ORIGINAL RESEARCH ARTICLE
Arthroscopic-assisted total wrist arthrodesis: surgical design and clinical outcomes
Fengchi Suna,b,c,d*, Yuchen Liua,b,c,d*, Shuai Zhua,b,c,d, Xiangmeng Sua,b,c,d, Siwei Xua,b,c,d, Huawei Yina,b,c,d, Wendong Xua,b,c,d and Yundong Shena,b,c,d
aDepartment of Hand Surgery, Huashan Hospital Fudan University Shanghai, China; bDepartment of Hand and Upper Extremity Surgery, Shanghai Jing’an District Central Hospital, Shanghai, China; cNational Clinical Research Center for Aging and Medicine, Huashan Hospital, Fudan University, Shanghai, China; dNHC Key Laboratory of Hand Reconstruction, Fudan University, Shanghai, China
ABSTRACT
Introduction: This study presents an innovative arthroscopy-assisted total wrist arthrodesis technique utilising three hollow screws, aimed at improving clinical outcomes for patients with severe wrist arthritis.
Materials and methods: The technique involved the placement of three hollow screws to facilitate wrist bone fusion. Between August 2019 and August 2023, four patients diagnosed with severe wrist arthritis underwent the arthroscopy-assisted procedure. Each patient was followed postoperatively for at least 1 year. Clinical evaluations included the Visual Analogue Scale (VAS), the Quick Disabilities of the Arm, Shoulder, and Hand (Quick DASH) questionnaire, and the Patient-Rated Wrist Evaluation (PRWE). Radiographic imaging was performed to confirm successful bone fusion. Postoperative complications and scar length were also recorded.
Results: At the final follow-up, all patients exhibited decreased scores on the VAS, Quick DASH, and PRWE assessments, indicating reduced pain and improved wrist function. Radiographic imaging confirmed successful wrist bone fusion. No major complications arose, with an average scar length of 2.8 cm.
Conclusion: The novel arthroscopy-assisted total wrist arthrodesis technique offers a simple and minimally invasive method that effectively improves joint function and alleviates pain in patients with severe wrist arthritis, while reducing the risk of complications.
KEYWORDS: Wrist arthritis; total wrist arthrodesis; wrist fusion; wrist arthroscopy; minimal invasive
Citation: Journal of Plastic Surgery and Hand Surgery 2025; 60: 13–20. DOI: https://doi.org/10.2340/jphs.v60.42751.
Copyright: © 2025 The Author(s). Published by MJS Publishing on behalf of Acta Chirurgica Scandinavica. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material, with the condition of proper attribution to the original work.
Received: 27 September 2024; Accepted: 16 December 2024; Published: 28 January 2025
CONTACT: Yundong Shen yundongshen@fudan.edu.cn Department of Hand Surgery, Huashan Hospital, Fudan University, No.12 Middle Wulumuqi Road, Shanghai 200040, China
*These authors contributed to this work equally, and should be regarded as co-first authors.
Competing interests and funding: The authors report no conflicts of interest.
This work was supported by the National Natural Science Foundation of China under Grant [number 82071406, 82271417].
Introduction
Total wrist arthrodesis is a surgical procedure that fuses the wrist to the radius and is commonly used as an intervention for end-stage wrist arthritis [1,2]. It has been shown to effectively reduce wrist pain and enhance patients’ ability to perform daily activities [3,4]. However, studies have shown that traditional open total wrist arthrodesis, due to its invasive nature, often leads to several postoperative complications, such as tendon adhesions, carpal tunnel syndrome, wound infection, and ulnar impingement [5–8]. Thus, reducing surgical trauma from total wrist arthrodesis remains an urgent clinical challenge.
Wrist arthroscopy is a technique that assists surgeons in diagnosing and treating wrist conditions under direct arthroscopic visualisation [9,10]. Due to its ability to significantly reduce surgical trauma, this minimally invasive approach has become increasingly popular in the treatment of various wrist disorders [11,12]. Recent studies have begun to combine wrist arthroscopy with partial wrist fusion techniques, demonstrating its efficacy in reducing surgical trauma and the incidence of related complications [13,14]. In 2019, Nazerani innovatively integrated arthroscopic technology with total wrist arthrodesis, successfully applying various fixation methods in four patients, achieving favourable outcomes [15]. Despite these advancements, research on combining arthroscopic technology with total wrist arthrodesis remains limited, and there is no standardised fixation method for total wrist arthrodesis. The arthroscopy-assisted total wrist arthrodesis procedure still requires further refinement and standardisation.
The objective of this study is to design a novel arthroscopy-assisted total wrist arthrodesis fixation approach. Postoperative follow-up assessments were conducted to evaluate the surgical outcomes. We hypothesise that the novel wrist arthrodesis technique will significantly alleviate wrist pain, enhance the function of the affected limb, and reduce the incidence of surgery-related complications.
Material and methods
Fusion protocol design
Based on the anatomical characteristics of the distal radiocarpal structure, we developed a novel total wrist arthrodesis technique. This method involves inserting three hollow screws from the radial side of the distal radius into the wrist joint, securing the carpal bones to the distal radius. To ensure an even distribution of the screws across the bone contact surfaces, three lines were drawn on a standard neutral position wrist X-ray (Figure 1).
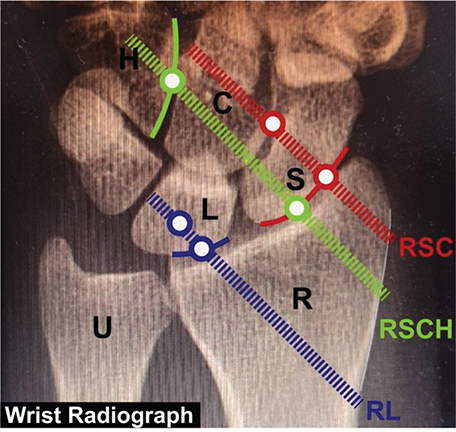
Figure 1. Schematic of the hollow screw insertion path. RSC Line (red dashed line): From the one-third point of the radial-scaphoid joint surface (lower red hollow circle) to the midpoint of the scaphoid-capitate joint surface (upper red hollow circle). RSCH Line (green dashed line): From the two-thirds point of the radial-scaphoid joint surface (lower green hollow circle) to the midpoint of the capitate-hamate joint surface (upper green hollow circle). RL Line (blue dashed line): From the midpoint of the radial-lunate joint surface (lower blue hollow circle) to the midpoint of the lunate (upper blue hollow circle). R: Radius. U: Ulna. S: Scaphoid. L: Lunate. C: Capitate. H: Hamate.
The three lines are: the RSC line (radial-scaphoid-capitate line), from the one-third point of the radial-scaphoid joint surface to the midpoint of the scaphoid-capitate joint surface; the RSCH line (radial-scaphoid-capitate-hamate line), from the two-thirds point of the radial-scaphoid joint surface to the midpoint of the capitate-hamate joint surface; and the RL line (radial-lunate line), from the midpoint of the radial-lunate joint surface to the midpoint of the lunate. The intersection points of these lines with the radial cortical bone were identified as the entry points for the hollow screws. Following these entry points, three hollow screws were inserted along the predetermined paths to complete the total wrist arthrodesis. On lateral X-rays, the three hollow screws should be parallel to the long axis of the radius. In clinical practice, the placement and angles of the screws can be adjusted. For example, the first screw can be inserted into the hamate, or the third screw can be placed in the triquetrum or hamate. Surgeons can flexibly adjust the fixation method based on their expertise and the specific anatomical characteristics of each case.
Surgical technique
Cavity debridement
In the setup for arthroscopic surgery, the patient was positioned supine, with the affected arm placed on a side table following general anaesthesia. The elbow was flexed at 90°, and 10–15 pounds of longitudinal traction were applied. Applying traction with slight wrist flexion helped facilitate approach localisation. Diagnostic wrist arthroscopy portals were then established (3–4, 6R, and 6U) to assess the stability of the triangular fibrocartilage complex (TFCC).
Subsequently, arthroscopic assistance was employed, along with radiofrequency devices and resection tools, to clear proliferative synovial tissues within the wrist joint cavity.
Joint surface grinding
After removing the proliferative synovium, a bone burr was used arthroscopically to grind away the remaining cartilage on the radiocarpal joint surfaces, exposing the subchondral bone. Figure 2 shows arthroscopic images of a wrist arthritis patient before (Figure 2A) and after (Figure 2B) synovium and cartilage debridement.
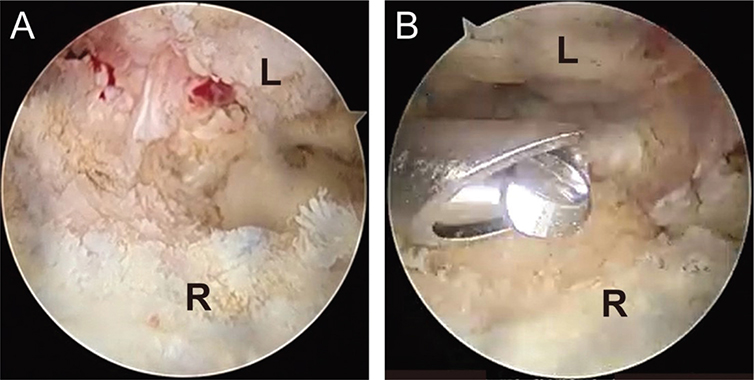
Figure 2. Arthroscopic view from the 6R portal during surgery. (A) Significant synovial proliferation in the joint cavity with destruction of the normal joint structure prior to debridement. (B) Synovial proliferation and degenerated cartilage were removed with a shaver, revealing the subchondral bone surface. R: Radius. L: Lunate.
Notably, all patients in this study exhibited severe wrist damage and osseous fusion in the midcarpal joint, which prevented the insertion of arthroscopic instruments into the midcarpal space. Therefore, no additional procedures were performed in the midcarpal joint aside from the described steps.
Three-screws fixation
A small longitudinal incision was made on the radial side of the distal radius to facilitate the insertion of the hollow screws. The subcutaneous tissue was carefully dissected, taking care to protect the cephalic vein and the superficial radial nerve. The extensor pollicis longus and abductor pollicis longus tendons were retracted to expose the radial cortex. The insertion points and angles for the three hollow screws were determined based on the preoperatively designed entry routes on the posteroanterior wrist X-rays. First, three Kirschner wires (K-wires) were inserted from the distal radius towards the wrist joint to serve as guide wires (Figure 3). Intraoperative fluoroscopy with a C-arm confirmed that the position of the K-wires aligned with the predetermined paths. Next, bone channels were created along the K-wires using a hollow drill bit, and the three hollow screws were inserted, after which the K-wires were removed.
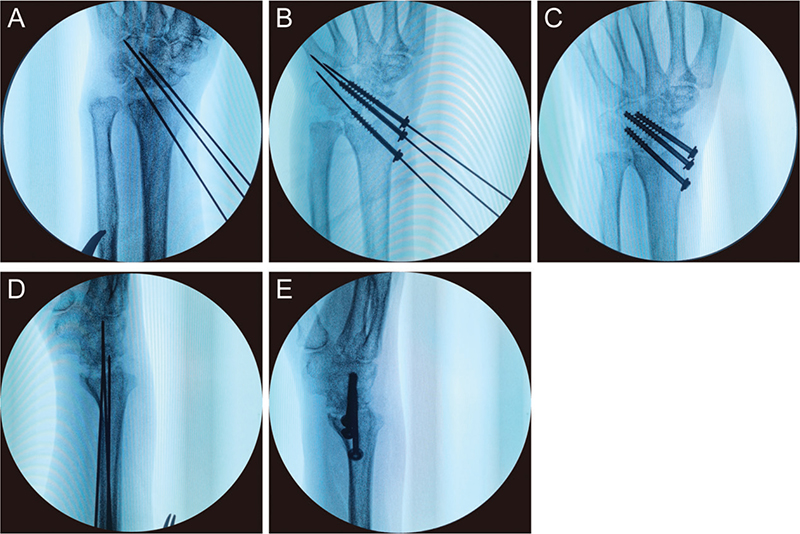
Figure 3. Intraoperative fluoroscopic images. (A) Position of the three Kirschner wires (K-wires) on a posteroanterior wrist X-ray. (B) Hollow drill used along the K-wires to create bone channels, followed by the insertion of three hollow screws. (C) Removal of the K-wires, completing the wrist arthrodesis. (D) Position of the three K-wires on a lateral X-ray. (E) Position of the three hollow screws on a lateral X-ray after completing the wrist arthrodesis.
Once the joint fusion was completed, haemostasis was achieved and the wound was irrigated (Figure 4). The incision was then closed with 5–0 Proline sutures.

Figure 4. Intraoperative photograph illustration. Wound photograph following the placement of three hollow screws.
Rehabilitation
Postoperatively, the wrist was immobilised in a slightly extended position with a short-arm cast. During the first 2 weeks after surgery, the wound was checked every 2–3 days. The cast was typically removed 3–4 weeks after the surgery. Wrist movement was discouraged until the cast was removed. Once bone healing was confirmed and wrist pain had subsided, gradual wrist mobilisation was initiated.
Patients selection
From August 2019 to August 2023, we performed four cases of arthroscopy-assisted debridement combined with wrist arthrodesis surgery at Huashan Hospital Jing’an Branch. Patients were included in this study if they met the following criteria: (1) diagnosed with rheumatoid arthritis or osteoarthritis of the wrist, with significant pain and restricted movement; (2) advanced-stage carpal bone avascular necrosis with joint collapse; (3) failure of conservative treatment, and voluntary consent for surgical intervention; (4) good general health and able to tolerate surgery.
Exclusion criteria included: (1) patients with poor general health or severe underlying diseases; (2) patients with tuberculous or septic wrist infections; (3) patients with poor compliance or those unable to follow postoperative rehabilitation protocols under medical supervision.
In this study, surgical treatment was performed based on the patients’ ages, occupations and activity requirements, with full preoperative communication regarding the pros and cons of other surgical options, such as wrist denervation. The study was approved by the Ethics Committee of Huashan Hospital Jing’an Branch (No. 202475) and conducted in accordance with the principles of the Helsinki Declaration (as revised in 2013). Informed consent was obtained from all participants.
Evaluation of surgical outcome
The evaluations in this study were conducted by a therapist who was unfamiliar with the patients’ medical histories. Preoperatively, and at 1, 4, 8, and 12 and more weeks postoperatively, wrist function was assessed using clinical scales. All patients underwent a postoperative wrist function assessment for at least 1 year. During each assessment, patients completed the Visual Analogue Scale (VAS) to evaluate pre- and postoperative pain levels, and wrist function was assessed using the Quick Disabilities of the Arm, Shoulder and Hand (Quick DASH) questionnaire and the Patient-Rated Wrist Evaluation (PRWE) score. Postoperative active wrist flexion-extension and rotational range of motion (ROM) were recorded and compared with the unaffected side. Routine follow-up included posteroanterior and lateral X-ray examinations of the affected wrist. Postoperative complications and scar length were also recorded.
Data analysis
Data were analysed using Statistical Package for the Social Sciences (SPSS) software (IBM Corporation, Version 25), with p-values <0.05 considered statistically significant. The differences in pre- and postoperative VAS, Quick DASH, and PRWE scores were assessed, and postoperative wrist flexion-extension ROM was compared with the unaffected side. Paired t-tests were used to compare continuous variables.
Results
Patients data
From August 2019 to August 2023, we performed four cases of arthroscopy-assisted debridement combined with wrist arthrodesis surgery at Huashan Hospital Jing’an Branch. The average follow-up period postoperatively was 24.3 months. The demographic characteristics of the patients are summarised in Table 1.
Wrist function
All patients were preoperatively diagnosed with total wrist arthritis, characterised by severe wrist pain that worsened with activity. Due to the severity of wrist pain, patients experienced significant limitations in their daily activities. By the last follow-up, all patients reported significant pain relief, with the average VAS score decreasing from 4.0 to 0.0 (Table 2). Patients reported that the marked reduction in pain enabled them to independently perform most daily activities after surgery. Upper limb function improved significantly following the fusion, with the mean PRWE score decreasing by 60.5 points and the mean Quick DASH score decreasing by 59.1 points. All patients achieved clinically significant improvement [16].
| Var | Patient 1 | Patient 2 | Patient 3 | Patient 4 | Mean | P |
| VAS score | ||||||
| Preoperative | 5 | 4 | 3 | 4 | 4.0 | 0.002* |
| Follow-up | 0 | 0 | 0 | 0 | 0.0 | |
| PRWE score | ||||||
| Preoperative | 75 | 48 | 74 | 65 | 65.5 | <0.001* |
| Follow-up | 8 | 0 | 7 | 5 | 5.0 | |
| Quick DASH score | ||||||
| Preoperative | 84.1 | 59.1 | 68.2 | 81.8 | 73.3 | <0.001* |
| Follow-up | 20.5 | 2.3 | 18.2 | 15.9 | 14.2 | |
| Incision length, cm | 2.4 | 2.8 | 3.0 | 2.8 | 2.8 | |
| VAS: Visual Analog Scale; PRWE: Patient-Rated Wrist Evaluation; Quick DASH: Disabilities of the Arm, Shoulder, and Hand Questionnaire. *Significant difference. Var; variables | ||||||
Range of motion
By the last follow-up, compared to the unaffected side, the flexion and extension ROM of the affected wrist decreased by 55.8° and 49.8°, respectively. Although there was a loss of flexion-extension ROM postoperatively, pronation and supination were well preserved (Table 3, Figure 5A–F).
| ROM | Patient 1 | Patient 2 | Patient 3 | Patient 4 | Mean | P |
| Extension (°) | ||||||
| Uninjured side | 58 | 40 | 65 | 60 | 55.8 | 0.002* |
| Injured side | 0 | 0 | 0 | 0 | 0.0 | |
| Flexion (°) | ||||||
| Uninjured side | 56 | 51 | 42 | 50 | 49.8 | <0.001* |
| Injured side | 0 | 0 | 0 | 0 | 0.0 | |
| Pronation (°) | ||||||
| Uninjured side | 90 | 71 | 81 | 85 | 81.8 | 0.092 |
| Injured side | 90 | 66 | 71 | 80 | 76.8 | |
| Supination (°) | ||||||
| Uninjured side | 90 | 86 | 90 | 85 | 87.8 | 0.098 |
| Injured side | 77 | 85 | 79 | 82 | 80.8 | |
| *Significant difference, ROM; range of motion. | ||||||
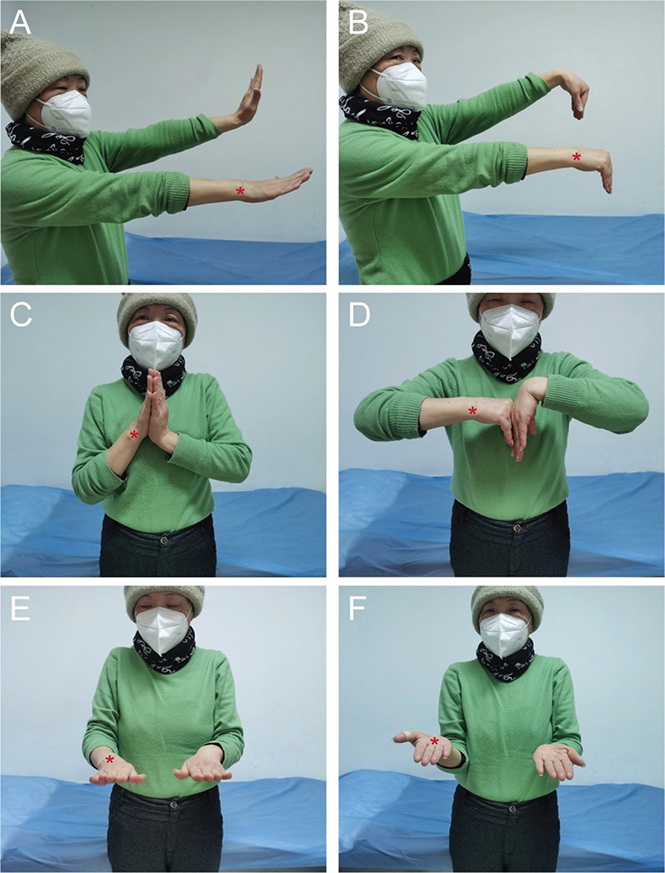
Figure 5. Range of motion (ROM) of the affected and unaffected wrists. (A–B) Active wrist flexion and extension ROM. (C–D) Passive wrist flexion and extension ROM. (E–F) Active pronation and supination ROM. *Surgical side.
Radiographs results
Preoperative magnetic resonance imaging (MRI) and X-ray imaging of the wrist showed that all patients had severe wrist arthritis (Figure 6A–C). Compared to the unaffected side, the joint cartilage was severely eroded, and the joint space was significantly narrowed or completely absent. The diagnosis was conclusively identified as Stage IV Scapholunate Advanced Collapse (SLAC) wrist [17,18]. The final follow-up wrist X-rays for all four patients showed good bone healing, with no complications such as delayed healing or non-union observed (Figure 6D).

Figure 6. Preoperative and postoperative imaging of the same case. (A–B) Preoperative wrist magnetic resonance imaging (MRI). (C) Preoperative X-ray of the affected wrist. (D) Postoperative X-ray of the affected wrist.
Complications and scar
Postoperatively, no patients experienced complications such as tendon adhesions, carpal tunnel syndrome or wound non-healing, effectively avoiding trauma-related complications typically associated with traditional open surgery. After the surgery, only a small longitudinal scar remained on the radial side of the distal radius and small arthroscopic scars on the dorsal wrist. The average length of the radial longitudinal scar was 2.8 cm (Table 2, Figure 7).
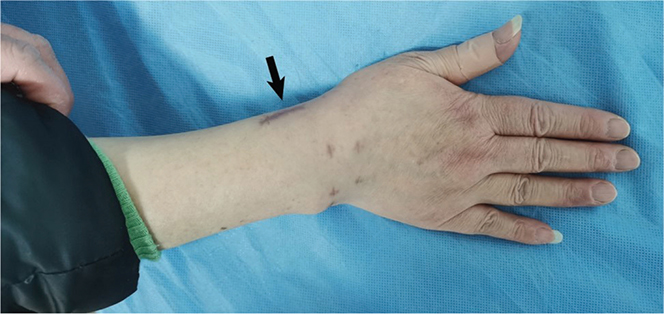
Figure 7. Surgical scar from arthroscopy-assisted wrist arthrodesis.
Discussion
In this study, based on the anatomical characteristics of the distal radius and carpal bones, total wrist arthrodesis was achieved under arthroscopic assistance using three hollow screws. At the final follow-up, all patients who underwent this surgery exhibited significant alleviation of wrist joint pain, with both objective and subjective wrist function scores showing marked improvement. There were no significant postoperative complications observed in the patients.
Our minimally invasive total wrist arthrodesis approach significantly reduced the occurrence of postoperative complications. Traditional open total wrist arthrodesis requires a long dorsal incision at the fixation sites of the radius, carpal, and metacarpal bones [19,20]. This conventional large open incision leads to noticeable scar formation and a higher risk of infection [20,21]. Additionally, open incisions made near the extensor tendons of the fingers can result in postoperative issues such as tendon adhesions [8]. Studies have shown that the overall complication rate following traditional joint fusion surgery is 29% [7]. The minimally invasive approach in this study did not result in related complications, though this may be influenced by the limited clinical cases. Theoretically, however, the improved surgical technique offers significant advantages in reducing the incidence of trauma-related postoperative complications, as demonstrated in the following aspects. Firstly, a smaller incision is made on the radial side of the distal forearm radius. This minimally invasive incision significantly reduces surgical trauma, thereby lowering the associated risks of scar formation and wound infection. Secondly, our minimally invasive incision avoids irritation to the extensor tendons of the fingers, thus preventing tendon adhesions that could affect finger mobility. Thirdly, we use hollow screws for fixation instead of plate fixation, which to some extent reduces the likelihood of secondary surgery to remove internal fixation devices.
In this study, we found that patients who underwent total wrist arthrodesis exhibited a significant reduction in flexion and extension ROM compared to a normal wrist, but pronation and supination movements were well preserved. This outcome is consistent with the follow-up results of wrist motion post-total wrist arthrodesis in many studies on wrist arthritis, likely due to the destruction of the normal anatomical structure of the wrist when the carpal joints are fixed to the radius in total wrist arthrodesis [8]. Although wrist flexion and extension are noticeably restricted after total wrist arthrodesis, research indicates that the wrist requires only a limited ROM to perform most daily activities, which can be compensated for by movements in other joints [22]. Therefore, despite the loss of some ROM post-surgery, the majority of patients remain satisfied with the outcomes of the total wrist arthrodesis, with 93% of patients expressing willingness to undergo the surgery again [23].
The modified fusion surgery may be more suitable for elderly patients with severe wrist arthritis. In addition to total wrist arthrodesis, total wrist arthroplasty is another common method for treating patients with end-stage wrist arthritis [7,8]. Many studies have shown that both methods significantly reduce wrist pain [8,24–26]. Hence, patient needs play a crucial role in the selection of the surgical approach. We propose that the modified total wrist arthrodesis procedure is more appropriate for elderly patients for the following reasons. Firstly, elderly patients with wrist arthritis typically seek pain relief and the ability to perform simple daily activities; preserving wrist mobility is not the primary objective of surgery [27,28]. Therefore, despite postoperative limitation in joint movement, total wrist arthrodesis remains suitable for the elderly. Secondly, cost-effectiveness is a significant consideration when choosing a surgical approach. A cost-effectiveness analysis has shown that the expense of joint arthroplasty is twice that of arthrodesis [25]. The high cost and limited lifespan of prosthetics in total wrist arthroplasty may restrict elderly patients from choosing this option. Thirdly, elderly patients often have underlying physical conditions, including cardiovascular diseases, necessitating a limitation in surgical trauma [29,30]. Our surgical method significantly reduces trauma, thereby minimising the adverse effects of postoperative complications on elderly patients. Therefore, we believe the modified total wrist arthrodesis fixation approach offers elderly patients a surgical option that meets their needs and is cost-effective.
Joint arthrodesis can be used to treat patients with brachial plexus injuries or post-stroke hemiplegia [31–33]. Patients with these conditions often experience significant upper limb motor function limitations due to peripheral or central nervous system damage. The stability of the wrist joint following total wrist arthrodesis aids in further improving finger motor function in these patients [34]. However, it is important to note that tendon adhesions resulting from traditional open fusion surgery can impact finger flexion and extension. Our proposed method addresses this issue by making a small incision on the radial side of the distal radius. Nazarani successfully applied a similar technique to patients with brachial plexus injuries and cerebral palsy, partially restoring their finger flexion, extension movements, and grip strength [15]. We believe that the new surgical approach also holds promise for further application in such patients.
In the process of developing an internal fixation scheme, we ultimately selected a surgical approach using three parallel hollow screws for fixation. This choice was inspired by the fixation method for femoral neck fractures. In the treatment of femoral neck fractures, the use of three parallel hollow screws is a widely applied technique in clinical practice [35]. The fundamental principle of this method is that the screws are arranged in a parallel, inverted triangular formation to achieve a sliding compression effect [36–38]. We adapted this technique for carpal bone fixation, aiming to enhance joint stability. Notably, our three hollow screws did not adopt a parallel, inverted triangular arrangement but were instead placed in a slanting parallel formation from proximal to distal. This choice was driven by two reasons. Firstly, inserting the three hollow screws through the same incision in parallel minimises the number of surgical incisions and reduces surgical trauma. Secondly, postoperative follow-up results indicate that this fixation approach is sufficient to achieve effective wrist joint stabilisation.
Additionally, in traditional open surgery, the use of manual instruments such as bone nibblers to remove degenerated cartilage can lead to excessive bone removal, often necessitating autologous bone grafting [15]. In our surgical technique, arthroscopic assistance allows for more precise joint surface grinding, preserving the contour of the carpal bones’ Gilula arcs more completely, thereby eliminating the need for autologous bone grafting.
Finally, the specific choice of surgical approach must be determined by the surgeon based on the patient’s actual anatomical situation, and the fixation approach proposed in our study is not the only optimal choice. In clinical practice, the insertion positions and angles of the hollow screws can be adjusted. For instance, the first screw can be inserted into the hamate, or the third screw can be placed in the triquetrum or hamate. Surgeons can flexibly adjust the fixation method based on their professional judgement and the anatomical characteristics of each case.
This study has some limitations. As it is a report on a novel arthroscopy-assisted total wrist arthrodesis and first preliminary report on its clinical outcomes, the number of clinical cases included is limited. Future research should expand the patient cohort and include traditional open wrist fusion surgery as a control group to assess the advantages of this minimally invasive surgery in reducing patient recovery time.
Conclusion
The novel arthroscopy-assisted total wrist arthrodesis technique offers a simple and minimally invasive method that effectively improves joint function and alleviates pain in patients with severe wrist arthritis, while reducing the risk of complications.
Acknowledgements
Fengchi Sun and Yuchen Liu contributed equally to the article.
References
[1] Gupta A, Scheker L. Wrist and distal radioulnar joint arthroplasty: maximizing results in difficult conditions. Hand Clin. 2023;39(3):331–339. https://doi.org/10.1016/j.hcl.2023.04.002
[2] O’Callaghan PK, Matthews JH, Kirn PT, et al. Bone grafting in total wrist arthrodesis with large bone defects using the reamer-irrigator-aspirator: A case study of 2 patients. J Hand Surg. 2019;44(7):620.e1–620.e7. https://doi.org/10.1016/j.jhsa.2018.08.021
[3] Hayden RJ, Jebson PJL. Wrist arthrodesis. Hand Clin. 2005;21(4):631–640. https://doi.org/10.1016/j.hcl.2005.08.004
[4] Rayan GM. Wrist arthrodesis. J Hand Surg. 1986;11(3):356–364. https://doi.org/10.1016/s0363-5023(86)80142-3
[5] Rehak DC, Kasper P, Baratz ME, et al. A comparison of plate and pin fixation for arthrodesis of the rheumatoid wrist. Orthopedics. 2000;23(1):43–48. https://doi.org/10.3928/0147-7447-20000101-15
[6] Vicar AJ, Burton RI. Surgical management of the rheumatoid wrist – fusion or arthroplasty. J Hand Surg. 1986;11(6):790–797. https://doi.org/10.1016/s0363-5023(86)80224-6
[7] Wei DH, Feldon P. Total wrist arthrodesis: indications and clinical outcomes. J Am Acad Orthop Surg. 2017;25(1):3–11. https://doi.org/10.5435/JAAOS-D-15-00424
[8] Zhu XM, Perera E, Gohal C, et al. A systematic review of outcomes of wrist arthrodesis and wrist arthroplasty in patients with rheumatoid arthritis. J Hand Surg Eur Vol. 2021;46(3):297–303. https://doi.org/10.1177/1753193420953683
[9] Phillips R, Choo S, Fletcher B, et al. Dry wrist arthroscopy: technique and rationale. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 2023;39(8):1779–1780. https://doi.org/10.1016/j.arthro.2023.02.002
[10] Wolf JM, Dukas A, Pensak M. Advances in wrist arthroscopy. J Am Acad Orthop Surg. 2012;20(11):725–734. https://doi.org/10.5435/JAAOS-20-11-725
[11] d’Ailly PN, Schep NWL, Coert JHH. [Arthroscopy of the wrist]. Ned Tijdschr Geneeskd. 2022;166:D6312.
[12] Shulman B, Catalano L. Wrist arthroscopy scope for the best and plan for the worst. Bull Hosp Jt Dis 2013. 2020;78(1):81–87.
[13] Baur EM. Arthroscopic-assisted partial wrist arthrodesis. Hand Clin. 2017;33(4):735–753. https://doi.org/10.1016/j.hcl.2017.07.013
[14] Ho PC. Arthroscopic partial wrist fusion. Tech Hand Up Extrem Surg. 2008;12(4):242–265. https://doi.org/10.1097/BTH.0b013e318190244b
[15] Nazerani S, Nazerani T, Molayem A, et al. A modified surgical technique for minimally invasive arthroscopic total wrist fusion. J Wrist Surg. 2019;8(1):84–88. https://doi.org/10.1055/s-0038-1669918
[16] Park JH, Lim JW, Kwon YW, et al. Functional outcomes are similar after early and late arthroscopic one-tunnel transosseous repair of triangular fibrocartilage complex foveal tears. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 2020;36(7):1845–1852. https://doi.org/10.1016/j.arthro.2020.03.026
[17] Peterson B, Szabo RM. Carpal osteoarthrosis. Hand Clin. 2006;22(4):517–528; abstract vii. https://doi.org/10.1016/j.hcl.2006.07.001
[18] Weiss KE, Rodner CM. Osteoarthritis of the wrist. J Hand Surg. 2007;32(5):725–746. https://doi.org/10.1016/j.jhsa.2007.02.003
[19] Rodriguez-Merchan EC, Tabeayo-Alvarez ED, Shojaie B, et al. Total wrist arthrodesis: an update on indications, technique and outcomes. Arch Bone Jt Surg. 2023;11(3):144–153. https://doi.org/10.22038/ABJS.2022.65875.3154
[20] Taii T, Matsumoto T, Tanaka S, et al. Wrist arthrodesis in rheumatoid arthritis using an LCP metaphyseal locking plate versus an AO wrist fusion plate. Int J Rheumatol. 2018;2018:4719634. https://doi.org/10.1155/2018/4719634
[21] Hazewinkel MHJ, Lans J, Lunn KN, et al. Complications and factors associated with reoperation following total wrist fusion. J Wrist Surg. 2020;9(6):498–508. https://doi.org/10.1055/s-0040-1714683
[22] Nelson DL. Functional wrist motion. Hand Clin. 1997;13(1):83–92. https://doi.org/10.1016/S0749-0712(21)00082-2
[23] Wagner ER, Elhassan BT, Kakar S. Long-term functional outcomes after bilateral total wrist arthrodesis. J Hand Surg. 2015;40(2):224–228.e1. https://doi.org/10.1016/j.jhsa.2014.10.032
[24] Berber O, Garagnani L, Gidwani S. Systematic review of total wrist arthroplasty and arthrodesis in wrist arthritis. J Wrist Surg. 2018;7(5):424–440. https://doi.org/10.1055/s-0038-1646956
[25] Cavaliere CM, Chung KC. A cost-utility analysis of nonsurgical management, total wrist arthroplasty, and total wrist arthrodesis in rheumatoid arthritis. J Hand Surg. 2010;35(3):379–391.e2. https://doi.org/10.1016/j.jhsa.2009.12.013
[26] Rodríguez-Nogué L, Martínez-Villén G. Total wrist fusion versus total wrist prosthesis: a comparative study. J Plast Surg Hand Surg. 2023;57(1–6):466–470. https://doi.org/10.1080/2000656X.2022.2153131
[27] Siviero P, Zambon S, Limongi F, et al. How hand osteoarthritis, comorbidity, and pain interact to determine functional limitation in older people: observations from the European project on OSteoArthritis study. Arthritis Rheumatol Hoboken NJ. 2016;68(11):2662–2670. https://doi.org/10.1002/art.39757
[28] der Windt JWV, Akkerman W, Hofstra M, et al. Reduced pain and improved daily activities for individuals with hand osteoarthritis using a silicone wrist hand orthosis. J Hand Ther Off J Am Soc Hand Ther. 2023;36(3):669–677. https://doi.org/10.1016/j.jht.2022.09.003
[29] Desserud KF, Veen T, Søreide K. Emergency general surgery in the geriatric patient. Br J Surg. 2016;103(2):e52–e61. https://doi.org/10.1002/bjs.10044
[30] Søreide K, Desserud KF. Emergency surgery in the elderly: the balance between function, frailty, fatality and futility. Scand J Trauma Resusc Emerg Med. 2015;23:10. https://doi.org/10.1186/s13049-015-0099-x
[31] Brunelli G, Vigasio A, Battiston B, et al. [Arthrodesis of the wrist in cases of hand paralysis (personal technique)]. Ann Chir Main Memb Superieur Organe Off Soc Chir Main Ann Hand Up Limb Surg. 1990;9(1):47–53; discussion 54. https://doi.org/10.1016/S0753-9053(05)80499-5
[32] Le Nen D, Kerfant N, Dellestable A, et al. Wrist fusion in peripheral paralysis. Hand Surg Rehabil. 2022;41S:S98–S104. https://doi.org/10.1016/j.hansur.2021.01.010
[33] Steindler A. Orthopedic operations on the hand. J Am Med Assoc. 1918;71:1288–1291. https://doi.org/10.1001/jama.1918.02600420030009
[34] Bincaz LE, Cherifi H, Alnot JY. [Palliative tendon transfer for reanimation of the wrist and finger extension lag. Report of 14 transfers for radial nerve palsies and ten transfers for brachial plexus lesions]. Chir Main. 2002;21(1):13–22. https://doi.org/10.1016/s1297-3203(01)00081-6
[35] Florschutz AV, Langford JR, Haidukewych GJ, et al. Femoral neck fractures: current management. J Orthop Trauma. 2015;29(3):121–129. https://doi.org/10.1097/BOT.0000000000000291
[36] Burgess RC. Anatomic variations of the midcarpal joint. J Hand Surg. 1990;15(1):129–131. https://doi.org/10.1016/S0363-5023(09)91119-4
[37] Maurer SG, Wright KE, Kummer FJ, et al. Two or three screws for fixation of femoral neck fractures? Am J Orthop Belle Mead NJ. 2003;32(9):438–442.
[38] Zdero R, Keast-Butler O, Schemitsch EH. A biomechanical comparison of two triple-screw methods for femoral neck fracture fixation in a synthetic bone model. J Trauma. 2010;69(6):1537–1544. https://doi.org/10.1097/TA.0b013e3181efb1d1