ORIGINAL RESEARCH ARTICLE
Retrospective analysis of scaphoid trapezium pyrocarbon implant intervention in STT arthritis: a 3-year follow-up study
Maria Zandera,b , Allan Ibsen-Sörensena,b, Anders Nilssona,b and Anders Björkmana,b
, Allan Ibsen-Sörensena,b, Anders Nilssona,b and Anders Björkmana,b
aDepartment of Hand Surgery, Sahlgrenska University Hospital, Gothenburg, Sweden; bDepartment of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden
ABSTRACT
Aim: The purpose of this study was to evaluate clinical, patient rated and radiological outcome of the scaphoid trapezium pyrocarbon implant (STPI) at a minimum of three years follow-up.
Methods: Consecutive patients operated with the STPI due to scaphotrapeziotrapezoidal (STT) arthritis between 2012 and 2019 were included. Patients were evaluated preoperatively and annually after surgery for range of motion, grip strength, key pinch, quick-DASH, pain, and satisfaction. Radiographs were evaluated for implant position, signs of dorsal intercalated segment instability (DISI), capitolunate (CL) angle, scapholunate (SL) distance, and presence of osteophytes.
Results: Twenty-six patients (29 implants) were included. Seven implants were revised during the follow up, mainly due to pain: three implants were removed, four patients received a new STPI of a different size, leaving 22 implants in 20 patients available for follow up, 9 males and 11 females. Median age was 61.7 years (51–78 years). Median follow-up time was 68 months (37–105 months). Comparing preoperative status to the last follow-up, wrist extension and deviation, thumb abduction, and grip strength did not change. Key Pinch, quick DASH, pain, and patient satisfaction improved significantly at last follow-up. Radiographic signs of DISI were seen in six cases preoperatively and in 12 cases at last follow-up.
Conlusion: At a minimum of three years follow-up, the STPI used for STT-arthritis improve pain, quick-DASH result, and patient satisfaction significantly. ROM and grip strength did not change compared to preoperative values. Radiographic signs of carpal instability were common at the follow-up and the revision rate was high.
KEYWORDS: STT-arthritis; pyrocarbon; STPI; scaphotrapeziotrapezoidal; pyrocarbon implant.
Citation: Journal of Plastic Surgery and Hand Surgery 2024; 59: 40–45. DOI: https://doi.org/10.2340/jphs.v59.34985.
Copyright: © 2024 The Author(s). Published by MJS Publishing on behalf of Acta Chirurgica Scandinavica. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material, with the condition of proper attribution to the original work.
Received: 15 December 2023; Accepted: 14 February 2024; Published: 02 April 2024
CONTACT Maria Zander maria.zander@vgregion.se Department of Hand Surgery, Sahlgrenska University Hospital, SE-413 45 Gothenburg, Sweden
Competing interests and funding: The authors report there are no competing interests to declare.
Introduction
Osteoarthritis in the joint articulation between the scaphoid, trapezium, and trapezoid (STT-OA) is the second most common location of arthritis in the wrist; next to CMC 1 osteoarthritis. It is more common in women and the prevalence increases with age [1]. The etiology of STT-OA is not completely understood, but heredity and prior joint injury are suggested risk factors [2]. In addition, carpal instability, especially a dorsal intercalated segment instability (DISI), has been shown to be associated with STT-OA [3, 4]. However, most cases of STT-OA are idiopathic.
The true incidence of STT-OA is unclear. Radiographic signs of STT-OA have been shown in between 1 and 16% of adults seeking hospital care due to a different hand problem. However, cadaveric studies have shown that STT-OA may be underestimated on radiographs [5]. In addition, there is a poor correlation between radiological STT-OA and clinical symptoms [1].
Patients with symptomatic STT-OA are most often treated conservatively with non-steroid anti-inflammatory drugs (NSAID), orthosis, and occasionally corticosteroid injections. For those not responding to conservative treatment, surgical options include STT-fusion, excision of the distal pole of the scaphoid, excision of the trapezium, and implant arthroplasty [6–8].
STT-fusion changes carpal dynamics, leading to decreased ROM and a change of load transfer from the hand to the wrist [9]. Most studies on outcome after STT-fusion include a wide variety of diagnoses, and results vary extensively. STT-fusion has become a less common solution [6, 10]. Trapeziectomy with or without partial resection of the trapezoid is a common treatment but has a lengthy rehabilitation period [11]. Furthermore, trapeziectomy, as well as excision of the distal scaphoid, has the potential to cause carpal instability, which could be problematic since patients with STT-OA often show signs of carpal instability and a trapeziectomy or excision of the distal scaphoid could thus increase instability further [3, 12, 4, 8, 13].
An interposition arthroplasty placed in the STT-joint has the advantage of maintaining scaphoid mobility and length and keep the STT ligaments intact thus preserving normal carpal kinematics. The STPI (Scaphoid Trapezium Pyrocarbon Implant) has shown favorable results at short-term follow-ups in small cohorts (8–15 patients) [14–18], but there are no long-term results available.
The aim of this study was to evaluate clinical, patient rated, and radiological outcome at a minimum of three years after interposition arthroplasty using the STPI for STT-OA.
Methods
Patients
Consecutive cases operated for STT-OA with the scapho-trapezium pyrocarbon implant, STPI (BIOprofile, Tornier, France) from 2012 to 2019 were included. All cases had clinical and radiological STT-OA where conservative treatment had proven inadequate. Inflammatory joint disease was an exclusion criterion, but this did not cause any dropouts.
Twenty-nine STPI implants with a minimum of three years follow-up were identified in 26 patients, 10 males and 16 females. Median age was 61.5 years (range 51 to 78 years) at the time of surgery. Two female and one male patient had bilateral STPI implants. Four patients had previous surgery in the same hand as the STPI surgery: two patients had carpal tunnel release, one a previous arthrodesis in the metacarpophalangeal joint in the thumb, and one patient had a previous distal scaphoid excision.
Outcome measures
The STPI was introduced at the department of hand surgery in 2012. At the department, it has been routine to assess patients scheduled for new implant types such as the STPI preoperatively and at annual follow-up visits according to a standardized protocol. Thus, patients operated with the STPI had a preoperative status and postoperative status at annual follow-up, as well as assessment for complications. Patients were assessed for grip strength using a Jamar dynamometer (GMB Medical AB, Stockholm, Sweden), pinch strength using a pinch gauge (B&L Engineering, Santa Ana, USA), and range of motion (wrist flexion and extension, thumb radial, and volar abduction). In addition, patient-rated outcome was assessed using the quick version of the Disability of the Arm Shoulder and Hand questionnaire (q-DASH) [19] as well as visual analog scales (VAS) for assessments of pain and satisfaction) [20]. Preoperative radiographs and radiographs from the follow-up visits were assessed for implant position, osteophyte formation, and signs of carpal instability. Implant position was graded as ‘optimal’ or ‘suboptimal’. As there is no available objective grading system, this is a subjective estimation done by a hand surgeon who did not take part in any of the surgeries and who was blinded for patient outcome. Osteophyte formation was assessed as yes/no. Erosion of the implant on the capitate was assessed as yes/no. Carpal instability was assessed by measuring the SL interval, CL, -and SL angle. DISI was defined as an SL angle over 60° [21].
The study was approved by the Swedish Ethical review authority (2020-05337).
Surgical technique and postoperative regime
All patients were operated under brachial plexus anesthesia and tourniquet control by one of three highly experienced surgeons (level IV according to Tang et al. [22]). A dorsoradial approach was used, and approximately 3 mm was resected from the distal scaphoid. Care was taken not to compromise the volar ligaments in the STT joint. The best fitting of the two available implant sizes [23] was chosen. Implant position and stability in wrist radial/ulnar deviation and volar/dorsal extension were verified by intraoperative fluoroscopy also ensuring that the implant fitted in relation to the capitate. After placing the definitive implant, the capsule was closed using adsorbable sutures and the skin using nonabsorbable sutures.
Postoperatively patients were immobilized with a thumb spica splint with free IP-joint for three weeks. Then rehabilitation was started with several shorter episodes a day with motion exercise without weightbearing. Between training sessions, the patient used a prefabricated orthosis, supporting CMC 1 and STT-joint for an additional three weeks, thereafter gradually increased loadbearing and gradually decreased use of orthosis.
Statistical analysis
IBM SPSS Statistics (Statistical Package for the Social Sciences, version 25 for Mac; IBM Corp., Armonk, NY, USA) was used for the statistical assessment of data. As all of the data was not normally distributed according to the Shapiro–Wilks test, nonparametric tests were used in the analyses. Median values and range are presented. Differences between baseline and follow-up was assessed using the Wilcoxon signed-rank test for paired continuous variables. Any p-value less than 0.05 was considered significant.
Results
Of the 29 original implants, seven implants were revised during the follow-up period (Table 1). In one case, the cause of revision was a dislocation of the implant, the other six revisions were due to pain. All but one were female patients. One patient had revision surgery after 24 months; all the others within the first seven postoperative months. At the revision surgery, three patients had the implant removed followed by a four-corner fusion in one case, trapezium extirpation and tendon interposition in one case, and one case was treated with removal of the prosthesis only. The patient who was treated with prosthesis removal without interposition later developed painful ankylosis and was reoperated with trapezium extirpation and tendon interposition. Four patients were revised to a new implant of another size. Two of the revised implants were later removed due to persisting pain (Table 2).
| Revision cases | No revision | All cases | |
| Median age at time of surgery, years (range) | 60.2 (55–74) | 61.7 (51–78) | 61.5 (51–78) |
| Gender (M/F) = (N) | 1/6 = 7 | 10/12 = 22 | 11/18 = 29 |
| Had previous surgery in same hand (N) | 1 | 3 | 4 |
| DISI preoperatively (yes/no) * | 0/6 | 6/15 | 6/21 |
| DISI at last follow-up (yes/no)** | 4/3 | 12/8 | 16/11 |
| STPI position peroperative image *** optimal/suboptimal | 7/0 | 17/0 | 24/0 |
| STPI position 12 weeks postoperatively optimal/suboptimal | 5/2 | 20/2 | 25/4 |
| DISI: dorsal intercalated segment instability. DISI: Scapholunate angle over 60 degrees. *Missing data on SL-angle preoperatively in two cases. **Missing data on SL-angle postoperatively in two cases due to suboptimal images. ***Missing peroperative immage in five cases |
|||
Except the major revision cases, one patient had a minor revision with removal of osteophytes after 4.5 years. No patients were treated for infection, and there were no other complications recorded.
With the removed and revised implants excluded, the 22 remaining cases (10 males and 12 females) were followed for three years or more with a median follow-up time of 68 months (range 37–105 months). Median age at time for surgery for this group was 61.7 years (range 51–78 years).
When comparing preoperative values with values at the last follow-up, range of motion and grip strength did not change. However, pain decreased, key pinch strength increased, and satisfaction as well as q-DASH improved (Table 3).
| Preoperatively | Last follow-up | p | |
| Grip strength Kg median (range)* | 23.5 (8–62) | 26 (5–58) | 0.84 |
| Key pinch force Kg median (range)* | 4.7 (2–10) | 6.8 (2.3–11.0) | 0.007 |
| Wrist flexion- extension range of motion ° median (range)* | 105° (40–150°) | 97.5° (70–140°) | 0.97 |
| Thumb volar abduction° median (range)* | 42 (30–54) | 40 (35–50) | 0.21 |
| Pain VAS 0–100 in activity median (range)** | 75 (62–100) | 6 (0–77) | <0.001 |
| q-DASH median (range) *** | 52 (20–75) | 32 (0–75) | <0.001 |
| Satisfaction VAS 0–100 median (range)**** | 15 (0–72) | 78 (32–100) | <0.001 |
| q-DASH: quick version of the Disability of the Arm Shoulder and Hand questionnaire; VAS: visual analog scales. * Two missing values preoperatively. ** One missing value preoperatively. *** Three missing values preoperatively. **** Seven missing values preoperatively. |
|||
Osteophyte formation was seen in 10 cases and signs of erosion around the implant in seven cases (Table 4, Figure 3).
| Male cases N = 10 | Female cases N = 12 | Total N = 22 | |
| STPI position optimal/suboptimal | 9/1 | 9/3 | 18/4 |
| Erosion yes/no | 4/6 | 3/9 | 7/15 |
| osteophyte formation trapezium or scaphoid, yes/no | 4/6 | 6/6 | 10/12 |
| DISI yes/no * | 6/3 | 6/5 | 12/8 |
| DISI: dorsal intercalated segment instability. DISI: SL-angle over 60 degrees. *Missing data on SL – angle in two cases. |
|||
Twice as many cases showed DISI at the follow-up as preoperatively. However, patients with DISI did not show worse q-DASH or less strength or satisfaction. There was no gender difference regarding increase in SL-angle (Table 4). Mean and median SL-distance and CL-angle did not change compared to preoperative status (Table 5).
| Preoperative | Last follow-up | p | |
| SL-angle median | 56° | 63° | 0.030 |
| DISI yes/no* | 6/15 | 12/8 | 0.008 |
| SL-distance median | 1.5 mm | 17mm | 0.79 |
| CL-angle median** | 11.6° | 11.7° | 1.0 |
| CL-angle over 15° yes/no | 6/14 | 8/12 | 0.34 |
| DISI: dorsal intercalated segment instability; SL: scapholunate. DISI: Scapholunate angle over 60. * Missing data on SL-angle postoperatively in two cases, preoperatively in one case. ** Missing data on CL-angle preoperative in two cases and postoperatively in two cases. Missing data were due to suboptimal images. |
|||
In the preoperative images, all cases were graded as ‘optimal’ implant position (Figure 1). At the first postoperative follow-up at 12 weeks, 25 cases were graded as having an ‘optimal’ implant position and four cases as having a ‘suboptimal’ implant position. Two of the four implants with “suboptimal” position were later revised and two did not need intervention despite radiologically suboptimal implant position (Table 1).
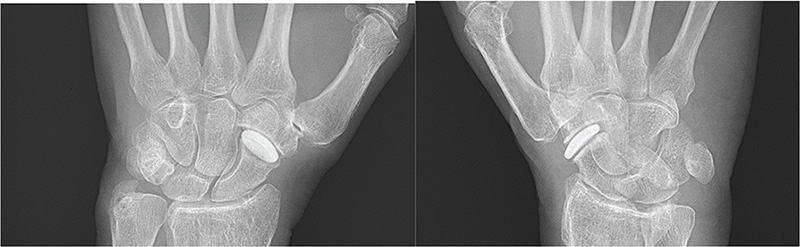
Figure 1. STPI, optimal position.
Discussion
This study shows that the STPI for symptomatic STT arthritis, with a minimum of three years follow-up, provided good pain relief, improved patient rated function, and key pinch strength, whereas ROM and grip strength did not change. However, the revision rate was high.
An interposition implant, such as the STPI, has the mechanical goal to maintain scaphoid mobility and length and preserve carpal stability. The current study corroborates prior smaller studies with shorter follow-ups showing improvement in pain and general function, whereas grip strength and range of motion did not change significantly compared to preoperatively. Previous authors have presented case series of 8, 10, and 15 patients with no complications [16–18]. In addition, Pegoli et al. had two dislocations among 10 cases, and Mathoulin et al also saw two dislocations in 12 cases, which both authors attributed to learning curve issues (too small resection) [14, 15]. The current study had a revision rate of 24% where one revision was due to dislocation and six due to persisting pain. Although there was just one case of dislocation, there were several cases where the implant position was optimal postoperatively but suboptimal on follow-up radiographs, indicating that the implant position sometimes shifts postoperatively meaning that the implant is unstable even if there is no obvious dislocation (Figure 2). Even though the revision rate was high, an advantage with the STPI is that revision surgery is relatively easy. The implant can simply be removed and the STT-joint and conversion to an STT-arthrodesis or a trapeziectomy is possible. We have no explanation for the high revision rate in the current study. All operations were performed by highly experienced surgeons. The revision cases were evenly distributed among the three surgeons and evenly distributed over time, making it less likely that the revisions are simply a learning curve issue. In four cases, the implant was changed to an STPI of another size. Three of the revision cases received a smaller implant and one received a larger size implant. One of the patients who had received a larger implant and one who received a smaller implant were satisfied after the revision, implying that it can be difficult for the surgeon to be confident that size is the correct one, but not that there is a systematic error in sizing. The STPI comes in two sizes, which could make it more difficult to achieve a perfect fitting. Especially in patients with smaller carpal bones such as in women, the fitting may be difficult. This could be an explanation for the fact that all but one of the seven revision cases were female patients. Another possible explanation for female overrepresentation in revisions may be that joint laxity [24], and osteoporosis is more common in women than men, resulting in a mechanical disadvantage. This gender difference in revision rate is interesting and should be assessed in further studies.
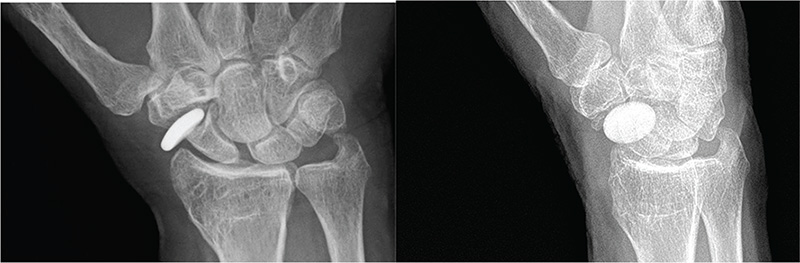
Figure 2. STPI, suboptimal position.
One of the reasons for implanting a prothesis like the STPI, instead of just performing a limited scaphoid resection, is to decrease the risk of carpal instability [8]. Some authors have limited their indication for the STPI to patients with a large SL-angle or a DISI deformity. According to these authors, the STPI improve carpal alignment, give more stability and height to the scaphoid [25, 26]. This assumption that scaphoid is more stable after surgery, is not supported by the present study where 6 patients had DISI before surgery and 12 at the last follow-up. We speculate that the STPI is rather thick and require resection of the distal scaphoid joint surface. This could potentially disturb the distal ligaments and destabilize the scaphoid leading to carpal instability and DISI.
In addition, the STPI has a concave and a convex surface, which may not be the ideal anatomical shape for an interposition arthroplasty as Bellemère and Mathoulin et al also suggest [27, 28]. The round shape might make it less stable than the flatter and thinner shape of, for example, the Pyrocardan implant [29]. In addition, a thinner implant also allows less bone resection entailing a decreased risk of destabilizing the STT-joint.
Signs of carpal instability in the form of increased CL-angle indicating CIND-DISI (carpal instability nondissociative dorsal intercalated segmental instability) has been discussed previously in association with STT-OA [4, 9]. The observed instability in the present study is an increase in SL-angle rather than increased CL-angle. Patients with signs of increased carpal instability preoperatively or postoperatively did not seem to fare worse in terms of worse PROMs or higher risk of revision surgery compared to patients without signs of increased instability. However, we do not know how the increased instability in patients with STPI will affect long-term outcome.
Osteophyte formation was noted around the implant in several cases. We speculate that osteophyte formation in these cases is a sign of joint instability and damage or wear from the implant [30]. We do not know the long-term implications of these osteophytes; however, it is possible that such osteophytes may cause progressive prosthetic instability and pain.
There are several limitations to this study. This is a retrospective follow-up of a cohort of consecutively operated STPI cases. Thus, there were no strict inclusion and exclusion criteria other than that all nonrheumatoid patients who received an STPI-implant during the time period were included. In addition, four of the patients had previous surgery to their hands that could confound the results. Radiographs were not standardized and thus quality of the radiographs varies, and it was not possible to measure CL angle reliably on all radiographs. There are no objective criteria for implant position, and in combination with the nonstandardized radiographs, verification of optimal or suboptimal implant position is subjective. The number of patients is low, but this is still to our knowledge the largest cohort published on the STPI.
Many of the patients experienced good pain relief and had good hand function after surgery with the STPI. However, the reasons for the high revision rate in this study, especially in the female group, should be investigated further. Ideally, a randomized trial between different implants would render the most reliable information, but larger case series from other centers could provide additional information. We believe the principle behind a spacer implant in the STT joint is sound; however, the STPI destabilizes the carpus and the implant design is unstable. We suggest that a different implant design with more inherent stability will prove it easier to obtain consistent satisfactory results.
ORCIDs
Maria Zander:  https://orcid.org/0000-0001-5792-1458
https://orcid.org/0000-0001-5792-1458
References
[1] Wollstein R, Clavijo J, Gilula LA. Osteoarthritis of the Wrist STT Joint and Radiocarpal Joint. Arthritis. 2012;242159. https://doi.org/10.1155/2012/242159
[2] Wu JC, Calandruccio JH. Evaluation and management of scaphoid-trapezium-trapezoid joint arthritis. Orthop Clin North Am. 2019;50(4):497–508. https://doi.org/10.1016/j.ocl.2019.05.005
[3] Scordino LE, Bernstein J, Nakashian M, et al. Radiographic prevalence of scaphotrapeziotrapezoid osteoarthrosis. J Hand Surg Am. 2014;39(9):1677–82. https://doi.org/10.1016/j.jhsa.2014.05.033
[4] Tay SC, Moran SL, Shin AY, et al. The clinical implications of scaphotrapezium-trapezoidal arthritis with associated carpal instability. J Hand Surg Am. 2007;32(1):47–54. https://doi.org/10.1016/j.jhsa.2006.10.021
[5] Brown GD, 3rd, Roh MS, Strauch RJ, et al. Radiography and visual pathology of the osteoarthritic scaphotrapezio-trapezoidal joint, and its relationship to trapeziometacarpal osteoarthritis. J Hand Surg Am. 2003;28(5):739–43. https://doi.org/10.1016/S0363-5023(03)00258-2
[6] Wolf JM, Delaronde S. Current trends in nonoperative and operative treatment of trapeziometacarpal osteoarthritis: a survey of US hand surgeons. J Hand Surg Am. 2012;37(1):77–82. https://doi.org/10.1016/j.jhsa.2011.10.010
[7] Jehan S, Javaid Iqbal H, Javaid MM, et al. The surgical management for isolated scaphotrapeziotrapezoid (STT) osteoarthritis: a systematic review of the literature. Acta Orthop Belg. 2020;86(1):137–45.
[8] Berkhout MJ, Bachour Y, Wessing D, et al. Distal pole resection of the scaphoid for the treatment of scaphotrapeziotrapezoid osteoarthritis. Hand (N Y). 2019;14(2):230–5. https://doi.org/10.1177/1558944717735939
[9] Catalano LW, 3rd, Ryan DJ, Barron OA, et al. Surgical management of scaphotrapeziotrapezoid arthritis. J Am Acad Orthop Surg. 2020;28(6):221–8. https://doi.org/10.5435/JAAOS-D-19-00539
[10] Stephens AR, Garcia BN, Rogers MJ, et al. Scaphotrapeziotrapezoid arthrodesis: systematic review. J Hand Surg Am. 2022;47(3):218–27 e2. https://doi.org/10.1016/j.jhsa.2021.09.029
[11] Saab M, Chick G. Trapeziectomy for trapeziometacarpal osteoarthritis. Bone Jt Open. 2021;2(3):141–9. https://doi.org/10.1302/2633-1462.23.BJO-2020-0188.R1
[12] Ferris BD, Dunnett W, Lavelle JR. An association between scapho-trapezio-trapezoid osteoarthritis and static dorsal intercalated segment instability. J Hand Surg Br. 1994;19(3):338–9. https://doi.org/10.1016/0266-7681(94)90084-1
[13] Garcia-Elias M. Excisional arthroplasty for scaphotrapeziotrapezoidal osteoarthritis. J Hand Surg Am. 2011;36(3):516–20. https://doi.org/10.1016/j.jhsa.2010.12.016
[14] Pegoli L, Zorli IP, Pivato G, et al. Scaphotrapeziotrapezoid joint arthritis: a pilot study of treatment with the scaphoid trapezium pyrocarbon implant. J Hand Surg Br. 2006;31(5):569–73. https://doi.org/10.1016/J.JHSB.2006.05.006
[15] Mathoulin C, Darin F. Arthroscopic treatment of scaphotrapeziotrapezoid osteoarthritis. Hand Clin. 2011;27(3):319–22. https://doi.org/10.1016/j.hcl.2011.05.001
[16] Low AK, Edmunds IA. Isolated scaphotrapeziotrapezoid osteoarthritis: preliminary results of treatment using a pyrocarbon implant. Hand Surg. 2007;12(2):73–7. https://doi.org/10.1142/S0218810407003523
[17] Marcuzzi A, Ozben H, Russomando A. Treatment of scaphotrapezial trapezoidal osteoarthritis with resection of the distal pole of the scaphoid. Acta Orthop Traumatol Turc. 2014;48(4):431–6. https://doi.org/10.3944/AOTT.2014.14.0156
[18] Pequignot JP, D’Asnieres de Veigy L, Allieu Y. Arthroplasty for scaphotrapeziotrapezoidal arthrosis using a pyrolytic carbon implant. Preliminary results. Chir Main. 2005;24(3–4):148–52. https://doi.org/10.1016/j.main.2005.04.010
[19] Atroshi I, Gummesson C, Andersson B, et al. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: reliability and validity of the Swedish version evaluated in 176 patients. Acta Orthop Scand. 2000;71(6):613–8. https://doi.org/10.1080/000164700317362262
[20] Voutilainen A, Pitkaaho T, Kvist T, et al. How to ask about patient satisfaction? The visual analogue scale is less vulnerable to confounding factors and ceiling effect than a symmetric Likert scale. J Adv Nurs. 2016;72(4):946–57. https://doi.org/10.1111/jan.12875
[21] Weerakkody Y. Dorsal intercalated segment instability. Reference article. Radiopaedia [Internet]. 2010 (cited 15-05-2023) Available from https://radiopaedia.org/articles/9709.
[22] Tang JB, Avanessian B. Clinical reports: the importance of reporting a surgeon’s level of expertise. J Hand Surg Am. 2015;40(2):416–7. https://doi.org/10.1016/j.jhsa.2014.10.036
[23] BioProfile. stpi-surgical-technique-technique-chirurgicale-du-stpi. BioProfile.
[24] Wolf JM, Schreier S, Tomsick S, et al. Radiographic laxity of the trapeziometacarpal joint is correlated with generalized joint hypermobility. J Hand Surg Am. 2011;36(7):1165–9. https://doi.org/10.1016/j.jhsa.2011.03.017
[25] Pegoli L, Pozzi A. Arthroscopic management of scaphoid-trapezium-trapezoid joint arthritis. Hand Clin. 2017;33(4):813–7. https://doi.org/10.1016/j.hcl.2017.07.017
[26] Bellemere P. Pyrocarbon implants for the hand and wrist. Hand Surg Rehabil. 2018;37(3):129–54. https://doi.org/10.1016/j.hansur.2018.03.001
[27] Bellemere P. Pyrocarbon implants for the basal thumb arthritis. Hand Surg Rehabil. 2021;40S:90–101. https://doi.org/10.1016/j.hansur.2020.08.012
[28] Schindele SF, Giddins G, Bellemère P, editors. Arthroplasty in hand surgery : FESSH instructional course book 2020. Stuttgart: Thieme; 2021.
[29] Bellemere P. Medium- and long-term outcomes for hand and wrist pyrocarbon implants. J Hand Surg Eur Vol. 2019;44(9):887–97. https://doi.org/10.1177/1753193419871671
[30] Wong SH, Chiu KY, Yan CH. Review article: osteophytes. J Orthop Surg (Hong Kong). 2016;24(3):403–10. https://doi.org/10.1177/1602400327
