ORIGINAL RESEARCH ARTICLE
Direct fixation of fracture fragment with modified double Kirschner wires for the treatment of old bony mallet finger
Yong Zhanga*, Yingluo Gua*, Jupu Zhoua, Jiaju Zhaoa and Bo Jianga,b
aDepartment of Hand and Foot Surgery, The Second Affiliated Hospital of Soochow University, Suzhou, Jiangsu, China; bState Key Laboratory of Radiation Medicine and Protection, Soochow University, Suzhou, Jiangsu, China
ABSTRACT
Background: The management of old bony mallet fingers is complicated. The purpose of this study was to describe direct fixation of fracture fragment with modified double Kirschner wires (K-wires) for treatment of old bony mallet finger, and to evaluate the functional outcomes during long-term follow-up.
Methods: Forty-nine patients with old bony mallet finger were enrolled and underwent surgical treatment from August 2014 to January 2021 in our hospital. Patients were divided into two groups according to whether they had undergone triple K-wires fixation or modified double K-wires with a dorsal brace fixation. The operation time, mean number of intraoperative fluoroscopy, bone union time, functional recovery and incidence of complications were monitored.
Results: Neither QuickDASH nor visual analogue scale measurement found statistically significant difference between the two groups (P > 0.05). However, the patients that underwent fixation with double K-wires and a dorsal brace required a shorter operation time and fewer intraoperative fluoroscopy, and exhibited a significantly greater mean final active range of the distal interphalangeal joint flexion, compared to those treated with triple K-wires (P < 0.01).
Conclusion: Direct fixation of fracture fragment with modified double K-wires was an easy and feasible procedure which could achieve anatomical reduction and stable fixation of the dorsal fracture block of old bony mallet finger with relatively few complications.
KEYWORDS: Bony mallet finger; fracture fixation; Kirschner wires; dorsal brace.
Citation: Journal of Plastic Surgery and Hand Surgery 2023; 58: 119–123. DOI: https://doi.org/10.2340/jphs.v58.18306.
Copyright: © 2023 The Author(s). Published by MJS Publishing on behalf of Acta Chirurgica Scandinavica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Received: 26 July 2023; Accepted: 4 September 2023; Published: 29 September 2023.
CONTACT Bo Jiang jiangbo082611@163.com Department of Hand and Foot Surgery, The Second Affiliated Hospital of Soochow University, Suzhou, 215004, Jiangsu, China. State Key Laboratory of Radiation Medicine and Protection, Soochow University, Suzhou, 215123, Jiangsu China.
*These authors contributed equally to this work as co-first author.
Competing interests and funding: No potential conflict of interest was reported by the authors.
This work was supported by the Science and Technology and Planning Program of Suzhou City (No. SYS2020127, No. SKY2022143), the Lifting Project of Discipline Construction of the Second Affiliated Hospital of Soochow University (No. XKTJ-HRC2021008).
Introduction
Bony mallet finger is a common type of finger deformity that results from a rupture of the extensor tendon or a bony avulsion injury at the base of the distal phalanx. This, as a consequence, leads to loss of the extensor mechanism of the distal interphalangeal (DIP) joint, which produce a fracture of the extensor tendon from the base of the distal phalanx with a bony fragment [1–4]. Most patients receive timely and effective diagnosis and treatment, the recovery is generally good. Some patients evolve into old fractures due to insufficient attention or missed diagnosis in the early stage, which not only increases the difficulty of treatment but also tends to a poor efficacy [5].
The majority of acute bony mallet finger injuries can be treated conservatively with an extension splint or brace for 6–8 weeks, but surgical treatment is required for old bony mallet fingers caused by improper treatment or treatment failure in the acute phase, if the flexion deformity is >40° or the dorsiflexion function is limited [6, 7]. Common surgical strategies include tension band wiring [8], Kirschner wire (K-wire) fixation [4–9], microscrew fixation [10], pullout wire fixation [11], extension block fixation [4, 12, 13] and hook plate [7]. However, these procedures are generally complex and often result in complications.
We have developed a triple K-wires fixation technique that internally fixates the dorsal fracture block with two vertically inserted K-wires and the DIP joint with a third, slightly larger K-wire. This surgical method has been demonstrated in numerous clinical practices to be able to promote stable fixation and accurate reduction of fracture block [14]. Nevertheless, it is still not without complications such as joint degeneration or weakened flexion. Recently, we modified the triple K-wires fixation technique by substituting a dorsal brace for the third K-wire, which showed better efficacy based on preliminary clinical evidence. Therefore, the purpose of this study was to describe direct fixation of fracture fragment with modified double K-wires for treatment of old bony mallet finger, and to report on long-term follow-up results.
Materials and methods
Patients
The study cohort consisted of 49 patients diagnosed with an old bony mallet finger who underwent surgical treatment between August 2014 and January 2021 in our hospital. All patients gave written informed consent. The study was approved by the ethical review committee of the Second Affiliated Hospital of Soochow University. The study adhered to declaration of Helsinki guidelines.
The inclusion criteria wwere (1) the injury time exceeded 4 weeks, (2) the lateral film of the finger showed exceeded one-third of the distal phalanx joint surface, and (3) the affected finger could be passively extended. The exclusion criteria were (1) the avulsion fracture block was comminuted, (2) the width of the fracture block was less than 2 mm, (3) the DIP joint was stiff, and (4) the patient had other serious disease.
Patients were allocated into two groups based on the surgical procedures. Specifically, Group I was composed of 34 patients who were treated by triple K-wires fixation, whereas Group II contained 15 subjects that each received double K-wires with a dorsal brace. All patients were surgically treated between 5 weeks and 13 months after injury. General demographic and clinical information of all patients are summarized in Table 1. The follow-up time of the patients ranged from 11 to 26 months, with a mean value of 16 months.
The duration of the surgery and the number of intraoperative fluoroscopy that each patient received were accurately recorded. Post-surgical recovery was evaluated by measuring the functional range of motion of the DIP joint and monitoring the occurrence of possible complications, such as nail deformity, elongation of the fracture segment, narrowed joint space, or any other degenerative changes. Interphalangeal joint goniometer was used to measure range of motion of the DIP joint of each surgically treated finger. The functional recovery and pain scores were evaluated by the QuickDASH and the visual analogue scale methods.
Surgical procedures
In group I, anesthesia was first induced by digital nerve block, followed by a small curved transverse incision in the dorsal aspect of the DIP joint, raised a flap to the distal end over the dorsal aspect of DIP joint and exposed the fracture site and terminal extensor mechanism. The fractured block was separated, and the extensor tendon was released. After removing the scar tissue and refresh the fracture surface between the dorsal fracture block and distal phalanx, reduction of the bone block was performed under direct vision and maintained with the use of a small periosteal dissector. Next, the fracture was internally fixated by vertically drilling a 0.6 mm or 0.8 mm K-wire into a dorsal-palmar direction across the fracture line. Once anatomic reduction of both the fracture block and the distal phalanx was radiographically confirmed, a second K-wire of the same size was inserted 2–3 mm away from and parallel to the first. The two K-wires were subsequently pulled with an electric drill from the finger pulp, with their dorsal ends positioned 1–2 mm external to the dorsal cortex and their volar ends bent. Finally, a 1.0 mm K-wire was inserted from the fingertip and palmarly across the DIP joint to hold it in slight hyperextension under fluoroscopic guidance. This procedure ensured that the K-wire did not traverse the fracture line, and that the dorsal fracture block was not damaged. The dorsal incision of the DIP joint was closed with 5-0 Prolene sutures (Figure 1a–d). Noteworthy, the obsolete cases needed to remove the scar tissue completely. Six weeks after the surgery, the three K-wires were removed from all patients, who were then instructed to immediately initiate active and passive exercises of their recovering DIP joints.
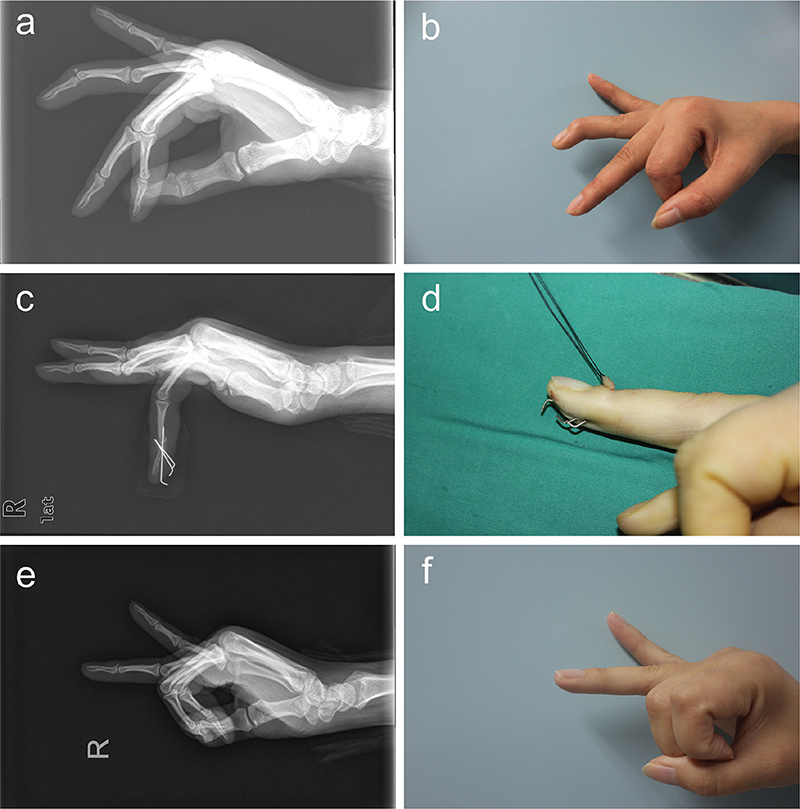
Figure 1. A patient received the triple K-wires fixation treatment for old bony mallet finger with the ring finger of the right hand. (a) Preoperative fluoroscopy. (b) Preoperative appearance. (c) Intraoperative fluoroscopy. (d) Intraoperative appearance. (e) Fluoroscopy 6 months postoperatively. (f) Appearance 6 months postoperatively.
In group II, the procedures for anesthesia, incision and vertical insertion of the first two K-wires were similar to those in triple K-wire fixation elucidated above. However, instead of inserting a third K-wire, a dorsal brace was used to hold the DIP joint in slight hyperextension (Figure 2a–g). Six weeks after the surgery, the two K-wires and the dorsal brace were removed from all patients, who were then instructed to immediately initiate active and passive exercises of their recovering DIP.
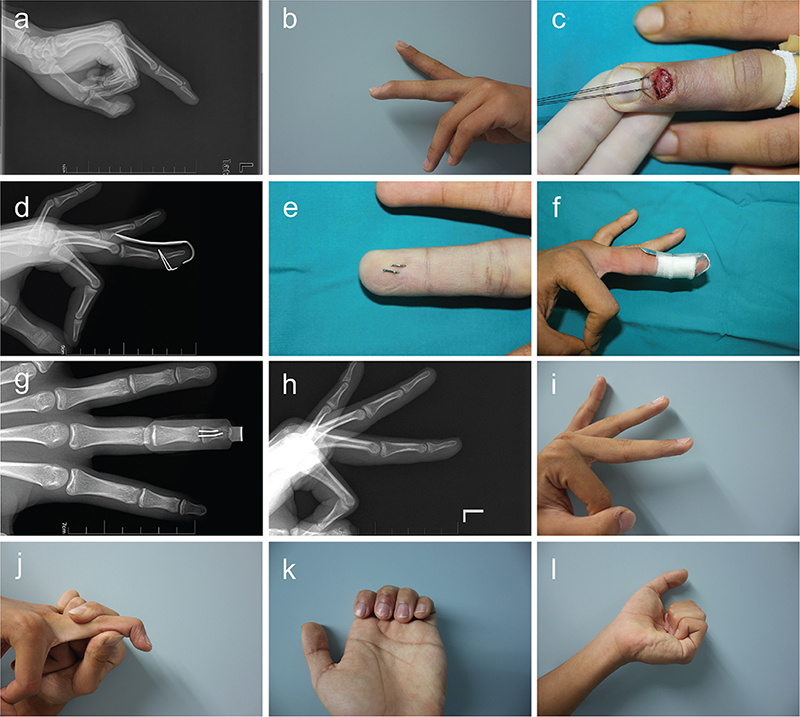
Figure 2. A patient received double K-wires with a dorsal brace treatment for old bony mallet finger with the middle finger of the left hand. (a) Preoperative fluoroscopy. (b) Preoperative appearance. (c, e, f) Intraoperative appearance. (d, g) Intraoperative fluoroscopy. (h) Fluoroscopy 6 months postoperatively. (i–l) Appearance 6 months postoperatively.
Statistical analysis
Statistical analyses were performed using SPSS 21.0 (SPSS, Inc., Chicago, IL, USA). Continuous variables were expressed as the means ± standard deviations, and categorical variables were expressed as numbers. The independent-samples t-test was employed to compare differences between the two groups. Differences within the same group were compared by paired Student’s t-test, and categorical variables were compared using the chi-square test. P < 0.05 was considered statistically significant.
Results
There was no statistically significant difference in age, gender, mechanism of injury, mean time to surgery, size of fracture block involved articular surface between the two groups (P > 0.05). Meanwhile, surgical treatment performed on the patients in Group I lasted an average of 53.68 ± 1.60 min, whereas the mean operation time for Group II was significantly shorter at 36 ± 1.48 min (P < 0.01). The patients in Group I also, on average, received a greater number of intraoperative fluoroscopy (P < 0.01) (Table 1). In all patients, the surgical incisions achieved healing by first intention and conclusive radiographic evidence of bone union was obtained.
Subsequent follow-up found 15 cases of nail deformity, 10 in Group I and five in Group II, which disappeared after a mean period of 8 months (between 6 and 10 months). Furthermore, radiological examinations revealed that 18 patients, including 14 in Group I and 4 in Group II, showed signs of joint degeneration or joint space narrowing. Among them, eight from Group I and four from Group II were considered to have developed mild joint degeneration, whereas another 11 from Group I exhibited several degenerative changes with mild joint pain (Table 2). However, none of the patients had to limit their daily activities or seek additional surgical intervention because of the complications. No severe complications or surgical incidents, such as infection, skin necrosis, K-wire breakage, avascular necrosis of the fracture block, cold intolerance or prominent dorsal bump were observed.
| Complications | Group I | Group II | P |
| Nail deformity | 10 | 5 | 0.784 |
| Severe joint degeneration | 11 | 0 | 0.012 |
| Mild joint degeneration | 8 | 4 | 0.814 |
The mean final extensor lag was 7° for Group I and 10° for Group II, with no statistically significant difference in between. However, the DIP joint flexion of patients in Group I showed a significantly narrower mean final active range of 66° (in the range of 55° – 90°) compared to that of Group II (mean of 75.4° and range of 67° – 90°). QuickDASH outcome measurement produced an average score of 11.74 for Group I and 11.8 for Group II, whereas the mean visual analogue scale scores of Groups I and II were 0.21 and 0.27, respectively (Table 1), both showing no statistically significant inter-group difference. Figures 1 and 2 present typical cases.
Discussion
Common surgical methods for treating bony mallet fingers can be divided into two categories, including closed reduction-internal fixation (CRIF) and open reduction-internal fixation (ORIF) [15]. For the old bony mallet finger, especially when the fracture block is significantly displaced, it is often accompanied by the turnover of the fracture block, extensor tendon retraction and adhesion, and the callus and fibrous tissue between the fracture ends, which will hinder the reduction and affect fracture healing. It is often difficult to maintain anatomical reduction the fracture block with CRIF. In these cases, an ORIF procedure is generally employed [16–18]. Therefore, we believe that the old bony mallet finger usually needs to be accurately reduced by open reduction, and removed callus and fibrous tissue of the fracture end and restored fresh bone interface so as to facilitate the fracture healing. Despite the availability of a wide selection of ORIF methods, they often produce inconsistent results in different patients and sometimes even lead to severe complications or aggravation of symptoms [19, 20].
The size of the fracture block at the base of the distal phalanx of the patients included in this study was more than one third of the joint surface of the distal phalanx. Therefore, the use of 0.6 mm or 0.8 mm K-wire to directly fix the fracture block in this study has clear operability and safety. In clinical practice, we found that when only one K-wire was inserted into the avulsion fracture block for fixation, the fracture block might rotate and the fixation was usually unstable. Therefore, in this study, two 0.6 mm or 0.8 mm K-wires were used to fix the fracture block. No avulsion fracture block split occurred during the intraoperative fixation process, and even one to two times of intraoperative adjustment could be made without causing fracture block.
In this study, all participating patients achieved anatomical reduction of the dorsal fracture blocks and radiographic bone union within 8 weeks, with a mean value of 6.5 weeks. There was no significant difference between the two groups in the incidence of transient nail ridging. However, patients that underwent fixation with double K-wires and a dorsal brace showed significantly fewer incidences of joint degeneration or joint space narrowing than those who received triple K-wires. In addition, treatment with double K-wires and a dorsal brace significantly decreased the time of surgery and number of intraoperative fluoroscopy, and the flexion function was basically the same as before injury. Based on these findings, we tentatively concluded that holding the DIP joint with a dorsal brace instead of a K-wire could not only achieve anatomical reduction and stable fixation but also reducing certain postoperative complications such as joint degeneration.
The fixation of the DIP joint with a K-wire, as practiced in the triple K-wires method, was a rather complicated procedure compared to that with a dorsal brace. When the avulsed bone block was large, it was difficult to prevent the K-wire from inserting into the fracture end when inserting from the distal end to the proximal end, which would affect the anatomical reduction of the fracture block. Moreover, the risk of destroying the avulsed bone block was often higher when drilling a K-wire for fixation of the DIP joint. For a good position of the K-wire, it always required multiple drills and fluoroscopy, which not only increased operation time and radiation exposure but also damaged the cartilage surface of the DIP joint. Moreover, the risk of traumatic arthritis would be increased in the later stage [5].
Furthermore, our clinical studies found that within 6 weeks after the surgery, substantially more patients undergoing triple K-wires fixation developed joint degeneration or joint space narrowing than those that were subjected to fixation with double K-wires and a dorsal brace. In particular, six of these patients with triple K-wires fixation suffered mild joint pain and eight showed varying degrees of joint stiffness with limited and/or weakened flexion functions. We speculated that the poorer patient outcome of the triple K-wires fixation technique could be attributed to joint degeneration and severe fibrous hyperplasia induced by the rigid internal fixation and lack of micromovement of the DIP joint.
Interestingly, the hook of the dorsal brace could pull the abdominal skin of the finger to make the DIP joint extension or mild hyperextension, which should be based on the softness of the affected fingers and do not force a certain extension of the bit to avoid pressure sores.
Long time fixation would inevitably lead to the decline of the dorsal extensor strength of the distal finger, which was not enough to resist the refractory flexion trend of the finger, so that the finger flexed gradually after removing the fixation. Meanwhile, the formation of tendon adhesion made the extensor tendon unable to effectively slide 5 mm to the proximal side under the condition of decreased muscle strength, resulting in difficulty in dorsiflexion of the distal finger. Therefore, we believed that the refractory flexion tendency of fingers, weak dorsalis and tendon adhesion were the main causes of active extensor lag.
The main limitation of this study was the lack of a comparison of the extension lag of the patients. In addition, the number of sample cases included in this study was insufficient as only 49 cases were analyzed. The follow-up research on the above limitations makes the focus of our further study.
Conclusion
Compared to the use of triple K-wires, fixation with double K-wires and a dorsal brace provides significant benefits in operation time, radiation exposure, post-surgical complications and functional recovery of the injured finger flexion. Direct fixation of fracture fragment with modified double K-wires was an easy and feasible procedure which could achieve anatomical reduction and stable fixation of the dorsal fracture block of old bony mallet finger with relatively few complications.
Ethical approval
The study was approved by the ethical review committee of the Second Affiliated Hospital of Soochow University with an approve No. EC2014087.
ORCID
Yong Zhang  https://orcid.org/0000-0002-2783-9768
https://orcid.org/0000-0002-2783-9768
Yingluo Gu:  https://orcid.org/0009-0007-5777-5121
https://orcid.org/0009-0007-5777-5121
Jupu Zhou:  https://orcid.org/0000-0001-6830-8931
https://orcid.org/0000-0001-6830-8931
Jiaju Zhao:  https://orcid.org/0000-0002-8810-3121
https://orcid.org/0000-0002-8810-3121
Bo Jiang:  https://orcid.org/0000-0001-5702-0473
https://orcid.org/0000-0001-5702-0473
References
[1] Gumussuyu G, Asoglu MM, Unal M, et al. Reliability of subluxation and articular involvement measurements during the assessment of bony mallet finger. Hand Surg Rehabil. 2021;40(1):87–92. https://doi.org/10.1016/j.hansur.2020.08.008
[2] Wang L, Zhang X, Liu Z, et al. Tendon-bone graft for tendinous mallet fingers following failed splinting. J Hand Surg Am. 2013; 38(12):2353–2359. https://doi.org/10.1016/j.jhsa.2013.09.008
[3] Degreef I, De Smet L. Multiple simultaneous mallet fingers in goalkeeper. Hand Surg. 2009;14(2–3):143–144. https://doi.org/10.1142/S0218810409004396
[4] Lee YH, Kim JY, Chung MS, et al. Two extension block Kirschner wire technique for mallet finger fractures. J Bone Joint Surg Br. 2009;91(11):1478–1481. https://doi.org/10.1302/0301-620X.91B11.22478
[5] Tang J, Wu K, Wang J, et al. Open reduction and compression with double Kirschner wires for the treatment of old bony mallet finger. J Orthop Surg Res. 2019;14(1):459. https://doi.org/10.1186/s13018-019-1513-2
[6] Alla SR, Deal ND, Dempsey IJ. Current concepts: mallet finger. Hand (N Y). 2014;9(2):138–144. https://doi.org/10.1007/s11552-014-9609-y
[7] Wang WC, Hsu CE, Yeh CW, et al. Functional outcomes and complications of hook plate for bony mallet finger: a retrospective case series study. BMC Musculoskelet Disord. 2021;22(1):281. https://doi.org/10.1186/s12891-021-04163-2
[8] Damron TA, Engber WD. Surgical treatment of mallet finger fractures by tension band technique. Clin Orthop Relat Res. 1994;300:133–140. https://doi.org/10.1097/00003086-199403000-00017
[9] Lubahn JD. Mallet finger fractures: a comparison of open and closed technique. J Hand Surg Am. 1989;14(2 Pt 2):394–396. https://doi.org/10.1016/0363-5023(89)90121-4
[10] Kronlage SC, Faust D. Open reduction and screw fixation of mallet fractures. J Hand Surg Br. 2004;29(2):135–138. https://doi.org/10.1016/j.jhsb.2003.10.012
[11] Zhang X, Meng H, Shao X, et al. Pull-out wire fixation for acute mallet finger fractures with k-wire stabilization of the distal interphalangeal joint. J Hand Surg Am. 2010;35(11):1864–1869. https://doi.org/10.1016/j.jhsa.2010.07.021
[12] Ishiguro T, Itoh Y, Yabe Y, et al. Extension block with Kirschner wire for fracture dislocation of the distal interphalangeal joint. Tech Hand Up Extrem Surg. 1997;1(2):95–102. https://doi.org/10.1097/00130911-199706000-00005
[13] Gumussuyu G, Asoglu MM, Guler O, et al. Extension pin block technique versus extension orthosis for acute bony mallet finger; a retrospective comparison. Orthop Traumatol Surg Res. 2021;107(5):102764. https://doi.org/10.1016/j.otsr.2020.102764
[14] Jiang B, Wang PJ, Zhao JJ. The treatment of bony mallet fingers using a triple K-wire fixation technique. J Hand Surg Eur Vol. 2015;40(8):864–866. https://doi.org/10.1177/1753193414553139
[15] Giddins GE. Bony mallet finger injuries: assessment of stability with extension stress testing. J Hand Surg Eur Vol. 2016;41(7):696–700. https://doi.org/10.1177/1753193416647307
[16] Ulusoy MG, Karalezli N, Koçer U, et al. Pull-in suture technique for the treatment of mallet finger. Plast Reconstr Surg. 2006; 118(3):696–702. https://doi.org/10.1097/01.prs.0000232983.23840.f2
[17] Lee SK, Kim HJ, Lee KW, et al. Modified pull-out wire suture technique for the treatment of chronic bony mallet finger. Ann Plast Surg. 2010;65(5):466–470. https://doi.org/10.1097/SAP.0b013e3181d377c2
[18] Reddy M, Ho CA. Comparison of percutaneous reduction and pin fixation in acute and chronic pediatric mallet fractures. J Pediatr Orthop. 2019;39(3):146–152. https://doi.org/10.1097/BPO.0000000000000896
[19] Miura T. Extension block pinning using a small external fixator for mallet finger fractures. J Hand Surg Am. 2013;38(12):2348–2352. https://doi.org/10.1016/j.jhsa.2013.09.009
[20] Kim JY, Lee SH. Factors related to distal interphalangeal joint extension loss after extension block pinning of mallet finger fractures. J Hand Surg Am. 2016;41(3):414–419. https://doi.org/10.1016/j.jhsa.2015.11.026