ORIGINAL RESEARCH ARTICLE
A reliable and objective method of measuring soft tissue changes in 2D photographs after distraction osteogenesis in individuals with CL/P
Annika Bergendal Sternera, Henry Svenssona,b, Magnus Beckera,b, Farokh Collander Farzaneha,b and Anna-Paulina Wiedela,c,d
aDepartment of Clinical Sciences in Malmö, Lund University, Lund, Sweden; bDepartment of Plastic and Reconstructive Surgery, Skåne University Hospital, Malmö, Sweden; cDepartment of Oral and Maxillofacial Surgery, Skåne University Hospital, Malmö, Sweden; dDepartment of Orthodontics, Malmö University, Malmö, Sweden
ABSTRACT
Pre- and postoperative photos to assess results are widely used in plastic and reconstructive surgery, for instance, in patients with cleft lip and palate (CL/P). Evaluations are often performed by assessment panels by viewing the photos. However, these are prone to be subjective. Measurements of soft tissues in photos could be an alternative method but have not been widely used so far. Some patients with CL/P develop a retrognathic maxilla in adolescence, with ensuing Class III malocclusion. In severe cases, distraction osteogenesis (DO) of the maxilla may be indicated. The effect of DO on the facial soft tissues is sparsely reported, perhaps due to the rare procedure. The primary aim of the present study is to provide a reliable and objective method of measuring soft tissue profiles in two-dimensional digital photos. Furthermore, the study aims at assessing changes in soft tissues following DO.
Fourteen patients who had undergone DO at our unit were recruited. Preoperative and postoperative photos were identified, and long-term follow-up photos were taken. Three raters performed measurements of four angles and two distances. Inter- and intra-rater reliability and soft tissue changes were analyzed statistically.
Inter- and intra-rater reliability was high overall for most variables. Two angles related to facial convexity changed significantly. So did the upper lip height.
Soft tissues can be measured with a high degree of accuracy, but further evaluation of the method is necessary. DO causes a favorable increase in facial convexity, and an increased upper lip height.
KEYWORDS: Cleft lip and palate; distraction osteogenesis; longterm follow-up; photo; soft tissue measurements; soft tissue changes; anterior maxillary distraction; RED; validity
Citation: Journal of Plastic Surgery and Hand Surgery 2025; 60: 7–12. DOI: https://doi.org/10.2340/jphs.v60.40580.
Copyright: © 2025 The Author(s). Published by MJS Publishing on behalf of Acta Chirurgica Scandinavica. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material, with the condition of proper attribution to the original work.
Received: 15 April 2024; Accepted: 25 November 2024; Published: 28 January 2025
CONTACT Anna-Paulina Wiedel Anna-Paulina.Wiedel@med.lu.se Department of Oral and Maxillofacial Surgery, Skane University Hospital, Jan Waldenströmsgata 18, Malmö, 20502 Sweden.
Competing interests and funding: The authors report there are no competing interests to declare.
Introduction
An ensuing retrognathic maxilla is sometimes encountered in patients treated due to cleft lip and palate (CL/P). This results in a negative overjet with altered facial aesthetics. If the maxilla is only slightly retrognath, this can be corrected by a Le Fort I osteotomy with instant fixation [1]. In a few cases of more severe retrognathic maxilla, however, distraction osteogenesis (DO) of the maxilla may be indicated. In DO, a Le Fort I osteotomy is created and then the freely mobile teeth-bearing part of the maxilla is gradually advanced forward in the sagittal plane [2]. Both methods, in combination with orthodontic treatment, may achieve a neutral occlusion. However, whether, and in what way, the soft tissues of the face are altered by the procedure is so far poorly understood. If during adolescence the need for a secondary correction of the nose and lip is foreseen, it is customary to wait with these measures until after the orthognathic surgical correction. The idea is to ensure a stable result regarding soft tissues.
Facial appearance, for instance after DO, may be assessed from conventional photos using panels consisting of professionals, patients, and laymen. For this purpose, particular assessment indices have been developed, for instance, the Asher-McDade index and the CARS (Cleft Aesthetic Rating Scale) index [3, 4]. Apart from being prone to subjectivity, viewing photos may focus mostly on the face rather than on the precise effect of a particular surgical procedure. A feasible, objective and reliable measuring method for such an assessment would be of potential great clinical value. Consequently, the possibility of measuring certain angles and distances on preoperative, postoperative and long-term follow-up routine 2-dimensional (2D) digital photos seemed to be an option. 2D digital photography is simple and cheap technology and used routinely worldwide. Consequently, the method can be used globally in all settings which could be of value.
It would appear that very little is written in our context about 2D digital photography, and 3D photography is a significantly more expensive and complicated technology. The primary aim of the present study was therefore to further investigate whether angles and distances of soft tissues of the face can be measured with safety in digital photos. A secondary aim was to assess changes in facial morphometry following DO.
Materials and methods
Subjects
The responsible senior oral and maxillofacial surgeon at our unit kept short notes on which patients had been treated with DO. When the idea of a long-term follow-up study arose in 2017, 16 patients were identified using those notes and a pilot screening of indicated medical records was performed. Indications for DO were individual and primarily based on a combination of a marked retrognathic maxilla and marked scaring in the palate. Patients were then contacted by letter and informed about the study which required a 1.5–2 h visit to the clinic including taking photos and cephalograms, making dental impressions and speech recordings, as well as answering a questionnaire regarding their own experience of the DO procedure. Fourteen patients gave informed consent to participate, while two declined since they lived far away from the clinic.
After the study cohort was set, the photographic archives at the departments of Maxillofacial Surgery and Plastic and Reconstructive Surgery were scrutinized. Photos were taken straight from the front (en face), and in profile. Preoperative photos had to be taken in the late teens to make sure that the facial skeleton was fully grown. Postoperative photos were taken approximately 1 year after DO. Missing data were noted for one patient whose postoperative photos could not be found. Long-term photos were taken at the clinical follow-up. All photos were taken at a distance between camera and subject of 1.5 meters, and camera settings of 50–110 mm regarding focal length and 8–16 regarding aperture.
Demographic data are shown in Table 1. Review of the medical records showed that a secondary rhinoplasty had been delayed in seven patients (3, 4, 6, 9, 12, 13, 14) and a secondary lipplasty in two patients (5, 8) until after completion of the DO. The cohort has previously been reported in regards to patient reported outcome [5] and speech [6]. Briefly, the patients tolerated DO very well. DO caused deteriorated velopharyngeal function in a few cases in whom secondary velopharyngeal surgery had to be performed.
Handling of photos and measurements
All collected photos were transferred to Sectra PACS (Sectra AB, Linköping, SWEDEN) which is the program used by our Department of Radiology for handling images. In order to calibrate the photos en face, the interpupillary distance was set to 100 arbitrary length units measured from the center of each pupil. One senior orthodontist (A), one medical student (B) and one senior plastic surgeon (C) carried out the measurements independently. However, before starting they calibrated their interpretation of crucial landmarks. Angles measured on the profile photos were N’A’Pg, N’Prn’Pg, the nasolabial angle and the tip of the nose (Figures 1 and 2). Distances were measured on the en face photos and represented the alar width and the height of the upper lip (Figure 3). We chose these six parameters based on the most expected effects of DO on the soft tissues. After a minimum of 4 weeks, the assessors repeated the measurements without looking at their previous results. Results were noted on paper sheets and then transferred to a SPSS database for computation.
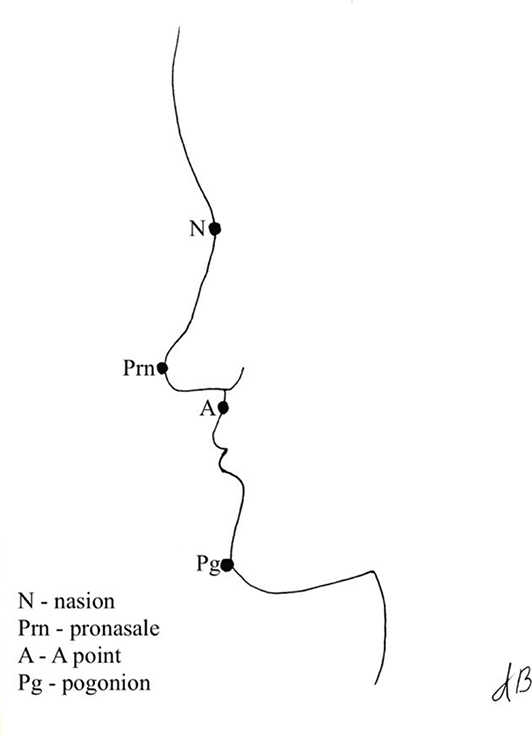
Figure 1. The four landmarks on the profile photos.
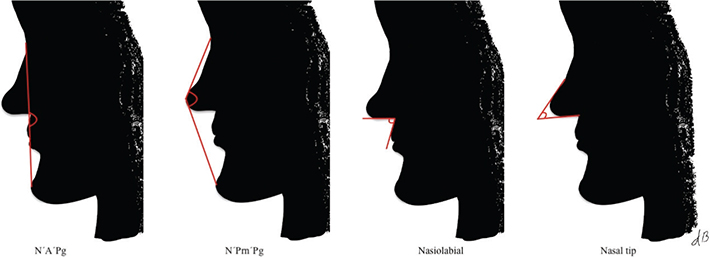
Figure 2. The four measured angles. From left to right: N’A’Pg, N’Prn’Pg, nasolabial, nasal tip.
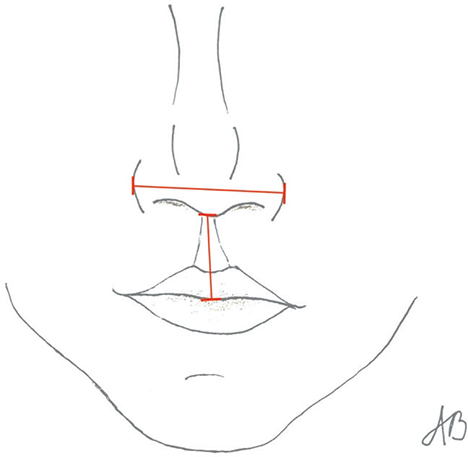
Figure 3. The two measured distances: alar width and upper lip height.
Statistics
Inter-rater agreement
The measurements were stored and analyzed using IBM SPSS Statistics (IBM, New York, U.S.A.). Inter-rater agreement was analyzed using the Intraclass Correlation Coefficient (ICC). For this purpose, the first measurements were used. With a 95% confidence interval (CI), the ICC values indicate the following reliability: <0.5, poor; 0.5–0.75, moderate; 0.75–0.9, good; >0.9, excellent [7].
Intra-rater agreement
Intra-rater agreement, that is, agreement between first measurements and measurements 4 weeks later, was analyzed for each rater, also using the ICC.
Soft tissue changes
The soft tissue measurements were compared between pre- and postoperative photos (n = 13), preoperative photos and follow-up photos (n = 14), and postoperative photos and follow-up photos (n = 13). Whether soft tissues changed following DO was analyzed using the non-parametric Wilcoxon signed rank test for paired observations. For this analysis, median values of the three raters’ first measurements of each angle and distance were used. A p-value <0.05 was considered to indicate a significant change.
Ethics
The study was conducted according to the principles of the Declaration of Helsinki, and it was approved by the Regional Ethical Review Board in Lund, Sweden (Dnr 2017/690). All patients gave their informed consent to participate.
Results
Inter-rater reliability
Table 2 lists the results for inter-rater reliability for each measured variable on the preoperative, postoperative and follow-up photos. The reliability was high overall with average measures ranging from good to excellent. N’A’Pg and N’Prn’Pg had mostly excellent agreement. The nasolabial angle and the nasal tip were the only measurements with moderate agreement between the raters. However, the average measures were still in the good to excellent range. The agreement for linear measurements was good to excellent among the raters.
Intra-rater reliability
Table 3 lists the results for intra-rater reliability for each measured variable on the preoperative, postoperative, and follow-up photos. N’A’Pg and N’Prn’Pg showed excellent agreement for raters A and B, and good to excellent agreement for rater C. The ICC for the preoperative nasolabial angle was low, with poor to moderate agreement. However, raters A and C showed good to excellent agreement for the nasolabial angle on the postoperative and follow-up photos. The nasal tip showed good to excellent agreement for all raters, and the linear measurements showed mostly excellent agreement.
Soft tissue changes
Soft tissue measurements were statistically significant between the preoperative and the postoperative photos, and the preoperative and follow-up photos for N’A’Pg, N’Prn’Pg and upper lip height (Table 4). There were no significant changes between the postoperative, and the follow-up photos for any variable. N’A’Pg decreased from a median of 181.2 on the preoperative photo, to 171.0 on the postoperative photo. This change seemed to remain in the follow-up photos, where the median was 173.3. N’Prn’Pg decreased slightly between the preoperative and the postoperative photos, as well as the follow-up photos. The upper lip height increased from a median of 25.2 in the preoperative photos, to 29.5 and 30.4 in the postoperative and follow-up photos, respectively.
| Variable | Median 0 (min-max) | Median 1 (min-max) | Median 2 (min-max) | p-sig. 0–1 | p-sig. 0–2 | p-sig 1–2 |
| N’A’Pg (degrees) | 181.2 (174.0 – 195.9) | 171.0 (166.7 – 186.6) | 173.3 (167.5 – 189.7) | *** | *** | NS |
| N’Prn’Pg (degrees) | 139.9 (130.0 – 147.4) | 136.3 (130.2 – 148.2) | 138.0 (130.2 – 145.6) | ** | ** | NS |
| Nasolab (degrees) | 106.5 (70.0 – 128.0) | 104.8 (83.5 – 124.2) | 108.5 (82.3 – 131.3) | NS | NS | NS |
| Nasal tip (degrees) | 66.7 (54.1 – 85.2) | 68.3 (46.3 – 87.1) | 65.8 (50.2 – 83.9) | NS | NS | NS |
| Alar width (lu) | 62.4 (54.8 – 68.2) | 66.0 (59.1 – 70.4) | 65.8 (58.6 – 69.9) | NS | NS | NS |
| Upper lip height (lu) | 25.2 (20.0 – 30.2) | 29.5 (26.0 – 33.2) | 30.4 (26.0 – 36.3) | *** | *** | NS |
| Soft tissue medians for the preoperative (0), postoperative (1) and follow-up photos (2) for each variable. The minimum and maximum medians are listed in parentheses. Angular measurements are listed in degrees and distances in length units (lu). Statistically significant differences between 0–1, 0–2, and 1–2, p < 0.001 ***; p < 0.01 **; NS = no significance. | ||||||
Discussion
Methodological considerations
Although CL/P is one of the most common orofacial deformities, the number of patients is small, with an incidence of just 0.1–0.2% of all live births [8, 9]. With modern cleft care, the number of patients who will eventually suffer from severe retrognathic maxilla is even smaller. Therefore, DO for retrognathic maxilla is very seldom encountered in the treatment of CL/P. In this study, we had the opportunity to identify 16 consecutive patients who had undergone the procedure during a 12-year period. Furthermore, 14 of them agreed to participate in a long-term follow-up. Two patients lived far away and were unable to participate for that reason. Hence, the study population should be representative of the entire cohort. A small study population constitutes always a weakness in the study of rare conditions.
Because of the small study population, a literature search was at start conducted to strengthen the scientific basis of the study regarding the feasibility of using digital photos for measurements of angles and distances of soft tissues in the face. The PubMed database was consequently searched (October 2023) using the terms ‘photographic assessment + soft tissue + face’ which generated 189 results. After having judged titles and abstracts, about half of the articles were discarded because they did not fulfill the objectives of the present study. The other half were read in full text except for six which could not be accessed through the internet. Additional inclusion criteria that were the photos depict real persons, and at least three assessors performed measurements independently including methodological evaluations excluded almost all articles. In the end, only two remained. Fink et al. [10] conducted a study where soft tissue measurements were performed on both conventional photos and three-dimensional face scans. The intra-rater reliability varied markedly between moderate and almost perfect. The authors concluded that observer sensitivity affected the outcome of measurements of the facial soft tissues in photographs. Ikävalko et al. [11] used lateral photographs to measure the facial convexity through three different landmarks. The inter-rater reliability varied between poor and moderate, and the authors concluded that their method was unreliable for its purpose.
A cephalogram primarily shows the skeletal structures even though a rough assessment of the soft tissues of the face is conceivable in the lateral view. A cephalogram in the frontal view adds no further information in this respect. Consequently, the use of digital photos with software analysis of angles and distances seems to be an interesting new avenue of refinement when soft tissues need to be addressed. Digital photography is simple and cheap, and it does not imply any radiation hazards. The storage, handling, and visual interpretation of digital images have moreover become a clinical routine worldwide.
At the time when the pre- and postoperative photographs were taken, it was not anticipated that they would constitute a basis for a later scientific evaluation. They were simply taken as a clinical routine and no ruler was used as reference. To overcome this issue, the interpupillary distance was set to 100 in all photos en face and measurements of distances could thereby be expressed in length units, rather than in metric mm. The interpupillary width attains final range at the age around 20 years [12]. Due to this alternative calibration, conclusions can clearly be drawn about the actual changes in alar width and upper lip height in terms of increases and decreases.
Early on it was shown that there is a substantial agreement between findings in clinical investigations and assessments in 2-dimensional digital photographs regarding the soft tissues in patients treated due to CL/P [13]. However, as the literature search showed, reliability analyses of such photographical measurements have been sparsely reported in the past. Nonetheless, reliability analyses are crucial in order to evaluate whether a new method can be implemented in clinical practice with safety. From this perspective, our study population of 14 individuals, 6 variables, and 3 assessors is most adequate for the purpose. Notably, measurements are not dependent on the underlying type of cleft.
The level of agreement varied between the six variables examined in this report but was high overall. N’A’Pg and N’Prn’Pg, which are two large angles between three distinct landmarks, had good to excellent inter- and intra-rater reliability. The nasolabial angle, and to some extent the nasal tip angle, did not reach the same level of agreement. The discrepancy in agreement between the angles could be because it is probably more difficult to measure an angle with less distinct landmarks. Additionally, a small angle makes the raters’ margin of error larger. The same reasoning regarding ambiguous landmarks can be applied to distances, which is supported by a study using 3-dimensional photos in normal adults [14]. However, the inter- and intra-rater reliability were in the good to excellent range for our two distances measured. This was expected since the outer edges of the alae and the lower border of the upper lip were clearly visible on the photos and thereby easy to localize. The subnasale, from which the upper lip height was measured, might be less conspicuous but was also localized with accuracy. The literature search provided two articles for comparison. Both reported poorer levels of agreement compared with our results. This difference might be due to the choice of landmarks, and how difficult these are to locate on photos. In this study, the raters found the four landmarks on the lateral photos easy to localize since they all correspond to the innermost or outermost points of the profile. Fink et al. [10] used the landmarks of the nasion, subnasale, pogonion, orbitale and porion. The orbitale, a landmark under the eye, could possibly be difficult to localize on lateral photos as it lacks well-defined adjacent structures. Furthermore, the subnasale was used by both Fink et al. and Ikävalko et al. [11] and might be slightly harder to locate on lateral photos compared to the A point (Figure 1) which was chosen in this study. Ikävalko et al. used the glabella, the smooth area of the frontal bone between the superciliary arches, instead of the nasion. The glabella is probably harder to localize since it is less distinct than the nasion.
Clinical considerations
DO is expected to markedly improve the facial aesthetics by balancing the facial profile. Both N’A’Pg and N’Prn’Pg really decreased significantly between the preoperative and postoperative photos, indicating a more convex facial profile. The greatest difference was observed in N’A’Pg, by 10.2° whereas N’Prn’Pg decreased only by 3.6°. Because of these small numbers, the differences should be interpreted with caution. Anyhow, the decrease indicates that the soft tissue of the nasal tip is also advanced forward during DO. As mentioned earlier, the nasolabial and nasal tip angles had poorer reliability, and no soft tissue changes between preoperative and postoperative photos were observed in these variables.
The results regarding profile changes after DO are supported by a previous study, in which lateral cephalograms were analyzed in regards to soft tissues. Wen-Ching Ko et al. [15] measured N’Prn’Pg and found a 6.82° decrease. Furthermore, the nasolabial angle favorably increased significantly, but the standard deviation in this variable was large, indicating a great individual variation between patients. This supports our view that the nasolabial angle is ambiguous, and therefore perhaps less appropriate to measure on photographs.
No significant changes were observed in the alar width, which could conceivably increase as a result of increased tension of the soft parts of the base of the nose. Nevertheless, with a fairly low p-value of 0.064 between preoperative and postoperative photos, the width increased by 3.6 length units. A larger study population would perhaps allow for a statistically significant change. The median height of the upper lip increased significantly by 4.3 length units between the preoperative and postoperative photos. This change was perhaps unexpected but shows that the upper lip adjusts after DO and thus covers the upper incisors in a more normal way. We have no sure explanation for this but possibly the vestibular incision plays a role with a release of the lip. However, our results in this respect are not supported by Wen-Ching Ko et al. [15], who found no change in upper lip height.
Meazzini and co-workes [16] investigated 12 adult patients with clefts operated with maxillary DO at a mean age of 24.4 years (range 17–44 years). Results were evaluated with cephalometry and the A point was advanced 17.7 ± 6.6 mm and SNA increased by 13.9 ± 5.9 degrees. No significant change of the maxillary position was observed at long time follow-up indicating that DO is an extremely stable and reliable procedure. Our current results regarding soft tissues are in good agreement with these cephalometric findings as we found no significant changes between postoperative and follow-up photos in any variables. However, no unambiguous conclusion can be drawn from this in the perspective of DO since nine patients had had secondary corrections either of the nose or the lip. These operations might affect the soft parts, although the effects are likely to be less than the effects of the distraction itself. Furthermore, an effect of aging on the soft tissue cannot be excluded as the timeframe between DO and follow-up is wide (21–163 months).
A weakness of the study might be that the photos were taken merely as a clinical routine, rather than in a scientific consistent way. However, our clinical photos follow since long departmental practices: the head leaned to a neck support; the patient was instructed to look straight forward, distance to camera was 1.5 meters; and standard camera settings were used. An inclusion of a ruler in the photos would have enabled measurements of distances in true mm.
Conclusions
Soft tissue measurements of angles and distances in digital photos can be measured with a high degree of accuracy, but further evaluation and standardization of the method is necessary.
DO causes a favorable increase in facial convexity, and an increased upper lip height. These soft tissue changes seem to be stable over time.
Acknowledgement
We are indebted to Bo Sunzel, DDS, associate professor and Ingemar Swanholm, DDS, who in various ways contributed to the initiation and carrying through of the study.
ORCID
Anna-Paulina Wiedel  https://orcid.org/0000-0001-6088-1143
https://orcid.org/0000-0001-6088-1143
References
[1] Phillips JH, Nish I, Daskalogiannakis J. Orthognathic surgery in cleft patients. Plast Reconstr Surg. 2012;129(3):535e–548e. https://doi.org/10.1097/PRS.0b013e31824128e6
[2] Combs PD, Harshbarger RJ, 3rd. Le fort I maxillary advancement using distraction osteogenesis. Semin Plast Surg. 2014;28(4):193–198. https://doi.org/10.1055/s-0034-1390172
[3] Duggal I, Talwar A, Duggal R, et al. Comparative evaluation of nasolabial appearance of unilateral cleft lip and palate patients by professional, patient and layperson using 2 aesthetic scoring systems: a cross sectional study. Orthod Craniofac Res. 2023;26(4):660–666. https://doi.org/10.1111/ocr.12663
[4] Zhu S, Jayaraman J, Khambay B. Evaluation of facial appearance in patients with cleft lip and palate by laypeople and professionals: a systematic literature review. Cleft Palate Craniofac J. 2016;53(2):187–196. https://doi.org/10.1597/14-177
[5] Yasin L, Becker M, Svensson H, et al. Long-term patient-reported outcomes after anterior distraction osteogenesis of the maxilla in patients with cleft. J Plast Surg Hand Surg. 2023;57(1–6):488–493. https://doi.org/10.1080/2000656X.2022.2164294
[6] Klintö K, Svensson H, Wiedel AP. Long-term speech outcome after distraction osteogenesis of the maxilla in patients with cleft lip and palate. J Plast Surg Hand Surg. 2023;58:110–114. https://doi.org/10.2340/jphs.v58.12308
[7] Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155–163. https://doi.org/10.1016/j.jcm.2016.02.012
[8] Salari N, Darvishi N, Heydari M, et al. Global prevalence of cleft palate, cleft lip and cleft plate and lip: a comprehensive systematic review and meta-analysis. Stomatol Oral Maxillofac Surg. 2022;123(2):110–120. https://doi.org/10.1016/j.jormas.2021.05.008
[9] Mossey PA, Little J, Munger RG, et al. Cleft lip and palate. Lancet. 2009;374(9703):1773–1785. https://doi.org/10.1016/S0140-6736(09)60695-4
[10] Fink M, Hirschfelder U, Hirschinger V, et al. Assessment of facial soft-tissue profiles based on lateral photographs versus three-dimensional face scans. J Orofac Orthop. 2017;78(1):70–76. https://doi.org/10.1007/s00056-016-0055-z
[11] Ikävalko T, Narhi M, Lakka T, et al. Lateral facial profile may reveal the risk for sleep disordered breathing in children – the PANIC-study. Acta Odontol Scand. 2015;73(7):550–555. https://doi.org/10.3109/00016357.2014.997795
[12] Filipović T. Changes in the interpupillary distance (IPD) with ages and its effect on the near convergence/distance (NC/D) ratio. Coll Antropol. 2003;27(2):723–727.
[13] Becker M, Svensson H, Jacobsson S. Clinical examination compared with morphometry of digital photographs for evaluation of repaired cleft lips. Scand J Plast Reconstr Hand Surg. 1998;32:301–306. https://doi.org/10.1080/02844319850158642
[14] Duppe K, Becker M, Schönmeyr B. Evaluation of facial anthropometry using three-dimensional photogrammetry and direct measuring techniques. J Craniofac Surg. 2018;29:1245–1251. https://doi.org/10.1097/SCS.0000000000004580
[15] Wen-Ching Ko E, Figueroa AA, Polley JW. Soft tissue profile changes after maxillary advancement with distraction osteogenesis by use of a rigid external distraction device: a 1-year follow-up. J Oral Maxillofac Surg. 2000;58(9):959–970. https://doi.org/10.1053/joms.2000.8735
[16] Meazzini MC, BNasile V, Mazzoleni F, et al. Long-term follow-up of large maxillary advancements with distraction osteogenesis in growing and non-growing cleft lip and palate patients. J Plast Reconstr Aestet Surg. 2015;68(1):79–86. https://doi.org/10.1016/j.bjps.2014.08.069