ORIGINAL RESEARCH ARTICLE
Treatment and rehabilitation of post-traumatic elbow stiffness with heterotopic ossification
Qi Wanga,b, Jiang Pengc, Aiyuan Wangc, Wenjing Xuc, Jinshu Tangd and Jinshu Tangd*
aJinzhou Medical University, Jinzhou, Liaoning, China; bRehabilitation Center, Beijing Rehabilitation Hospital Affiliated to Capital Medical University, Beijing, China; cInstitute of Orthopedics, Chinese PLA General Hospital, Beijing Key Laboratory of Regenerative Medicine in Orthopedics, Key Laboratory of Musculoskeletal Trauma & War Injuries PLA, Beijing, China; dDepartment of Orthopedic Surgery, Fourth Medical Center, Chinese PLA Gen Hospital, Beijing, China
ABSTRACT
Aim: To investigate surgical treatment, postoperative rehabilitation and prevention of heterotopic ossification (HO) in patients with post-traumatic elbow stiffness.
Methods: We performed a retrospective review of patients with post-traumatic elbow stiffness combined with HO between 2007 and 2021. This study was performed on a total of 15 patients (18 elbows) admitted to our hospital, consisting of 12 males and 3 females, with post-traumatic stiffness of the elbow combined with HO, where elbow function could not be recovered by rehabilitation and orthosis treatment. Fifteen patients were treated by surgical excision of heterotopic bones and release of elbow contracture combined with postoperative rehabilitation and orthosis-wearing. Comprehensive treatments, including radiation, oral ibuprofen medication, and manipulation techniques to improve range of motion, were used to prevent HO recurrence. The flexion–extension arc and functional score of the elbow were measured after treatment and compared with the preoperative measurements. Roentgenography was used to observe HO recurrence.
Results: After surgical treatment and postoperative rehabilitation, the patients’ range of motion improved, and the functional score improved considerably. The postoperative flexion-extension arc and The Hospital for Special Surgery (HSS) functional score were statistically significantly higher than the preoperative values (p < 0.01). Roentgenographic examination showed no HO recurrence during the follow-up period.
Conclusion: Surgical excision of heterotopic bones and elbow contracture release combined with postoperative rehabilitation and preventative HO measures can be an effective treatment for cases of post-traumatic elbow stiffness combined with HO, for which conservative treatment is ineffective.
KEYWORDS: Post-traumatic stiffness of the elbow; Heterotopic ossification; Surgical treatment; Early rehabilitation
Citation: Journal of Plastic Surgery and Hand Surgery 2024; 59: 18–23. DOI: https://doi.org/10.2340/jphs.v59.18363.
Copyright: © 2024 The Author(s). Published by MJS Publishing on behalf of Acta Chirurgica Scandinavica. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material, with the condition of proper attribution to the original work.
Received: 4 August 2023; Accepted: 21 November 2023; Published: 4 February 2024
CONTACT Dr. Jinshu Tang drtang304@sina.com Department of Orthopedic Surgery, Fourth Medical Center, Chinese PLA Gen Hospital, Beijing, 100048, China
Introduction
Post-traumatic elbow stiffness is a common complication among patients with injuries or burns to the elbow joint and the surrounding tissues that leads to limited flexion and extension of the elbow joint, and even limited forearm rotation in some patients, thus severely affecting patients’ daily activities. Heterotopic ossification (HO) is one of the most important causes of post-traumatic elbow stiffness. In general, for patients with stiff elbow joint injuries and mild HO who can still perform elbow joint function training, it is recommended that elbow joint function be restored through rehabilitation training, being careful of the intensity of manual treatment. However, for patients with post-traumatic elbow stiffness and severe HO or patients with nonsevere HO during preoperative examination but with poor long-term treatment effects, the usual recommendation is surgical excision of heterotopic bones and elbow contracture release. However, there is still much controversy regarding the timing of surgical resection, postoperative elbow functional training techniques, and measures to prevent HO recurrence [1–3]. Since 2007, we have simultaneously performed surgical excision of heterotopic bones and elbow contracture release to treat patients with post-traumatic elbow stiffness and HO, along with using active rehabilitation therapy early after surgery to restore elbow function. Combining radiotherapy and oral drug therapy, as well as making corresponding changes in rehabilitation training techniques, can comprehensively prevent HO recurrence. So, the purpose of this study was to analyze the effect of post-traumatic stiffness by taking operation and postoperative rehabilitation.
Materials and methods
General information
From February 2007 to November 2021, we performed surgical release on 17 patients (20 elbows) who were unable to recover functional elbow stiffness through rehabilitation and brace treatment, among which 15 cases (18 elbows) were associated with various degrees of HO, accounting for 90% (18/20) of the total number of treated elbows. Among the 15 patients with HO and elbow stiffness, 12 were male and 3 females, with the age range of 21–62 (mean 41.1 years). The stiffness time ranged from 6 to 36 months, with an average of 15.1 months. The cases were classified by injury type as follows: two cases of olecranon fracture, one case of distal humerus fracture, one case of olecranon fracture combined with distal humerus fracture, three cases of soft tissue injuries around the elbow, and eight cases of elbow stiffness and HO secondary to large-area burns, including a case of bony ankylosis. The fractures were treated with open reduction and internal fixation (ORIF). Three olecranon fractures were fixed with tension band wiring or plate fixation, and two distal humerus fractures with plate fixation. The causes for injury were classified as follows: two vehicle accidents, four falls, eight burns, and one cutting injury. HO was diagnosed in 14 out of 15 patients (Figure 1) and was not found through preoperative X-ray on the other patient. However, bony tissue was found in the posterior region of elbow during intraoperative release for the patient without HO, which confirmed to be cartilage tissues by postoperative pathological examination (Figure 2). HO was found in the anterior region in only 1 case, in the posterior region in 6 cases, and in the medial region in 11 cases. The severity of HO in 17 elbows was determined according to the Hasting and Graham classification [4]. Class I (n = 0): Radiographic evidence without functional deficit; Class IIA (n = 15): Radiographic evidence with limitation in the flexion–extension axis; Class IIB (n = 0): Radiographic evidence with limitation in the pronation–supination axis; Class IIIA (n = 2): Ectopic bone formation and ankylosis of the joint in the flexion–extension axis; Class IIIB (n = 0): Ectopic bone formation and ankylosis of the joint in the pronation–supination axis; Class IIIC (n = 0): Ectopic bone formation and ankylosis of the joint in the pronation–supination and flexion–extension axes (Table 1). Flexion and extension dysfunction to different degrees was also discovered in most patients (Figure 3). The preoperative flexion–extension arc of the elbow ranged from 0° to 70°, with an average of 22.8°. The functional score ranged from 39 to 72 points, with a mean of 51.6 points. Elbow flexion ranged from 0 to 90 degrees, with a mean of 46.1 degrees. A written informed consent was obtained from each patient.
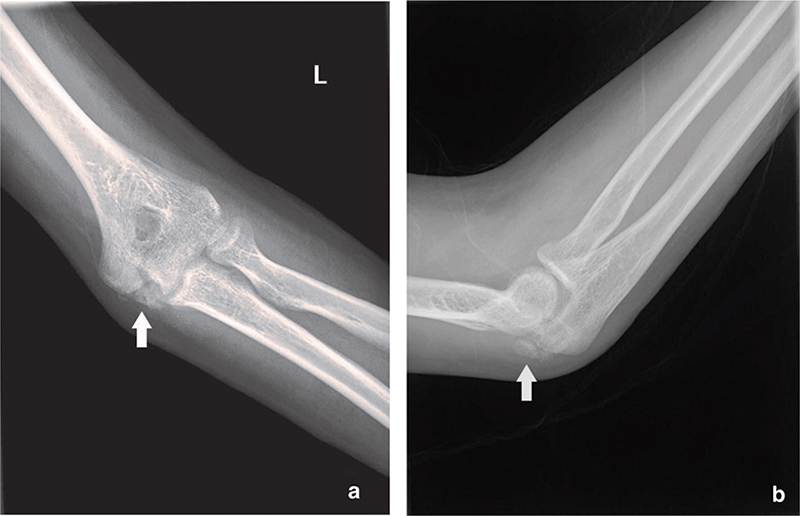
Figure 1. The preoperative radiograph showed HO in the medial and posterior elbow, as indicated by the arrows. (a) The X-ray shows HO on the ulnar side of the elbow joint in the anteroposterior projection. (b) The X-ray shows HO on the ulnar side of the elbow joint in the lateral projection.
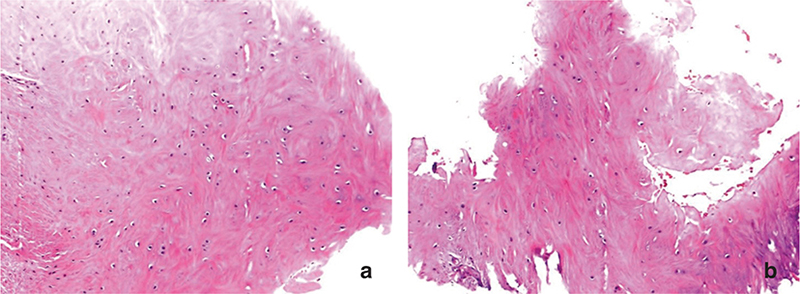
Figure 2. X-ray examination of a patient did not reveal HO, but pathological examination after surgery indicated that the submitted sample contained bone.
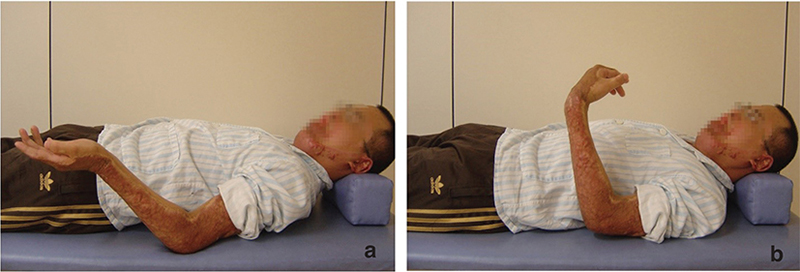
Figure 3. Preoperative examination showed limited degrees of flexion–extension arc of the elbow. (a) Preoperative observation of clear extension problems with the elbow joint. (b) The range of motion for active flexion of the joint is significantly limited.
Ethical statement
This study was conducted in accordance with the declaration of Helsinki. This study was conducted with approval from the Ethics Committee of the Fourth Medical Center of Chinese PLA General Hospital NO: 2022KY059-KS001, and an informed consent was obtained from all patients.
Treatment
Operative method: We used the original surgical incision, and surgical approaches were individualized considering the HO location. The skin and subcutaneous tissues were directly incised to the deep fascia and muscles, and entry through the intermuscular space was used to expose the joint capsule and HO. Resection of heterotopic bones affects elbow motion (Figure 4) and incises the contracture joint capsule tissues. Passive flexion and extension of the elbow joint can be performed many times during the release process to explore possible factors of stiffness, which should be subsequently eliminated. When performed, passive flexion and extension should be gentle, and the use of force should be avoided. The drainage tube is conventionally placed during surgery. A patient-controlled analgesia pump should be installed immediately after operation.
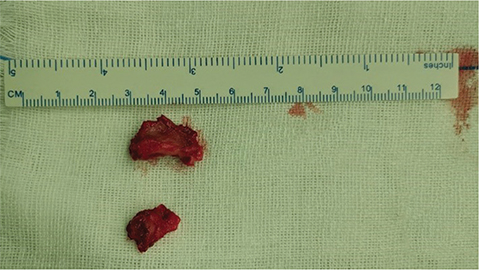
Figure 4. Heterotopic bones were resected during operation.
Postoperative management and rehabilitation: All patients performed exercises for isometric contraction of limb muscles when pain-free on the 2nd postoperative day, if the wound was stable after surgery. To increase the range of motion of the elbow, patients also received gentle active and passive function training after the removal of the drainage tube and continued to perform muscle-strength training for elbow flexion and extension. A professional rehabilitation team administered comprehensive rehabilitation treatment. The patients were strongly encouraged to carry out active training to increase the range of joint motion. Adjuvant therapy with semiconductor laser irradiation and intermediate frequency electrotherapy were also performed to relieve pain, relax adhesion, and promote tissue repair. Stitches were removed 2 weeks after operation. For patients whose straightening or flexion angles were not progressing significantly, the elbow joint was fixed for 2–6 h a day at the maximum extension or flexion angle reached during rehabilitation training with an orthosis made of low-temperature thermoplastic panels to help improve the range of joint mobility (Figure 5).
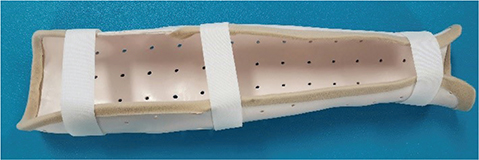
Figure 5. The orthosis employed for extension.
Measures to prevent HO recurrence: (1) Radiation therapy at 500–800 rad was performed once within 24 h before operation. Three patients (4 elbows) received radiation therapy once within 24 h before operation, and the two patients with severe HO received an additional single dose of radiation therapy of 500–800 rad after operation. The patient for whom HO was observed during operation received radiation therapy once within 24 h after operation. (2) Patients were administered 0.2 g of ibuprofen three times daily for 2–3 months postoperatively. If gastrointestinal reactions occurred while under medication, the medication was accordingly discontinued. (3) For passive joint activity training in rehabilitation therapy, gentle manual treatment was used to prevent excessive pain reactions, and routine cold compressions were administered for 15 to 20 minutes after training. (4) Joint physiotherapies with thermogenic factors, such as wax therapy and infrared radiation therapy, were avoided, and nonheating semiconductor laser irradiation and intermediate frequency electrotherapy were recommended.
Functional assessment
The flexion-extension arc and functional score of the elbow joint were measured after treatment and compared with the measurements before treatment. The Hospital for Special Surgery (HSS) elbow assessment scoring system (with a maximum score of 100) was used to assess elbow joint function, including pain, function, range of motion in the sagittal plane, muscle strength, flexion contracture, extension contracture, pronation, and supination. X-ray examination was performed to observe HO recurrence in the elbow joint and adjacent tissues.
Statistical analysis
The paired-samples t-test was used to determine statistical significance, and the categorical variables were compared by chi-square test. We considered p < 0.05 to be statistically significant and used two-sided tests.
Results
We analyzed the differences of location and extent of HO between burns and other traumas and found that the locations of burn-induced Hos mainly located in the medial side of the elbow, whereas HOs caused by other traumas, such as fractures and soft tissue injuries, generally located in the posterior side (p < 0.01) (Table 2). The severity of HO was not statistically significant between burns and other traumas (p > 0.05) (Table 2). All the patients’ incisions healed well. After surgical treatment and postoperative rehabilitation, joint function was significantly improved (Figure 6). The follow-up time ranged from 3 to 52, with a mean of 31.2 months. The elbow flexion–extension arc after treatment ranged from 75° to 140°, with a mean of 105.8°. The functional score of the elbow joint ranged from 64 to 100 points, with a mean of 88.7 points. The increase in both the flexion–extension arc and functional score of the elbow joint after treatment was statistically significant (p < 0.01) (Table 3). Roentgenographic examination showed no HO recurrence during the follow-up period (Figure 7).
| Burns | Others | χ2 | p | ||
| HO Location (n = 18) | 18.635 | 0.000 | |||
| medial | 11 | 0 | |||
| lateral | 0 | 0 | |||
| anterior | 0 | 1 | |||
| posterior | 0 | 6 | |||
| Extent of HO (n = 17†) | - | 1.000 | |||
| IIA | 10 | 5 | |||
| IIIA | 1 | 1 | |||
| †n = 17, patient with chondrogenic ossification was excluded due to no preoperative X-ray evidence. | |||||
| Preoperative | Follow-up | p | |
| Flexion-Extension Arc | 22.8 ± 18.8 | 105.8 ± 20.8 | 0.000<0.01 |
| HSS Score | 51.6 ± 8.1 | 88.7 ± 9.5 | 0.000<0.01 |
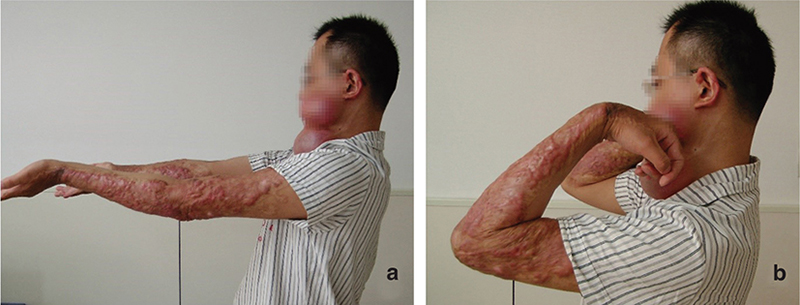
Figure 6. Postoperative active joint range of motion. (a) There was clear improvement in the elbow extension after operation. (b) The range of motion of elbow joint flexion was significantly improved after operation.
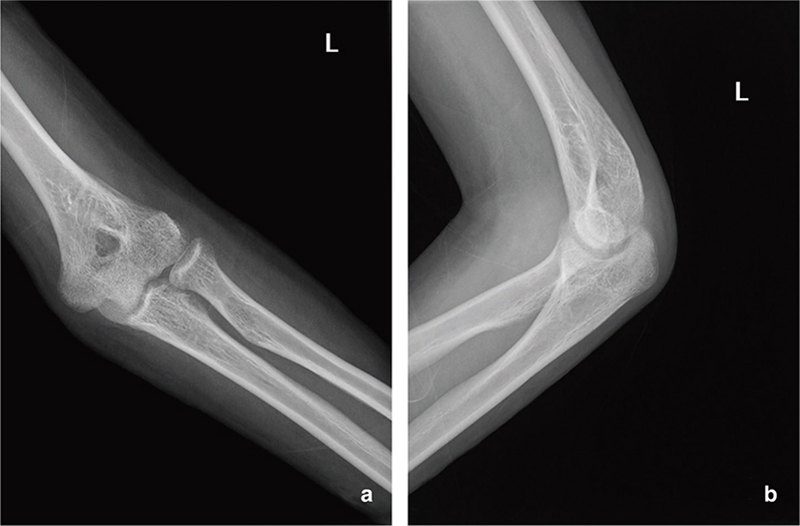
Figure 7. At follow-up, X-ray examination showed no HO recurrence, either in the anteroposterior projection (a) or the lateral projection (b).
Discussion
Fractures, dislocations, soft tissue injuries, and burns of the elbow joint can cause elbow joint stiffness, commonly known as post-traumatic elbow stiffness [5]. The main manifestations of elbow joint stiffness include that the elbow joint and its surrounding tissues become indurated and contracted and lack softness and ductility, and there is limited flexion and extension of the elbow joint, combined with forearm rotation dysfunction in a few patients. The main pathological basis of post-traumatic elbow stiffness is the formation of scars around the joint caused by injury or surgery and the shortening of soft tissues around the joint caused by long-term immobilization, and HO of the tissues around the joint is also a very important pathological factor [6,7]. HO is commonly observed in limb joints suffering severe trauma, burns, and central-nervous-system injury and mainly occurs in the knee and hip joints and, in particular, the elbow joint. Currently, the pathogenesis of HO is still not fully understood, and various theories have been put forward. The reaction after local tissue damage, local immobilization, limb spasticity, etc. plays a central role in the development of HO. It has been suggested that HO in patients with severe local trauma is related to an increase in local endogenous bone morphogenic protein, fibroblast growth factors, and other biological factors that facilitate bone formation [8–10]. However, this theory makes it difficult to explain why HO occurs in limb joints with central-nervous-system injury. Although HO formation involves many factors, restricted activity or immobilization may be a very important coexisting factor. This factor mainly includes two aspects. One is the limitation of movement caused by various internal and external fixations required for treatment; the other is the active pain resulting from severe trauma and burns and the limitation of passive movement by increased muscle tension of the limbs resulting from injury to the central nervous system.
For patients with post-traumatic elbow stiffness combined with HO who need surgical treatment, it is important to determine when to perform surgical excision of heterotopic bones and how to perform intraoperative release of elbow contracture. It is generally believed that it is necessary to wait until the heterotopic bones become mature to perform surgical excision. However, it is difficult to establish a unified standard for heterotopic bone maturity in clinical practice. Surgical excision is generally performed at least 8 months after the diagnosis of heterotopic bones, and laboratory test results, such as erythrocyte sedimentation rate, C-reactive protein, and alkaline phosphatase, must be normal [11,12]. Another problem that should be noted is that, in most cases, joint stiffness tends to be last longer when surgical excision is performed after heterotopic bones are mature. Contracture and shortening of the joint capsule, ligaments around the joint and muscle, and tendon tissues must be observed at the time of release. Therefore, surgical treatment of post-traumatic elbow stiffness combined with HO should consist not only of resection of the heterotopic bones affecting the range of joint motion but also the release of the contracture and shortening of the joint capsule and the soft tissues around the joint to create good conditions for postoperative rehabilitation of joint function [11,13,14]. In addition, we observed a very important clinical phenomenon: once ectopic ossification has resulted in complete ankylosis of the elbow joint, disappearance and fibrosis of articular cartilage are imminent. Therefore, we suggest that heterotopic bone be removed as soon as possible to avoid joint fusion and disappearance of articular cartilage and further affect the treatment effect, irrespective of 8 months maturity of heterotopic bone.
Despite the excellent range of passive motion of a joint resulting from surgical excision of heterotopic bone and soft-tissue loosening, postoperative rehabilitation is still considered to be a very difficult process. The main manifestations of this difficulty are as follows: (1) the patient feels pain during the training process, and the active and passive ranges of motion decrease soon after operation; (2) the ductility and compliance of the soft tissues around the joints make it necessary to wait to perform rehabilitation until sufficient stretching and functional activities have been performed. As joint recovery takes a long time, there is a very clear rebound of the joint range of motion. The patient’s range of motion increases immediately after training but returns to its original level after a night’s rest. This behavior often confuses therapists as well as patients, who sometimes even lose confidence in recovery. In rehabilitation training, priority should be given to restoring flexion function, when necessary, to ensure that patients can perform some functional activities as soon as possible to enhance their confidence in rehabilitation [15]. To alleviate the rebound degree, a static orthosis made of a low-temperature thermoplastic plate can be used after joint-motion training to significantly increase the time of tissue remodeling and promote the gradual extension of the structures around the elbow joint. A characteristic feature of an orthosis made of the aforementioned material is that the angle of the orthosis can be adjusted over time by heating and shaping according to the progress of the patient’s joint motion, which can promote rehabilitation. The orthosis should be worn intermittently. Intermittent fixation of the orthosis can increase the length of time that shortened tissues lacking ductility can be maintained in a drawn state, thereby increasing tissue ductility as soon as possible and reducing the rehabilitation time. Another advantage of intermittent fixation is that the restoration of a different orthosis angle is not affected by external fixation of the orthosis during the night and removal the next morning to carry out extension or flexion training.
Preventing the recurrence of ectopic bone is an important and arduous task in the treatment of patients with elbow stiffness. We successfully prevented the recurrence of ectopic ossification by combining administration of oral ibuprofen for 2–3 months [3] with the protection of soft tissue during operation, thorough drainage of hemorrhage after operation, and attention to the training strength of passive joint motion after operation. It has been reported in many studies that a single dose of radiation can effectively prevent the occurrence of HO or recurrence after heterotopic osteotomy [16,17]. However, only three patients in this group were treated with preoperative or postoperative radiotherapy to prevent the recurrence of HO, whereas none of our patient’s experienced recurrence of HO. Therefore, it is difficult for us to make a comprehensive and accurate evaluation of the effect of radiotherapy. Note that there is no problem with fracture healing in patients treated with radiation and oral ibuprofen, whereas radiation may otherwise affect the final healing of a fracture [18]. Neither a definite conclusion nor research reports have been published regarding the causal relationship between HO and the passive motion of the elbow joint. The purpose of passive motion is quite clear, that is, shortening of the elbow joint capsule and the surrounding soft tissues. The problem of shortened tissues must be resolved through mechanical drawing by passive motion, whereas the use of active motion is currently often very limited in rehabilitation and sometimes even ineffective. However, there is a consensus that the use of excessive external force during the rehabilitation of the elbow joint should be avoided in case of an increased risk of HO in the soft tissues around the joint. Our treatment experience has shown that satisfactory therapeutic effects can be achieved by controlling the intensity of passive motion and degree of pain experienced by the patient in combination with applying ice compresses after training based on reasonable physical factors; thus, the incidence of HO caused by passive motion is effectively reduced and can even be prevented.
However, this study has some limitations. The number of cases was small, so the distribution characteristics of HO in the elbow joint due to different causes were not analyzed. Additionally, this study applied multiple measures to prevent HO recurrence and reconstruct elbow function, and it was not possible to analyze the role of a single measure. Therefore, we will enroll more patients and optimize the study protocol in further study, to observe the important role of HO in causing post-traumatic elbow stiffness and find out more targeted preventive measures.
Conclusion
Most of traumatic elbow stiffness that required surgical release is combined with heterotopic or chondrolated heterotopic bone formation. Surgical excision of heterotopic bones and elbow contracture release combined with postoperative rehabilitation and preventative HO measures can be an effective treatment for cases of post-traumatic elbow stiffness combined with HO for which conservative treatment is ineffective.
References
[1] Adolfsson L. Post-traumatic stiff elbow. EFORT Open Rev. 2018;3(5):210–216. https://doi.org/10.1302/2058-5241.3.170062
[2] Chen S, Yu SY, Yan H, et al. The time point in surgical excision of heterotopic ossification of post-traumatic stiff elbow: recommendation for early excision followed by early exercise. J Shoulder Elbow Surg. 2015;24(8):1165–1171. https://doi.org/10.1016/j.jse.2015.05.044
[3] Haglin JM, Kugelman DN, Christiano A, Konda SR, Paksima N, Egol KA. Open surgical elbow contracture release after trauma: results and recommendations. J Shoulder Elbow Surg. 2018;27(3):418–426. https://doi.org/10.1016/j.jse.2017.10.023
[4] Bai J, Kuang Z, Chen Y, Hang K, Xu J, Xue D. Serum uric acid level is associated with the incidence of heterotopic ossification following elbow trauma surgery. J Shoulder Elbow Surg. 2020;29(5):996–1001. https://doi.org/10.1016/j.jse.2020.01.071
[5] Zhang Z, Zhang Y, Wang Z, Qiu X, Chen Y. Incidence of and risk factors for the development of asymptomatic heterotopic ossification after elbow fracture fixation. J Int Med Res. 2020;48(2):300060519877324. https://doi.org/10.1177/0300060519877324
[6] Viveen J, Doornberg JN, Kodde IF, et al. Continuous passive motion and physical therapy (CPM) versus physical therapy (PT) versus delayed physical therapy (DPT) after surgical release for elbow contractures; a study protocol for a prospective randomized controlled trial. BMC Musculoskelet Disord. 2017;18(1):484. https://doi.org/10.1186/s12891-017-1854-0
[7] Meyer HL, Burggraf M, Polan C, Husen M, Dudda M, Kauther MD. Lollipop sign – ossification at wire ends after osteosynthesis? J Orthop Case Rep. 2019;9(2):52–55.
[8] May RD, Frauchiger DA, Albers CE, et al. Application of cytokines of the bone morphogenetic protein (BMP) family in spinal fusion – effects on the bone, intervertebral disc and mesenchymal stromal cells. Curr Stem Cell Res Ther. 2019;14(8):618–643. https://doi.org/10.2174/1574888X14666190628103528
[9] Katagiri W, Osugi M, Kawai T, Hibi H. Secreted frizzled-related protein promotes bone regeneration by human bone marrow- derived mesenchymal stem cells. Int J Mol Sci. 2015;16(10):23250–23258. https://doi.org/10.3390/ijms161023250
[10] Joshi AA, Padhye AM, Gupta HS. Platelet derived growth factor-BB levels in gingival crevicular fluid of localized intrabony defect sites treated with platelet rich fibrin membrane or collagen membrane containing recombinant human platelet derived growth factor-BB: a randomized clinical and biochemical study. J Periodontol. 2019;90(7):701–708. https://doi.org/10.1002/JPER.18-0496
[11] Manske MC, Hanel DP. Postburn contractures of the elbow and heterotopic ossification. Hand Clin. 2017;33(2):375–388. https://doi.org/10.1016/j.hcl.2016.12.014
[12] Chen JY, Fu CW, Ho HY, Lu YC. Surgical treatment of postburn heterotopic ossification around the elbow: Three case reports. Medicine (Baltimore). 2019;98(6):e14403. https://doi.org/10.1097/MD.0000000000014403
[13] Chen S, Liu J, Cai J, et al. Results and outcome predictors after open release of complete ankylosis of the elbow caused by heterotopic ossification. Int Orthop. 2017;41(8):1627–1632. https://doi.org/10.1007/s00264-016-3395-9
[14] Piper SL, Lattanza LL, Shen TS, Wall LB, Goldfarb CA. Open surgical release of posttraumatic elbow contracture in children and adolescents. J Pediatr Orthop. 2019;39(5):241–246. https://doi.org/10.1097/BPO.0000000000000923
[15] Cancio JM, Rhee P. Therapeutic management of the posttraumatic stiff elbow after open osteocapsular release. Tech Hand Up Extrem Surg. 2018;22(4):134–136. https://doi.org/10.1097/BTH.0000000000000207
[16] Morcos M, Smith K, Tanzer M. The effect of late radiotherapy on the progression of heterotopic ossification following total hip arthroplasty. Eur J Orthop Surg Traumatol. 2018;28(6):1125–1131. https://doi.org/10.1007/s00590-018-2185-z
[17] Georhakopoulos I, Kouloulias V, Kougiountzopoulou A, et al. Radiation therapy for the prevention of heterotopic ossification: efficacy and toxicity of single fraction radiotherapy. Orthop Rev (Pavia). 2020;12(2):8577. https://doi.org/10.4081/or.2020.8577
[18] Hu ZH, Chen W, Sun JN, et al. Radiotherapy for the prophylaxis of heterotopic ossification after total hip arthroplasty: a systematic review and meta-analysis of randomized controlled trails. Med Dosim. 2021;46(1):65–73. https://doi.org/10.1016/j.meddos.2020.07.010