: 137–154. https://doi.org/10.1080/02699206.2016.1205666
[15] Renfrew, CE. Bus story test: a test of narrative speech. Bicester, Oxon: Winslow Press, 1997.
[16] Svensson Y, Tuominen-Eriksson AM. Bussagan [The Bus Story]. Gothenburg, Sweden: Specialpedagogiska institutet Läromedel; 2002. [Swedish].
[17] The International Phonetic Alphabet (Revised to 2015). extIPA Symbols for Disordered Speech (Revised to 2008). International Phonetic Association. [cited 2023 May 10]. Available from: https://www.internationalphoneticassociation.org/content/ipa-chart
[18] Cicchetti DV. The precision of reliability and validity estimates re-visited: distinguishing between clinical and statistical significance of sample size requirements. J Clin Exp Neuropsychol. 2001; 23: 695–700. https://doi.org/10.1076/jcen.23.5.695.1249
[19] Klintö K, Salameh E K, Lohmander A. Phonology in Swedish-speaking 5-year-olds born with unilateral cleft lip and palate and the relationship with consonant production at 3 years of age. Int J Speech Lang Pathol. 2016; 18: 147–156. https://doi.org/10.3109/17549507.2015.1081287
[20] Lohmander A. Surgical intervention and speech outcomes in cleft lip and palate. In: Howard S, Lohmander A, editors. Cleft palate speech: assessment and intervention. Hoboken, NJ: Wiley-Blackwell; 2011. p. 55–85.
[21] Nyberg J, Peterson P, Lohmander A. Speech outcomes at age 5 and 10 years in unilateral cleft lip and palate after one-stage palatal repair with minimal incision technique – a longitudinal perspective. Int J Pediatr Otorhinolaryngol. 2014; 78: 1662–1670. https://doi.org/10.1016/j.ijporl.2014.07.016
[22] Nyberg J, Havstam C. Speech in 10-year-olds born with cleft lip and palate: what do peers say? Cleft Palate Craniofac J. 2016; 5: 516–526. https://doi.org/10.1597/15-140
[23] Nyberg J, Hagberg E, Havstam C. ‘She sounds like a small child or perhaps she has problems’-peers’ descriptions of speech in 7-year-olds born with cleft palate. Cleft Palate Craniofac J. 2020; 57: 707–714. https://doi.org/10.1177/1055665619890785