ORIGINAL RESEARCH ARTICLE
The effect of injury area on the success of treatment in digital nerve injury
Numan Atilgan
Department of Hand surgery, Private Clinic, Gaziantep, Turkey
ABSTRACT
Introduction: The main objective of the current study is to investigate variations in postoperative outcomes that follow digital nerve repair in Zone 1 and Zone 2, respectively. We hope that by carrying out this investigation, we will be able to identify which zone has better sensation recovery and patient-reported outcomes, allowing us to identify the best way of conducting surgery for specific types of injuries.
Materials and methods: A retrospective cohort study was conducted in patients with digital nerve injuries treated in a designated hand surgery clinic between January 2021 and December 2023. The study was guided by ethical consideration, where all participants gave their informed consent. Surgical interventions involved primary repair, autograft/allograft nerve grafting, nonsurgical approaches, as well as conduit repair in which results were determined using objective measures and patient feedback.
Results: Direct repair emerged superior among injuries of Zone 1 and Zone 2 with high success rates and good patient-reported outcomes. In general, injuries in Zone 1 had better sensory recovery than injuries in Zone 2 and this was associated with higher levels of satisfaction. Comparisons using statistical methods confirmed that direct repair outperformed other modalities.
Conclusion: More importantly, the comparison of this study shows that repairs in Zone 1 are more successful than those in Zone 2 revealing direct repair as a superior method for digital nerve injuries. The difference is crucial because it suggests that surgical efficiency may depend on where the injury is. This means that direct repair should be given priority over the two zones, although surgeons will need to watch out for challenges related to Zone 2 injuries and adjust their strategies accordingly to obtain the best patient outcomes possible.
KEYWORDS: Digital nerve injuries; surgical repair techniques; Zone 1 and Zone 2 injuries; direct repair
Citation: Journal of Plastic Surgery and Hand Surgery 2024; 59: 89–94. DOI: https://doi.org/10.2340/jphs.v59.40519.
Copyright: © 2024 The Author(s). Published by MJS Publishing on behalf of Acta Chirurgica Scandinavica. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material, with the condition of proper attribution to the original work.
Received: 6 February 2024; Accepted: 25 June 2024; Published: 26 July 2024
CONTACT Numan Atilgan doktor_dao@hotmail.com Department of Hand surgery, Private Clinic, Gaziantep, Turkey, Postal code: 27060.
Competing interests and funding: The author declared no conflicts of interest with respect to the authorship and/or publication of this article.
The author received no financial support for the research and/or authorship of this article.
Introduction
The number of times that digital nerves are injured in a sample urban area in Europe is 6.2 cases per 100,000 people [1]. Various household and occupational accidents cause these injuries, which affect all age groups. However, it mostly affects employees between the ages of 20 and 40 years, with men two to five times more susceptible than women [2, 3]. Standard treatment for digital nerve injuries may involve direct surgical reconnection using the smallest stitches. However, alternative surgical techniques are used when there is a gap that prevents direct reconnection [4, 5].
Having an intricate structure, in addition to being vital to daily living, makes effective therapeutic strategies for hand injuries extremely necessary. Within this category, however, damage to digital nerves poses a unique problem due to their profound impact on tactile sensation and overall hand function. Additionally, variability in the location of digital nerve injury also complicates matters further with primary injury divisions limited to Zone 1 or Zone 2 injuries. This distinction is important because the zone where the injury occurred can be influential both with respect to the operative method and the prognosis for recovery of neural tissue through regeneration processes [6].
Loss of sensory input due to digital nerve injuries causes impaired hand movement, which has an impact on quality of life. This is so because the repair of these injuries began decades ago and this has seen the use of direct repair, autografts, allografts, and conduits. On what it carries along with itself have its own advantages and limitations that are frequently defined by the magnitude and site [7, 8]. However, despite advances in surgical techniques, there is a literature gap on a comprehensive understanding of the relative effectiveness of these methods based on the injury zone. Consequently, digital nerve injuries of Zone 1 versus Zone 2 require a comparative analysis of how the incision area affects cure or no cure success [9].
However, research on the recovery of tactile sensations is not merely physical correction but rather restores people’s full interaction capabilities with their surroundings [10]. Previous research has provided useful information on digital nerve repair outcomes; however, few studies conducted comprehensive analyses that compared success rates between different zones of injury [11]. Additionally, despite being crucial for successful surgical interventions from a holistic perspective, they are often under-reported in terms of patient-reported outcomes, such as satisfaction and perceived quality of life after repair [12].
To narrow the gap in understanding, this study compares the efficacy of various surgical repair techniques for digital nerve injuries in Zone 1 and Zone 2. The focus is on sensory recovery regularity and subjective outcomes, providing a comprehensive view of treatment effectiveness at different injury sites. This analysis is crucial for clinical decision-making and improving patient care strategies for digital nerve injuries.
Our study outlines demographic characteristics, clinical profiles, operative techniques, and evaluates results using both objective measures and patient-reported data. This holistic assessment provides valuable insights into digital nerve repairs.
Digital nerve injuries are complex and require a nuanced understanding of treatments and outcomes. By comparing Zone 1 and Zone 2 injuries, the study aims to identify the reasons for different surgical outcomes and suggest optimal treatment strategies. The ultimate goal is to improve functional outcomes and quality of life for patients through enhanced standards of care.
Materials and methods
Patients
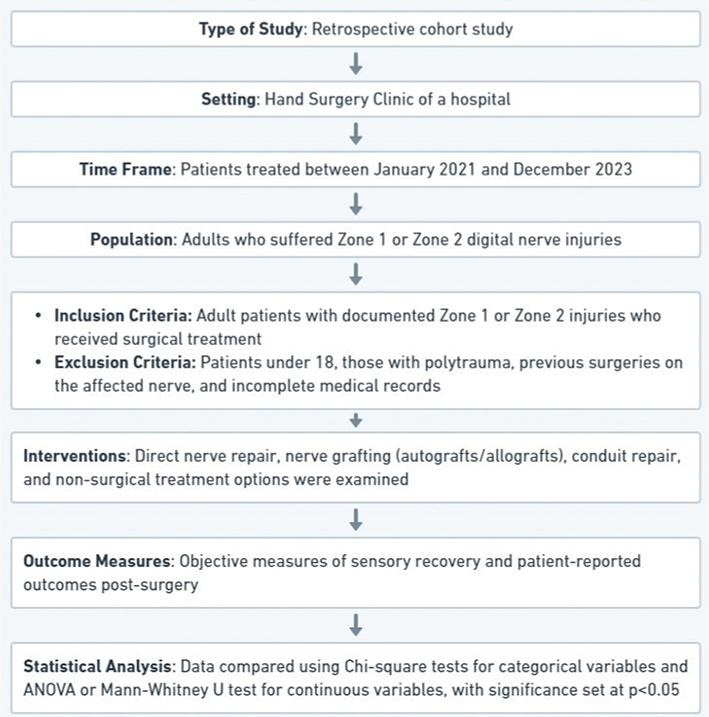
This research used a retrospective cohort study design, with the main focus on patients who underwent treatment for injuries to their digital nerves in the hand surgery clinic of Harran University Hospital between January 2021 and December 2023. The research was aimed at creating a comprehensive data set that involved preoperative, intraoperative, and postoperative determinants. This study was conducted to evaluate and compare the effectiveness of different surgical repair approaches in the treatment of digital nerve injuries (Figure 1.).
The patients who had exhibited digital nerve injury in Zone 1 or Zone 2 and undergone surgical repair made up the population under investigation. Demographic data provided complete range data comprising age, sex, dominant hand, career, and specific type of trauma leading to injury (e.g. cut versus crush). By doing so, it became possible to draw some kind of profile for those demographical characteristics, which will be useful for a better understanding of the characteristics of the population that could influence outcomes after surgery.
Therefore, inclusion criteria were strictly limited to adults over 18 years of age who had clear documentation about digital nerve injury in Zone 1 or Zone 2 and who had received an operative modality out of those investigated. Exclusion criteria defined groups such as those less than 18 years old; polytrauma or accompanying lesions that cause problems with postoperative evaluation; previous operations on damaged nerves; incomplete patient’s medical records. The purpose behind these criteria was to construct an identical group suitable for precise analysis.
Interventions included direct nerve repair, nerve autografts or allografts, conduit repairs, and no surgical repair. The selection of surgical technique was based on the nature of the injury, the considerations of the patient, and the preference of the surgeon. All of these were well documented to facilitate further analysis. Direct nerve repair technique, involving, conventionally, 8–10 sutures of 10–0 single-strand nylon was used in repairing the nerves. Nylon monofilament threads were the most employed suture material. A 10–0 diameter was implemented to precisely approximate the nerve endings. The nerve repair was performed under a surgical microscope to maximise the chances for regeneration by minimising tension during the approximation of both ends. Each suture was placed with utmost precision to ensure direct contact between the nerve ends.
Among other things, Semmes-Weinstein monofilament (SWMF) tests, Moving Two-Point Discrimination (m2PD), and Static two-point discrimination (s2PD) were some of the objective outcome measures chosen with great care. These tests made it possible to make a quantitative assessment of the sensory recovery that occurred after surgery. Structured questionnaires were used to collect patient-reported results. Some topics covered in these questionnaires related to pain management efficiency, life quality after injury and surgery, satisfaction with how the operation went, and perception of improvement in overall performance.
Statistical analysis
Using statistical software, the data was analysed. According to this, continuous variables were presented in the form of means and standard deviations, while those categorical were indicated in frequencies and proportions. Depending on how the data are distributed, we performed a comparative analysis between surgical techniques using the chi-square test for categorical variables and ANOVA or Mann-Whitney U test for continuous ones. For a statistical significance level of 0.05, we accepted p-values below it.
Ethics
The protocol for this study has been approved by the Ethics Committee of the Faculty of Medicine, Harran University, before starting the research. This endorsement indicated that this investigation adhered to ethical principles outlined in the Declaration of Helsinki (1964) and its later amendments. Informed consent was obtained from each participant or their parents/legal guardians to ensure that the medical records were used only after they had agreed in writing about it. Throughout the course of research, confidentiality of patient information was highly maintained and data coding was used to deidentify individual patients.
Results
The information contained in Table 1 provides a basic understanding of these patient populations by giving demographic and clinical details about them. Most of the injured patients in Zone 1 were men, representing 70% of the group, with an average age of 34.7 years. These injuries were primarily caused by cuts in about 60% of cases, and 40% of the injured were manual workers. Table 1 shows the homogeneity among different groups at risk of digital nerve injury. The Zone 2 injury group was slightly younger, with an average age of 31.9 years, and had a similar gender distribution and injury mechanism as the Zone 1 injury group. However, there were some differences in occupation distribution and the time to treatment.
Direct repair was the most frequently performed surgical technique and had the highest success rates in both Zone 1 (90.4%) and Zone 2 (91.9%) injuries, as shown in Table 2. This method demonstrated high efficiency, with the lowest complication rates, which is consistent with its high success rates. Table 2 shows that direct repair yields better outcomes in terms of success rate, sensory recovery time, and complication rate compared to autograft, allograft, or conduit techniques in digital nerve repair attempts.. Direct repair is superior than all other methods having a markedly high success rate. Figure 2 shows direct repair of a severed digital nerve during surgery.

Figure 2. Intraoperative images: Part A (Upper) showcases the meticulous process of direct nerve repair in Zone 1, while Part B (Below) depicts the equivalent procedure undertaken in Zone 2.
In total, injuries in Zone 1 generally achieved better objective sensory recovery results, such as s2PD and m2PD than those seen in injuries in Zone 2 (Result measures for injuries in Zone 1 & 2 injuries: results presented in Table 3). This discrepancy may be related to anatomical and physiological variations between the zones involved. Quality of life scores were high in both zones, but slightly higher among injuries in Zone 1, implying more favourable surgical results noted here.
According to the results of the statistical analysis provided in Table 4 (surgical repair techniques and results), there were statistically significant differences between direct repair and other techniques (p < 0.001). Autograft, allograft, and conduit were not statistically different from each other (p > 0.05). The purpose of this statistical analysis is to validate the trends observed in surgical outcomes, as well as demonstrate the superiority of direct repair compared to other methods.
Zone 2 had additional support from patient-reported outcome measures (Table 5) that demonstrated clinical and objective findings. A greater number of Zone 1 patients reported a significant improvement in quality of life (81%) and high satisfaction with treatment (88%). The patient descriptions supported the improvements made by surgery but also revealed the need to measure patient-specific aspects for evaluation purposes in terms of healing success rates.
Taking into account all these findings, it is evident that there are substantial differences in demographic characteristics, surgical outcomes, and patient-reported measures of digital nerve injuries in Zone 1 compared to Zone 2. The superiority of direct repair in both zones implies that it would be the preferred surgical technique for digital nerve injuries. This is because it has high success rates as well as positive postoperative measures reported by patients.
Discussion
Following a retrospective study at the Harran University Hospital Hand Surgery Clinic between 2021 and 2023, much has been learnt about which surgical techniques work best for digital nerve injuries in Zone 1 and Zone 2. The main objective of this study was to see which zone repair resulted in better results. Although our findings show that direct repair is overall more effective for both zones, it was not the primary objective of this study to find out which zone uses direct repair. But in line with our hypothesis that where digital nerve injury occurs may have a significant effect on the success of surgery and recovery, patients who receive repairs in Zone 1 are more likely to have good results than those who get repairs in Zone 2.
In our study, it is interesting to note that the complication rates varied significantly between the direct repair technique and other techniques such as autograft, allograft, or conduit, with this variation being more pronounced in Zone 1 compared to Zone 2. Although direct repair remains being the most effective approach, there may be higher inherent complexities with Zone 2 injuries that make it less advantageous [13, 14]. With respect to direct repair still being the most successful strategy, these are the circumstances in which it occurs. These findings underscore the imperative need to modify current methods or perhaps invent new ones to improve therapeutic results [15, 16]. In line with these findings, a critical re-evaluation of surgical approaches toward treating Zone 2 injuries should be done because these results show a pressing need for inventing new strategies.
Our results align with several previous studies that have documented the efficacy of direct repair in digital nerve injuries [17]. On the contrary, according to the existing literature on similar cases, nerve grafting appears to produce similar results like direct repair [18]. However, some components of our findings challenge those of the current body of knowledge. This difference may occur due to variation between participant populations, injury characteristics, or even surgical expertise, which underscores the complex nature of surgical decision-making in digital nerve repair. This distinction demonstrates the significance of considering specific circumstances and factors that may be present while applying a more thoughtful approach to each particular case [19, 20].
There are several limitations related to our study due to its retrospective nature. These limitations include the absence of randomisation and bias from medical records review. Consequently, these constraints could limit generalisability. Although there are some restrictions, our research findings are highly significant for those dealing with digital nerve injuries in terms of surgical management. The fact that direct repair has been shown to be superior lends credence to the fact that it is the method that is preferred in clinical settings. However, various shades of grey have been observed in Zone 2 injuries, leading to an indispensable need for individualised treatment plans based on specific context such as the peculiarities of the patient’s injuries and the uniqueness associated with each case. Therefore, individualised approaches are necessary for surgical interventions to be more effective and patient-centred [21, 22]. This means that therapeutic outcomes will only work as planned if optimised in this way.
Conclusion
In conclusion, more importantly, the comparison of this study shows that repairs in Zone 1 are more successful than those in Zone 2, thus revealing direct repair as a superior method for digital nerve injuries. The difference is crucial because it suggests that surgical efficiency may depend on where the injury is. This means that direct repair should be given priority over the two zones, although surgeons will need to watch out for challenges related to Zone 2 injuries and adjust their strategies accordingly to obtain the best patient outcomes possible. Moving forward, it would be desirable for future studies to be conducted on a prospective basis to avoid the challenges that are common with retrospective analyses and also look at new surgical methods that could improve patient outcomes. Generalising our findings to other settings calls for more research, showing the importance of multicentre trials to confirm our results in different clinical contexts.
Author’s contribution
N.A. contributed to study design, data collection, data analysis, figures and writing.
Patient consent for publication
A written informed consent was obtained from each patient.
Data sharing statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
ORCID
Numan Atilgan  https://orcid.org/0000-0001-7184-978X
https://orcid.org/0000-0001-7184-978X
References
[1] Cheng AS. Use of early tactile stimulation in rehabilitation of digital nerve injuries. Am J Occup Ther. 2000;54:159–165. https://doi.org/10.5014/ajot.54.2.159
[2] Fakin RM, Calcagni M, Klein HJ, et al. Long-term clinical outcome after epineural coaptation of digital nerves. J Hand Surg Eur Vol. 2016;41:148–154. https://doi.org/10.1177/1753193415578986
[3] Thomas PR, Saunders RJ, Means KR. Comparison of digital nerve sensory recovery after repair using loupe or operating microscope magnification. J Hand Surg Eur Vol. 2015;40:608–613. https://doi.org/10.1177/1753193414556006
[4] Dresvyanina EN, Tagandurdyyeva NA, Kodolova-Chukhontseva VV, et al. Structure and properties of composite fibers based on Chitosan and single-walled carbon nanotubes for peripheral nerve regeneration. Polymers (Basel). 2023;15:2860. https://doi.org/10.3390/polym15132860
[5] Geuna S, Gnavi S, Perroteau I, et al. Tissue engineering and peripheral nerve reconstruction: an overview. Int Rev Neurobiol. 2013;108:35–57. https://doi.org/10.1016/B978-0-12-410499-0.00002-2
[6] Thorsen F, Rosberg HE, Steen Carlsson K, et al. Digital nerve injuries: epidemiology, results, costs, and impact on daily life. J Plast Surg Hand Surg. 2012;46:184–190. https://doi.org/10.3109/2000656X.2012.676554
[7] Mermans JF, Franssen BB, Serroyen J, et al. Digital nerve injuries: a review of predictors of sensory recovery after microsurgical digital nerve repair. Hand (N Y). 2012;7:233–241. https://doi.org/10.1007/s11552-012-9433-1
[8] Kim JS, Bonsu NY, Leland HA, et al. A systematic review of prognostic factors for sensory recovery after digital nerve reconstruction. Ann Plast Surg. 2018;80:S311–S316. https://doi.org/10.1097/SAP.0000000000001440
[9] Loos MS, Freeman BG, Lorenzetti A. Zone of injury: a critical review of the literature. Ann Plast Surg. 2010;65:573–577. https://doi.org/10.1097/SAP.0b013e3181d50e3e
[10] Kim T, Lohse KR, Mackinnon SE, et al. Patient outcomes after peripheral nerve injury depend on bimanual dexterity and preserved use of the affected hand. Neurorehabil Neural Repair. 2024;38:134–147. https://doi.org/10.1177/15459683241227222
[11] Pamuk C. Digital nerve injury: to repair or not? Ir J Med Sci. 2023;192:2235–2241. https://doi.org/10.1007/s11845-022-03268-4
[12] Billig JI, Sears ED, Travis BN, et al. Patient-reported outcomes: understanding surgical efficacy and quality from the patient’s perspective. Ann Surg Oncol. 2020;27:56–64. https://doi.org/10.1245/s10434-019-07748-3
[13] Lans J, Eberlin KR, Evans PJ, et al. A systematic review and meta-analysis of nerve gap repair: comparative effectiveness of Allografts, Autografts, and conduits. Plast Reconstr Surg. 2023;151:814e–827e. https://doi.org/10.1097/PRS.0000000000010088
[14] Contreras E, Traserra S, Bolivar S, et al. Decellularized graft for repairing severe peripheral nerve injuries in sheep. Neurosurgery. 2023;93:1296–1304. https://doi.org/10.1227/neu.0000000000002572
[15] Moriya K, Yoshizu T, Tsubokawa N, et al. Outcomes of flexor tendon repairs in Zone 2 subzones with early active mobilization. J Hand Surg Eur Vol. 2017;42:896–902. https://doi.org/10.1177/1753193417715213
[16] Kotwal PP, Ansari MT. Zone 2 flexor tendon injuries: venturing into the no man’s land. Indian J Orthop. 2012;46:608–615. https://doi.org/10.4103/0019-5413.104183
[17] Herman ZJ, Ilyas AM. Sensory outcomes in digital nerve repair techniques: an updated meta-analysis and systematic review. Hand (N Y). 2020;15:157–164. https://doi.org/10.1177/1558944719844346
[18] Domeshek LF, Novak CB, Patterson JMM, et al. Nerve transfers-A paradigm shift in the reconstructive ladder. Plast Reconstr Surg Glob Open. 2019;7:e2290. https://doi.org/10.1097/GOX.0000000000002290
[19] Evertsson L, Carlsson C, Turesson C, et al. Incidence, demographics and rehabilitation after digital nerve injury: a population-based study of 1004 adult patients in Sweden. PLoS One. 2023;18:e0283907. https://doi.org/10.1371/journal.pone.0283907
[20] Wang E, Inaba K, Byerly S, et al. Optimal timing for repair of peripheral nerve injuries. J Trauma Acute Care Surg. 2017;83: 875–881. https://doi.org/10.1097/TA.0000000000001570
[21] Tobler-Ammann BC, Beckmann-Fries V, Calcagni M, et al. Outcomes of primary Flexor Tendon repairs in Zones 2 and 3: a retrospective cohort study. J Hand Surg Glob Online. 2023;5:445–453. https://doi.org/10.1016/j.jhsg.2023.03.016
[22] Ross PT, Bibler Zaidi NL. Limited by our limitations. Perspect Med Educ. 2019;8:261–264. https://doi.org/10.1007/s40037-019-00530-x