ORIGINAL RESEARCH ARTICLE
Proximal row carpectomy versus four-corner arthrodesis: a retrospective comparative study
Richard Chan, MDa,d, Justine Goursat, MDa, Mathilde Payen, MDb, Matthieu Lalevèe, MDa,e and Kamel Guelmi, MDc
aChirurgie Orthopédique Adulte, CHU Charles Nicolle, Rouen, France; bChirurgie Orthopédique Pédiatrique, CHU Charles Nicolle, Rouen, France; cChirurgie Orthopédique Adulte, GHH Monod, Montivilliers, France; dChirurgie de la main et plastique adulte, CHU Charles Nicolle, Rouen, France; eCETAPS UR3832, Research Center for Sports and Athletic Activities Transformations, Université de Rouen, Mont-Saint-Aignan, France
ABSTRACT
Background: Four-corner arthrodesis with scaphoid excision (FCA) and proximal row carpal resection (PRC) are frequently performed in wrists with post-traumatic Scaphoid Non-Union Advanced Collapse (SNAC)/Scapho-Lunate Advanced Collapse (SLAC) osteoarthritis. The aim of this study was to compare the clinical outcomes of these two procedures.
Methods: This single-center, retrospective cohort study included all patients who had PRC or FCA between January 1st, 2009 and January 1st, 2019 and who were followed up. Follow-up included: mobility (radial deviation, ulnar deviation, flexion, extension), strength (grip test, pinch test), function (QuickDash, patient-rated wrist evaluation [PRWE]), subjective mobility, and global satisfaction scores.
Results: Among 25 patients included, 11 had PRC and 14 had FCA with a mean follow-up of 69.5 months [12–132]. Radial deviation was 18° versus 14° (p = 0.7), ulnar deviation was 21° versus 22° (p = 0.15), flexion was 39° versus 30° (p = 0.32), extension was 32.5° versus 29.5° (p = 0.09), grip test compared to the controlateral side was 72% versus 62% (p = 0.53), Quick Dash score was 12.5 versus 17.6 (p = 0.84), PRWE was 18.7 versus 17.6 (p = 0.38), subjective mobility was 7.8 versus 7.5 (p = 0.23), and satisfaction score was 8.7 versus 9 (p = 0.76), respectively, in the FCA group and the PRC group. Re-operation rates were 14% patients in the FCA group and 0% in the PRC group.
Conclusion: This study found no significant difference between FCA and PRC on strength, mobility, and function in patients with post-traumatic SLAC or SNAC stage II wrist arthritis. Both FCA and PRC seem to be reliable surgical techniques with good outcomes with more revision in the FCA group.
KEYWORDS: Hand surgery; wrist; four bones arthrodesis; proximal row carpectomy; Scaphoid Non Union Advanced Collapse; Scapho-Lunate Advanced Collapse
Citation: Journal of Plastic Surgery and Hand Surgery 2024; 59: 77–82. DOI: https://doi.org/10.2340/jphs.v59.18338.
Copyright: © 2024 The Author(s). Published by MJS Publishing on behalf of Acta Chirurgica Scandinavica. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material, with the condition of proper attribution to the original work.
Received: 31 July 2023; Accepted: 6 May 2024; Published: 20 May 2024
CONTACT: Mathilde Payen mathilde-payen@hotmail.fr Chirurgie orthopédique pédiatrique. CHU Charles Nicolle, 37 Boulevard Gambetta, FR-76000 Rouen, France.
Competing interests and funding: The authors report there are no competing interests to declare.
This study was conducted without financial support.
Introduction
Four-corner arthrodesis with scaphoid excision (FCA) and proximal-row carpal resection (PRC) are common operations for wrists with post-traumatic Scaphoid Non Union Advanced Collapse (SNAC) or Scapho-Lunate Advanced Collapse (SLAC) stage II [1,2]. The clinical results of both procedures are satisfactory, giving good recovery of strength, mobility and function, each with its advantages and limits [1,2]. Although controversial, some studies consider that FCA maintains strength and PRC provides better mobility [3,4]. Over the last 30 years, the material used for FCA has developed considerably. Initially made with Kirschner wires in the 1990s, today osteosynthesis material is used that allows better stability (plates with locked screws, agraphs, etc.). The literature shows that PRC, compared to FCA, is 70–425% less expensive [5], has a shorter surgical time of 57 min versus 121 min [5], is technically less difficult and has a shorter duration of immobilization ranging from 0 to 3.5 weeks [6–8] versus 2–8 weeks [6,9].
Aim of the study
Currently, there are no comparative studies showing the superiority of one of these two techniques. The main hypothesis of this study was the superiority of FCA procedure compared to PRC procedure for strength, mobility, and function. The purpose of this study was to compare the clinical and radiographic results of these two procedures in SNAC/SLAC stage II wrists [1,2].
Material and methods
This single-center retrospective comparative study included patients operated by PRC or FCA between January 1st, 2009 and January 1st, 2019, who had follow-up. All patients were operated by the same surgeon. Data collection was performed by an independent observer.
General data
The following patient data were collected: age, sex, surgical history, dominant hand, occupation, etiology, operated side and type of operation: PRC or FCA all in SNAC/SLAC II, overall patient satisfaction (scale of 1–10) and subjective wrist mobility (scale of 1–10), and duration of time off work. Postoperative complications and repeat surgeries were reported.
Specific data
All mobility measurements were performed bilaterally using a goniometer: radial and ulnar deviation angles, flexion and extension of the wrist. Strength measurements were performed by Grip test, using a Jamar® hydraulic hand dynamometer, and by Pinch test, using a Jamar® hydrolic pinch gauge. Function measurements were performed using two validated questionnaires: Quick Dash (Quick disability of the arm, shoulder and hand) and the patient-rated wrist evaluation [10, 11] (PRWE).
Surgical technique
The patient was positioned supine on an arm table with a pneumatic tourniquet. The approach for FCA and PRC was similar. The incision on the dorsal aspect of the wrist was longitudinal and centered on the 4th extensor compartment. The extensor retinaculum was totally opened. The 4th compartment was reclined ulnarly, the 3rd radially.
The neurectomy of the posterior interosseous nerve was performed 1 cm below the 4th compartment as described by van Hernen et al. [12]. The capsulotomy was longitudinal. For the four bone arthrodesis and scaphoidectomy, the scaphoid was removed in one piece. The cartilage between the capitate, hamate, lunate, and triquetrum was trimmed with a gouge. The scaphoid was cut to prepare the bone graft between the four bones. The Dorsal intercalated segment instability (DISI) was reduced with a transradial Kirshner wire. The LEIBINGER® plate (Stryker US) was placed with four screws of 2.3 cortical diameter, one screw in each bone with the graft (Figure 1). During the resection of the first carpal row, once the capsulotomy was performed, the three bones, scaphoid, lunate and triquetrum were removed one by one.
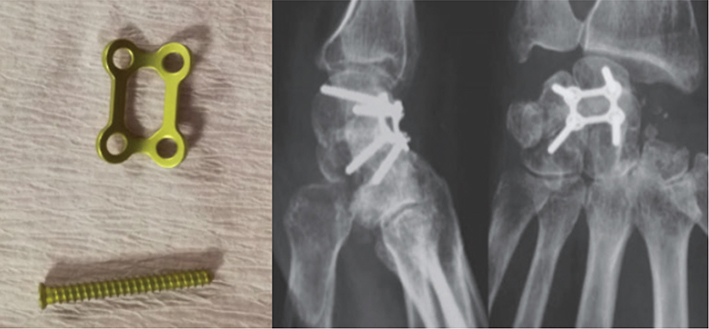
Figure 1. LIEBINGER plate with its 4 screws of diameter 2.3 cortical, a screw in each bone was necessary and radiographic result plate and screws placed.
Patients with FCA and PRC surgery had an antebrachial splint for 6 weeks and with immediate active physical therapy, for metacarpalphalangeal, proximal, distal interphalangeal joint. And immediate passive wrist joint then active mobisation of the wirst at 6 weeks postoperatively.
Statistical analysis
A nonparametric Wilcoxon–Mann–Whitney test was used for patient characteristics and a parametric Student’s t-test for mobility, strength, and function measures following the normal distribution. The comparability of the initial characteristics of the two groups was demonstrated by the Fisher exact test with Yates correction on R software. The statistical significance chosen was p < 0.05.
Ethics
This study followed the Declaration of Helsinki. Before each consultation, the design of the research was presented. Anonymity and medical confidentiality were respected by the investigator. Informed consent was obtained voluntarily from each patient included in the study.
Results
Baseline characteristics of the patients
Table 2 summarizes the etiology, the results of mobility, strength, wrist function, and patient satisfaction in both groups (Table 1). The mean total follow-up of patients was 69.5 months [12–132 months]. There was no difference in length of follow-up between the two groups (p = 0.84).
| Data | FCA | PRC | Total | P |
| N | 14 | 11 | 25 | |
| Mean age (years) | 59 | 66 | / | p = 0.01* |
| Men | 13 | 8 | 21 | p = 0.28** |
| Women | 1 | 3 | 4 | |
| Dominant wrist | 6 | 4 | 10 | p = 1** |
| Non-dominant wrist | 8 | 7 | 15 | |
| SLAC | 9 | 10 | 19 | p = 0.18** |
| SNAC | 5 | 1 | 6 | |
| Mean follow-up (month) | 65.8 | 74 | / | p = 0.84* |
| Time off work (month) | 3 | 2.6 | / | p = 0.84* |
| There was no statistically significant difference between the two groups (p > 0.05). FCA: Four-corner arthrodesis and scaphoid excision; PRC: First-row carpal resection; SNAC: Scaphoid Non Union Advanced Collapse; SLAC: Scapho-Lunate Advanced Collapse. *Student’s t-test, value p = 0.05. **Fischer exact test, value p = 0.05. | ||||
| Assessment criteria | FCA Mean[min-max] | PRC Mean[min-max] | P | |
| Mobility | Mean active radial deviation (degrees) | 18° [5–30°] | 14° [10–20°] | p = 0.70* |
| Mean active ulnar deviation (degrees) | 21° [10–30°] | 22° [10–30°] | p = 0.15* | |
| Mean active flexion (degrees) | 39° [20–50°] | 30° [20–40°] | p = 0.32* | |
| Mean active extension (degrees) | 32.5° [5–45°] | 29.5° [10–45°] | p = 0.09* | |
| Strength | Mean Grip Test (K-force) | 30.8 kg [8–40kg] | 20.3 kg [2–26kg] | p = 0.53* |
| Mean Pinch test (K-force) | 8.2 kg [4.5–10.5 kg] | 6.1 kg [4–7.5 kg] | p = 0.68* | |
| Function | Mean Quick Dash | 12.5 [0–31.82] | 17.6 [4.55–50] | p = 0.84* |
| Mean PRWE | 18.7 [4–37] | 17.6 [5–51] | p = 0.38* | |
| Satisfaction and mobility | Mean global satisfaction | 8.7 [7–10] | 9 [8–10] | p = 0.76* |
| Mean subjective mobility | 7.8 [5–10] | 7.5 [5–10] | p = 0.23* | |
| FCA: Four-corner arthrodesis and scaphoid excision; PRC: First-row carpal excision; PRWE: patient-rated wrist evaluation. *Student Test, value p = 0.05. | ||||
Among 30 patients who had surgery during the inclusion period, 25 were followed up, 3 died and 2 were lost to follow-up. A total of 25 patients were included in the analysis. The age of patients operated on by a PRC was higher than that of the FCA (p = 0.01).
Thirteen patients (52%) were in employment, including seven manual workers (5 in the FCA group, 2 in the PRC group), one of the patients had to change his job following the surgery. There was no difference in the length of time off work after surgery between the two groups (p = 0.84).
Mobility, strengh, function and satisfaction
The results of mobilily, strengh, function and satisfaction are summarized in Table 2.
Complications and surgical revision
Complications
Among the 14 patients in the FCA group, two of them had pseudarthrosis. Both were at the triquetro-lunate level and without functional consequences. One of them was 48 years old, had surgery 3 years ago, a Quick Dash score of 2.27/100, and a PRWE score of 2.5. The other patient was 68 years old, had surgery 4 years previously, a Quick Dash score of 4.55/100, and a PRWE score of 12. None of the 11 patients who had PRC had any complications, including radiocapital arthrosis.
Revision surgery
Among the 14 patients in the FCA group, two (14%) had a second operation. Both at 1 year after the first surgery for removal of hardware on a wrist extension defect. None of the 11 patients who had PRC had revision surgery.
Discussion
This study showed no difference between FCA and plate osteosynthesis versus PRC on strength, mobility, and function with a mean follow-up of 69.5 months in patients with SLAC or SNAC post-traumatic wrist arthritis. Thus, our original hypothesis was not confirmed.
Methods
The parameters chosen in this study were to evaluate strength, function, mobility, and pain in daily life. These parameters were used to analyze the overall success of these interventions and to compare them.
The Quick Dash score is an international score used in postoperative assessment of FCA or for PRC [1–3,7–9,13–16]. This score focuses on function. A total of 8 out of 11 items are based on daily tasks and only three on pain. It looks at hand, wrist, elbow and shoulder. The score may be biased when the patient has an upper limb pathology other than the wrist. This was not the case among the 25 patients reviewed in this series.
The PRWE score is also an international score that can be used in the postoperative evaluation of both procedures [17]. It allows a better study of pain with half of its items dedicated to its scoring. The association of the two scores allowed to be precise and limited the biases.
All mobility measurements were made by a single independent observer, limiting measurement bias. Force was studied in relation to the contralateral side. The equipment used for the grip test and pinch test was the same for all patients, limiting measurement bias.
All patients were seen and operated on by the same surgeon with the same technique for both operations, using the same material, the LEIBINGER® plate for the FCA. The objective measures were complemented by overall satisfaction and subjective mobility reported to the patients.
Analysis
Population
The rate of lost to follow-up was low with only five in a series of 30 patients. The average age of our series was 59.5 years, with only 52% active workers. Functional demand was lower for 48% of retirees, which may therefore bias our overall satisfaction score.
The mean age was higher in the PRC group (p = 0.01). The selection bias was due to the initial indication. In the case of a young and active patient, the operator chose FCA in view of the resumption of work and the need to maintain strength.
Mobility, strength and function
There was no difference between the two groups on mobility, functional scores and strength. Although not significant, the average grip test strength was greater in the FCA group: 30.8 kg compared to the PRC group: 20.3 kg. In our series, there is 72% in the FCA group versus 62% of the PRC group in the grip test. It is reasonable to assume that FCA gives better results in terms of grip test strength. There is a 10% loss of mobility in the FCA group (66%) compared to the PRC group (76%), on the ulnar deviation Berkhout et al. [6].
Global satisfaction and subjective mobility
No difference was found between the two groups regarding these two scores. For daily life, 5° to 40° of flexion, 30° to 40° of extension, 10°–20° of radial deviation and 15°–20° of ulnar deviation are required [18,19]. Mobility scores in this series were within the norms for daily living, yet subjective mobility scores were lower than overall satisfaction scores. Subjective mobility was rated at 7.8/10 for the FCA group versus 7.5/10 in the PRC group while subjective satisfaction was 8.7/10 versus 9/10.
Subjective mobility was not the predominant factor in patient satisfaction. There was an excellent overall satisfaction rating for both groups. All the patients reported that their satisfaction was linked to the explanations given by the surgeon. The patients were all warned of the loss of strength, mobility and the threshold given to them was 50% loss of strength, mobility and function before the operation. The worst score was seven corresponding to the patient who had to change his job following an FCA.
Complications and surgical revisions
The rate of post-PRC revision surgery is 0% compared to 14% for FCA, but it is not applicable in the long term. The revision surgeries in the FCA group were for plaque removal. No patient was reoperated for total wrist arthrodesis (TWA).
The rate of radiocapital osteoarthritis in PRC, for all diseases combined, varies from 0 to 18% at 10 years [20–25], with a survival rate of 65% at 20 years [14]. However, it is precisely in the context of radiocapital osteoarthritis that TWA is performed [26,27].
The result of this series is, however, in agreement with the series of Williams et al. [26] showing that with a follow-up of 8.2 years, there was no difference between the two groups in the rate of conversion to TWA. However, secondary surgery was higher in the FCA group (34.4%) versus PRC (16.1%).
Comparaison with other studies
Berkhout et al. [6] did not find any significant difference in strength, function and mobility except for ulnar deviation, which was greater with PRC (Table 3). They presented a retrospective cohort of 20 patients with a mean follow-up of 17 years, 69 patients operated on initially. Their methods differed from this series with the function scores used (Mayo Wrist Score and the Michigan Hand Outcomes Score) [6]. Three Kirschner wires were used for the FCA.
| Authors | Patients, n | Age (years) | Radial deviation (degrees) | Ulnar deviation (degrees) | Flexion (degrees) | Extension (degrees) | Mobility (%) | Strength compared to the contralateral side (%) | |
| Aita et al. [28] | FCA | 14 | 40.4 | – | – | – | – | 58 | 65 |
| PRC | 13 | 32.4 | – | – | – | – | 68.5 | 78.5 | |
| Berkhout et al. [6] | FCA | 8 | 45 | 16° | 17° | 36° | 36° | – | – |
| PRC | 14 | 40 | 10° | 29° | 46° | 51° | – | – | |
| Vanhove et al. [30] | FCA | 15 | 38 | 11° | 19° | 40° | 30° | – | 71 |
| PRC | 15 | 45 | 19° | 25° | 42° | 38° | – | 77 | |
| Present study | FCA | 14 | 53 | 18° | 21° | 39° | 32.5° | 59 | 72 |
| PRC | 11 | 66 | 14° | 22° | 30° | 29.5° | 62.5 | 62 | |
| FCA: Four-corner arthrodesis and scaphoid excision; PRC: First-row carpal resection; –: unknown. | |||||||||
One of the strengths of Berkhout et al. [6] was the average age of their patients (Table 3) corresponding to a population of active workers. The 17-year follow-up is a key point because it provided the data needed to evaluate the conversion rate to TWA. Their series showed 27 and 7% conversion for the FCA and PRC groups, respectively.
Their study had several limitations. The lack of information regarding the date of onset of radiocarpal osteoarthritis and its conversion to post-PRC TWA is a key point that would have been complementary to our study. Their clinical results were similar to this series (Tables 2 and 3). They showed that both procedures were reliable over time but that FCA had some disadvantages including prolonged immobilization and pin removal.
The study by Aita and al. [28] did not find any difference between the two groups for strength, function and mobility. The Quick Dash score was calculated at 11 for the FCA group and 13 for the PRC group. Their complication rate was 7.1% for the FCA group with an asymptomatic pseudarthrodesis that was not revised. Their complication rate was 7.7% for the PRC group due to symptomatic radiocapital osteoarthritis, revised by TWA.
Their surgical technique for PRC used radial styloidectomy to avoid radial deviation conflict [7,29]. It was performed over 2 mm and the material used was a circular plate with a screw in each bone. It was not described in FCA. Strength results and mobility were superior in PRC without signficant difference. This implies that PRC could be performed in the young, active patient. The age difference was 8 years on average between the two groups (Table 3) does not alone explain these results. The average strength of a dominant hand in the male grip test was 46.1 kg between 30 and 34 years of age and 45.9 kg between 40 and 44 years of age [30].
Vanhove and al. [30] showed identical results to this series for strength, function and mobility in a retrospective, non-randomized study of 30 patients with a mean follow-up of 3.5 years (Figure 2).
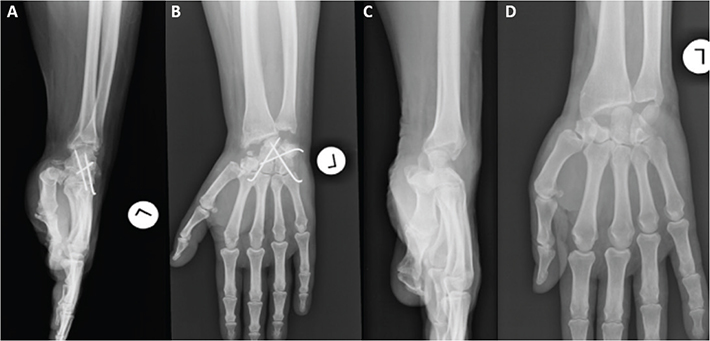
Figure 2. (A and B) Radiographs of arthrodesis of the 4 bones with scaphoidectomies according to their operative technique. (C and D) Radiographs of their first row carpal resection according to their operative technique.
All operated patients had SLAC. For FCA, 3 Kirschner wires of 1.8 mm diameter were used: 2 retrograde, one capitol-lunar, one hamate-lunar, and one anterograde triquetrohamate. They were removed at 3 months with an immobilization of 6 weeks for the FCA and 3 weeks for the PRC. No styloidectomy was performed. Their extension and radial deviation data were lower in FCA without significant difference. These data may be explained by the use of the retrograde approach and the delay in pin removal at 3 months.
In agreement with the study of Aita et al. [28], their strength data showed that PRC gives good results in young patients without significant difference. The duration of time off work (9.8 weeks for PRC vs. 38.6 weeks for FCA) was different result from ours. Their series had 27 active workers out of 30 patients making their result regarding time off work more representative because the proportion of active workers was higher. The follow-up was only 3.5 years.
Limits and biases
The results of this series showed no difference between the two procedures in contrast to the recent meta-analysis [31]. The literature shows that PRC is 70–425% less expensive than FCA [5]. The surgical time is shorter (57 min vs, 121 min) [5], technically less difficult, with a shorter immobilization time ranging from 0 to 3.5 weeks [6–8] versus 2 to 6 weeks [6,9] for PRC and FCA respectively for similar clinical results.
However, our study has limitation, our patients were not randomized. Young and active patients had been indicated FCA by operator’s suggestion, elderly patients had been indicated PRC.
Moreover, the lack of data concerning the strength before the operation is a source of bias, our analysis was made by neither taking into account the dominant wrist nor the operated side. There is a difference in strength between dominant and non-dominant hands of 5–5.6% [32]. The number of active patients was too low (7 out of a total of 25 patients), the functional demand being greater in active patients. The etiologies were SNACs and SLACs. No patient in this series had Kienbock’s disease or chronic perilunate dislocation of the carpus, which are indications for PRC. The mean follow-up of 69.5 months was too short to analyze the rate of revision surgery for conversion to TWA [31]. This was a single-center, single-operator study. The material used for FCA was the LEIBINGER® plate with 2.3 screws. Other methods of arthrodesis were not studied. The statistical power was limited by the small number of patients.
In conclusion, this study found no significant difference between FCA and plate osteosynthesis versus PRC on strength, mobility, and function with a mean follow-up of 69.5 months in patients with post-traumatic SLAC or SNAC stage II wrist arthritis. Both FCA and PRC are reliable interventions with good outcomes with more revision in the FCA group.
Acknowledgments
The authors are grateful to Nikki Sabourin-Gibbs, CHU Rouen, for her help in editing the manuscript.
References
[1] Rimokh J, Benazech B, Lebeau N, et al. Clinical and radiological outcomes of 40 cases of SLAC and SNAC wrist treated by four-corner arthrodesis with locking plate. Hand Surg Rehabil. 2020;39:36–40. https://doi.org/10.1016/j.hansur.2019.10.196
[2] Traverso P, Wong A, Wollstein R, et al. Ten-year minimum follow-up of 4-corner fusion for SLAC and SNAC wrist. HAND. 2017;12:568–572. https://doi.org/10.1177/1558944716681949
[3] Saltzman BM, Frank JM, Slikker W, et al. Clinical outcomes of proximal row carpectomy versus four-corner arthrodesis for post-traumatic wrist arthropathy: a systematic review. J Hand Surg Eur Vol. 2015;40:450–457. https://doi.org/10.1177/1753193414554359
[4] Dacho AK, Baumeister S, Germann G, et al. Comparison of proximal row carpectomy and midcarpal arthrodesis for the treatment of scaphoid nonunion advanced collapse (SNAC-wrist) and scapholunate advanced collapse (SLAC-wrist) in stage II. J Plast Reconstr Aesthet Surg. 2008;61:1210–1218. https://doi.org/10.1016/j.bjps.2007.08.007
[5] Kazmers N, Stephens A, Presson A, et al. Comparison of direct surgical costs for proximal row carpectomy and four-corner arthrodesis. J Wrist Surg. 2019;8:66–71. https://doi.org/10.1055/s-0038-1675791
[6] Berkhout MJL, Bachour Y, Zheng KH, et al. Four-corner arthrodesis versus proximal row carpectomy: a retrospective study with a mean follow-up of 17 years. J Hand Surg. 2015;40:1349–1354. https://doi.org/10.1016/j.jhsa.2014.12.035
[7] Della Santa DR, Sennwald GR, Mathys L, et al. Proximal row carpectomy in emergency. Chir Main. 2010;29:224–230. https://doi.org/10.1016/j.main.2010.06.001
[8] Edouard P, Vernay D, Martin S, et al. Proximal row carpectomy: is early postoperative mobilisation the right rehabilitation protocol? Orthop Traumatol Surg Res. 2010;96:513–520. https://doi.org/10.1016/j.otsr.2010.02.011
[9] Trail I, Murali R, Stanley J, et al. The long-term outcome of four-corner fusion. J Wrist Surg. 2015;4:128–133. https://doi.org/10.1055/s-0035-1549277
[10] Quatman-Yates CC, Gupta R, Paterno MV, et al. Internal consistency and validity of the QuickDASH instrument for upper extremity injuries in older children. J Pediatr Orthop. 2013;33:838–842. https://doi.org/10.1097/BPO.0b013e3182a00688
[11] Shafiee E, MacDermid J, Farzad M, et al. A systematic review and meta-analysis of patient-rated wrist (and hand) evaluation (PRWE/PRWHE) measurement properties, translation, and/or cross-cultural adaptation. Disabil Rehabil. 2022;44:6551–6565. https://doi.org/10.1080/09638288.2021.1970250
[12] van Hernen JJ, Lans J, Garg R, et al. Factors associated with reoperation and conversion to wrist fusion after proximal row carpectomy or 4-corner arthrodesis. J Hand Surg. 2020;45:85–94.e2. https://doi.org/10.1016/j.jhsa.2019.10.023
[13] Le Corre A, Ardouin L, Loubersac T, et al. Retrospective study of two fixation methods for 4-corner fusion: shape-memory staple vs. dorsal circular plate. Chir Main. 2015;34:300–306. https://doi.org/10.1016/j.main.2015.08.008
[14] Wall LB, DiDonna ML, Kiefhaber TR, et al. Proximal row carpectomy: minimum 20-year follow-up. J Hand Surg. 2013;38:1498–1504. https://doi.org/10.1016/j.jhsa.2013.04.028
[15] Tielemans A, Van Innis F, Troussel S, et al. Effect of four-corner fusion with locking plate without bone graft on functional recovery of the wrist: new treatment guidelines. Hand Surg Rehabil. 2017;36:186–191. https://doi.org/10.1016/j.hansur.2017.01.005
[16] Espinoza DP, Schertenleib P. Four-corner bone arthrodesis with dorsal rectangular plate: series and personal technique. J Hand Surg Eur Vol. 2009;34:609–613. https://doi.org/10.1177/1753193409105684
[17] Pham TT, Lenoir H, Coulet B, et al. Proximal row carpectomy in total arthrodesis of the rheumatoid wrist. Orthop Traumatol Surg Res. 2015;101:919–922. https://doi.org/10.1016/j.otsr.2015.09.032
[18] Palmer AK, Werner FW, Murphy D, et al. Functional wrist motion: a biomechanical study. J Hand Surg. 1985;10:39–46. https://doi.org/10.1016/S0363-5023(85)80246-X
[19] Ryu J, Cooney WP, Askew LJ, et al. Functional ranges of motion of the wrist joint. J Hand Surg. 1991;16:409–419. https://doi.org/10.1016/0363-5023(91)90006-W
[20] Jebson PJL, Hayes EP, Engber WD. Proximal row carpectomy: a minimum 10-year follow-up study. J Hand Surg. 2003;28:561–569. https://doi.org/10.1016/S0363-5023(03)00248-X
[21] DiDonna ML, Kiefhaber TR, Stern PJ. Proximal row carpectomy: study with a minimum of ten years of follow-up. J Bone Joint Surg Am. 2004;86:2359–2365. https://doi.org/10.2106/00004623-200411000-00001
[22] Croog AS, Stern PJ. Proximal row carpectomy for advanced Kienböck’s disease: average 10-year follow-up. J Hand Surg. 2008;33:1122–1130. https://doi.org/10.1016/j.jhsa.2008.02.031
[23] Lumsden BC, Stone A, Engber WD. Treatment of advanced-stage Kienböck’s disease with proximal row carpectomy: an average 15-year follow-up. J Hand Surg. 2008;33:493–502. https://doi.org/10.1016/j.jhsa.2007.12.010
[24] Richou J, Chuinard C, Moineau G, et al. Proximal row carpectomy: long-term results. Chir Main. 2010;29:10–15. https://doi.org/10.1016/j.main.2009.10.003
[25] Ali MH, Rizzo M, Shin AY, et al. Long-term outcomes of proximal row carpectomy: a minimum of 15-year follow-up. HAND. 2012;7:72–78. https://doi.org/10.1007/s11552-011-9368-y
[26] Williams J, Weiner H, Tyser A. Long-term outcome and secondary operations after proximal row carpectomy or four-corner arthrodesis. J Wrist Surg. 2018;7:51–56. https://doi.org/10.1055/s-0037-1604395
[27] Garcia BN, Lu C-C, Stephens AR, et al. Risk of total wrist arthrodesis or reoperation following 4-corner arthrodesis or proximal row carpectomy for stage-II SLAC/SNAC arthritis: a propensity score analysis of 502 wrists. J Bone Jt Surg. 2020;102:1050–1058. https://doi.org/10.2106/JBJS.19.00965
[28] Aita MA, Nakano EK, Schaffhausser HDL, et al. Randomized clinical trial between proximal row carpectomy and the four-corner fusion for patients with stage II SNAC. Rev Bras Ortop Engl Ed. 2016;51:574–582. https://doi.org/10.1016/j.rboe.2016.08.008
[29] Chim H, Moran S. Long-term outcomes of proximal row carpectomy: a systematic review of the literature. J Wrist Surg. 2012;1:141–148. https://doi.org/10.1055/s-0032-1329547
[30] Vanhove W, De Vil J, Van Seymortier P, et al. Proximal row carpectomy versus four-corner arthrodesis as a treatment for SLAC (Scapholunate Advanced Collapse) wrist. J Hand Surg Eur Vol. 2008;33:118–125. https://doi.org/10.1177/1753193408087116
[31] Chammas P-E, Hadouiri N, Chammas M, et al. La résection de première rangée des os du carpe permet de meilleurs résultats à moyen et long terme comparés à ceux de l’arthrodèse des quatre os pour l’arthrose du poignet post-traumatique : une méta-analyse. Rev Chir Orthopédique Traumatol. 2022;108:992–1003. https://doi.org/10.1016/j.rcot.2022.07.012
[32] Bohannon RW, Wang Y-C, Yen S-C, et al. Handgrip strength: a comparison of values obtained from the NHANES and NIH toolbox studies. Am J Occup Ther Off Publ Am Occup Ther Assoc. 2019;73:7302205080p1–9. https://doi.org/10.5014/ajot.2019.029538