ORIGINAL RESEARCH ARTICLE
Classification and treatment of congenital central slip hypoplasia
Yuzhou Liua,b,c, Xiuyue Xua,b,c, Le Wangd, Jie Laoa,b,c, Yongqing Zhuange and Yousheng Fanga,b,c
aDepartment of Hand Surgery, Huashan Hospital, Fudan University, Shanghai, China; bKey Laboratory of Hand Reconstruction, Ministry of Health, Shanghai, China; cShanghai Key Laboratory of Peripheral Nerve and Microsurgery, Shanghai, China; dDepartment of Pediatric Surgery, Shanghai Jiao Tong University Medical School Affiliated Ruijin Hospital, Shanghai, China; eHand and Microvascular Surgery Department, Shenzhen People’s Hospital, 2nd Clinical Medical College of Jinan University, 1st Affiliated Hospital of Southern University of Science and Technology, Shenzhen, China
Objectives: The aim of this study is to make a diagnosis and a classification for congenital central slip hypoplasia. The surgical treatment was determined according to the classification.
Methods: A retrospective study of 25 treated digits in 13 patients with congenital central slip hypoplasia was carried out. The central slip was classified into two types. Type I: The distance between the insertion of central slip and the proximal interphalangeal joint was shorter than or equal to 5 mm. Type II: The distance between the insertion of central slip and the proximal interphalangeal joint was longer than 5 mm. Tendon advancement or tendon graft was used for type I or II, respectively.
Results: The preoperative mean extension lag was 91° (range, 80°–100°), and the mean follow-up duration was 18 months (range, 9–24 months). The postoperative mean extension lag was 19° (range, 0°–50°). No matter whether in type I or II, the postoperative ranges of proximal interphalangeal joint extension had significant improvement compared with the preoperative ones. There was no statistical difference of proximal interphalangeal joint extension lag changes before and after surgery between the two types.
Conclusion: Congenital central slip hypoplasia could be classified into two types. Either tendon advancement or tendon graft might be effective, which depended on the classification.
KEYWORDS: Central slip; hypoplasia; tendon advancement; tendon graft Level of Evidence: IV (Therapeutic Study)
Citation: Journal of Plastic Surgery and Hand Surgery 2023; 58: 8–12. DOI: https://doi.org/10.2340/jphs.v58.7262.
Copyright: © 2023 The Author(s). Published by MJS Publishing on behalf of Acta Chirurgica Scandinavica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Received: 16 January 2023; Accepted: 10 March 2023. Published: 2023-05-16.
CONTACT Yousheng Fang fyshand@sina.com Department of Hand Surgery, Shanghai Huashan Hospital, 12 Wulumuqi Zhong Road, Jing An District, Shanghai 200040, China. Tel.: 13817937417.
Competing interests and funding: The authors declare that they have no conflicts of interest. The authors have no proprietary, financial, professional, or other personal interests of any nature or kind in any product, service, or company that could be construed as influencing the position presented in, or the review of, the manuscript.
Introduction
There were many kinds of congenital proximal interphalangeal joint flexion deformities, including camptodactyly, proximal flexor contracture, trigger finger, arthrogryposis, and proximal extensor tendon dysplasia and hypoplasia of the central slip. Congenital hypoplasia of the central slip of the extensor tendon was an extremely rare condition [1]. More commonly addressed had been congenital absence of the central slip of the extensor tendons, in which the insertion of the central slip at the base of the middle phalanx was not present [2]. It had been introduced briefly in very few published reports on congenital hypoplasia of the central slip in the English literature [1–4], and the number of cases was very small. At present, there was no report on classification and corresponding treatment plans for congenital hypoplasia of the central slip. In this study, the diagnosis and classification of congenital central slip hypoplasia were clarified. Different surgical schemes were adopted according to the classification.
Methods
A retrospective study of 25 treated digits in 13 patients with congenital hypoplasia of the central slip was carried out.
The diagnosis of congenital hypoplasia of the central slip included the following:
- No active extension of proximal interphalangeal joint of the affected digit since birth, while there was a full range of passive extension of proximal interphalangeal joint (Figure 1).
- The active extension of metacarpophalangeal joint was normal.
- Finger flexors, as well as wrist extensors and flexors, were intact.
- The dorsal skin of proximal interphalangeal joint was sunken and had adhesion with periosteum, while the palmar skin of the digit was normal.
The inclusion criteria were as follows: the patients with the typical signs of the central slip hypoplasia described above since birth and there was no any improvement after rehabilitation treatment for at least half a year. The exclusion criteria included acquired proximal interphalangeal joint extension disorder, camptodactyly, proximal flexor contracture, trigger finger, arthrogryposis, and proximal extensor tendon dysplasia. According to the medical records and inclusion and exclusion criteria, the enrolled patients were confirmed. Our institutional review board approved the study protocol. A written-informed consent was obtained from the guardians of all patients. All methods were carried out in accordance with relevant guidelines and regulations.
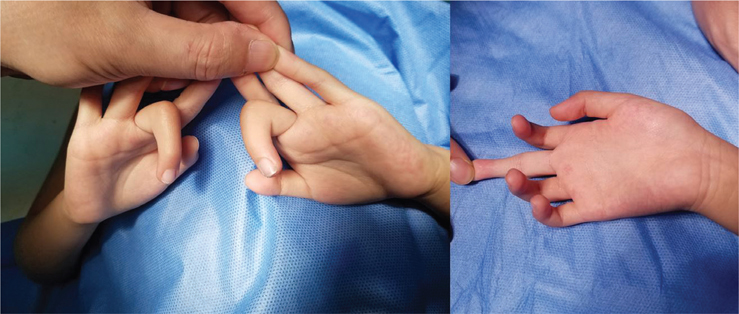
Figure 1. The typical sign of central slip hypoplasia: (left) no active extension of proximal interphalangeal joint, while there was a full range of passive extension of proximal interphalangeal joint (right).
From 2012 to 2020, 13 patients who were affected by hypoplasia of the central slip were treated. Twenty-five affected digits were classified into two types according to the condition of central slip during operation. No other abnormalities of the musculoskeletal system were observed. Radiographs revealed no evidence of bony or joint disease.
Surgical technique
The dorsum of the digit was explored through an ‘S’ incision. The central slip was exposed, and the insertion was detected. The central slip was universally found thinner and less white than the normal tendon. According to the distance between the insertion of the central slip and the proximal interphalangeal joint, the central slip was classified into two types:
Type I: The distance between the insertion of central slip and the proximal interphalangeal joint was shorter than or equal to 5 mm (Figure 2).

Figure 2. Type I: the distance between the insertion of central slip and the proximal phalangeal was shorter than or equal to 5 mm.
Type II: The distance between the insertion of central slip and the proximal interphalangeal joint was longer than 5 mm (Figure 3).

Figure 3. Type II: the distance between the insertion of central slip and the proximal phalangeal was longer than 5 mm.
Tendon advancement
Tendon advancement was suitable for type I. The central slip was dissected from the lateral bands and advanced distally to the insertion (Figure 4). Then, it could be sutured through a transverse osseous tunnel at the proximal end of middle phalangeal with 5-0 PDS (polydioxanone synthetic) sutures.
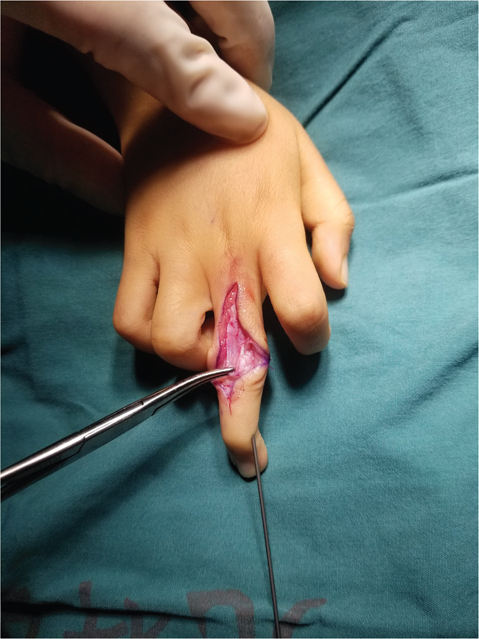
Figure 4. The central slip was dissected from the lateral bands and advanced distally to the insertion.
Tendon graft
As for type II, tendon graft was used to repair the central slip. The attenuated area was uniformly excised. The insertion of central slip was dissected. Palmaris longus tendon was harvested. Then, it was sutured with 5-0 PDS sutures to connect the proximal end of middle phalangeal through a transverse osseous tunnel and the end of central slip as a bridge (Figure 5).

Figure 5. Palmaris longus tendon was sutured with 5-0 PDS sutures to connect the proximal end of middle phalangeal through a transverse osseous tunnel and the end of central slip as a bridge.
No matter whether type I or II, the proximal interphalangeal joint was transfixed with a 1.0 mm Kirschner wire in straight position, and the wound was closed (Figure 6).

Figure 6. The proximal interphalangeal joint was transfixed with a 1.0 mm Kirschner wire in straight position and the wound was closed.
Postoperative care
The Kirschner wire was removed in outpatient 4 weeks after operation. Then, motion exercises were started by a therapist for 2 months.
Evaluation
Clinical outcomes were evaluated with measurement of the residual lack of full active extension of the proximal interphalangeal joint, and complications were recorded at final follow-up.
Statistical analysis
Data analysis was carried out using the Statistical Package for Social Sciences (SPSS version 19.0, Chicago, IL, USA). Comparisons between preoperative and postoperative extension lags and between two types were analyzed using t-test for parametric data and Wilcoxon signed rank sum test for nonparametric data. A p < 0.05 was considered statistically significant.
Ethics
All experimental protocols were approved by the Huashan Hospital’s Institutional Review Board. All methods were carried out in accordance with relevant guidelines and regulations.
Results
Patient demographic data and results were listed in Table 1. Patients included nine boys and four girls, mean age 44.1 months (range 14 months–7 years) at operation. In total, congenital hypoplasia of the central slip was found in 13 index and 12 middle fingers.
In this study, in total, there were 13 patients with 25 affected digits. Of which, 14 digits were repaired with tendon advancement, while another 11 digits were repaired with tendon graft. Six patients had bilateral symmetric hypoplasia of the central slip, while seven patients were affected unilaterally. One patient had two operation methods (tendon advancement and tendon graft) in two digits.
The preoperative mean extension lag was 91° (range, 80°–100°), and the mean follow-up duration was 18 months (range, 9–24 months). At the last follow-up, all the patients had improved active extension of proximal interphalangeal joint. The postoperative mean extension lag was 19° (range, 0°–50°), which was statistically less than the preoperative mean extension lag. The parents were satisfied with the improvement in range of extension of proximal interphalangeal joint. Neither operation methods had effect on flexion postoperatively in each patient.
The mean postoperative extension lags in tendon advancement and tendon graft groups were 17° and 20°, respectively. No matter whether in type I or II, the postoperative ranges of extension of proximal interphalangeal joint had significant improvement compared with the preoperative ones (p < 0.05). There was no statistical difference between the two types in the changes of extension lag of proximal interphalangeal joint before and after surgery (p = 0.819).
Complications
Thirteen digits in seven patients suffered joint stiffness within 4 weeks. After 2 months, the flexion and the extension of proximal interphalangeal joint improved. There were no other complications in all the patients.
Discussion
Congenital flexion deformity of the proximal interphalangeal finger joint was an occasional observation in children [1], which could be caused by various reasons. The clinical phenotype of camptodactyly [5] included ineffective active and passive extension of proximal interphalangeal joint, intrinsic and extrinsic tendon shortening, and a skin deficit on the palmar side of the proximal interphalangeal joint [6], which was different from the central slip hypoplasia. Congenital trigger finger [7,8] was another kind of flexor deformity caused by tendon sheath thickening and compression of flexor tendon. The finger extensor tendon was normal. Patients could intermittently do flexion and extension of proximal interphalangeal joint actively and passively. The pathological manifestation of congenital proximal flexor contracture [9,10] was at the beginning of the forearm flexor group. The digit extensor tendon was normal, but active and passive extensions of proximal interphalangeal joint were ineffective. Arthrogryposis [11,12] was a multiple symmetrical disease involving the whole body and flexor deformity occurring in many joints of the body. The difference between proximal extensor tendon dysplasia [13–15] and central slip hypoplasia was active extension of metacarpophalangeal joint. No active extension of metacarpophalangeal joint occurred in proximal extensor tendon dysplasia, while normal active extension of metacarpophalangeal joint could be finished in central slip hypoplasia.
In this study, congenital hypoplasia of the central slip occurred in index and middle fingers. Bilateral symmetrical central tendon dysplasia accounted for nearly a half. No matter tendon advancement or tendon graft, the surgery had improved the extension of proximal interphalangeal joint significantly without influencing the finger flexion function, which indicated that the classification and the surgical treatment according to the classification might be effective. There was no statistical difference between the two types in the changes of extension lag of proximal interphalangeal joint before and after surgery, which meant the essences of these two surgical methods could be consistent. So, congenital central slip hypoplasia could be classified into two types, according to the attenuated central slip. Either tendon advancement or tendon graft might be effective to repair hypoplasia of the central slip, which depended on the classification. The postoperative extension lag in one patient’s digit was 50°. She had tendon graft, which might be loose after removing the K wire and doing exercises. It resulted in limited extension of the digit. There was no severe complication in this study.
Carneiro reported five cases of central slip hypoplasia had tendon advancement [2]. There was usually half a centimeter or less between the normal tendon proximally and distally. Their treatment is consistent with our classified surgery. At the follow-up, there was a 10° and a 15° lack of extension in two small digits, respectively. The other three fingers developed full extension and 90” of flexion within 2 months of the surgery. The result was similar to our study. Lin reported a 19-year-old man with bilateral laxity of the central slip was treated surgically by non-excisional tightening of the central slip [4]. The case was different from others because laxity of the central slip was the cause of the deformity instead of the central slip attenuated and shorten. We had not seen the laxity of the central slip in any patient in the study. N. Hidaka described the outcomes of conservative treatment to 22 fingers with congenital central slip hypoplasia in 16 patients [1]. Treatment with bracing was successful in 21 digits, while unsuccessful in one digit. The mean age of patients was 10 months. As for the young patients within 1 years, conservative treatment could be useful. In our study, the average age of patients was 44.1 months. All patients had tried conservative treatment for at least half a year, but failed. Surgical treatment was a further helpful option for them.
Acute and chronic central slip injuries in adults were common. Direct suture or using a suture anchor was often adopted for an acute central slip laceration in adults. For a central slip defect, there were several surgical methods to repair it, including tendon advancement, using a proximally based flap of central slip tendon to rotate itself distally to reconstruct the central slip (Snow method) [16], or tendon graft. The choice of the repair method depended on several factors, including the length of defect and the width and texture of central slip. For children with central slip hypoplasia, there was a distance from the insertion point of central slip to the proximal interphalangeal joint. Learning from the method of repairing central slip defect in adult, tendon advancement was suitable for a short distance defect in children with central slip hypoplasia. Due to a thin texture tendon in central slip hypoplasia, tendon graft was an appropriate choice for a long-distance defect instead of Snow method in children with central slip hypoplasia. In this study, the age of patients ranged from 14 months to 7 years. The defect distance of 0.5 cm was used as the dividing line between tendon advancement and tendon graft. The curative effects were confirmed in both groups after follow-up. With the increase of age after 7 years, the dividing line might change, which was closely related to the length and ductility of the central slip.
This study had some limitations. This study was a retrospective study, and there was no control group. There was no imaging examination confirming hypoplasia of the central slip before operation. Because the central slip was very thin and small in child, it was difficult for detecting and imaging by normal ultrasound examination. In further research, special ultrasound or magnetic resonance imaging examination might be used to detect the condition of extensor tendon, which could be helpful to clarify the classification and treatment before surgery.
Acknowledgments
This work was funded by the National Natural Science Foundation of China (NSFC 81972122), the Shanghai Municipal Key Clinical Specialty (shslczdzk05601), and the Shenzhen’s Sanming Project (SZSM202111015). This study was supported by the Hand Surgery Department in Huashan Hospital, the Hand Function Research Center in Fudan University, and the Shenzhen People’s Hospital.
References
[1] Hidaka N, Uemura T, Nakamura H. Successful conservative treatment outcomes and clinical characteristics of congenital hypoplasia of the extensor tendon central slip. J Hand Surg Eur Vol. 2017;42(3):295–300. https://doi.org/10.1177/1753193416676410
[2] Carneiro RS. Congenital attenuation of the extensor tendon central slip. J Hand Surg Am. 1993;18:1004–1007. https://doi.org/10.1016/0363-5023(93)90391-F
[3] Kim JP, Go JH, Hwang CH, et al. Restoration of the central slip in congenital form of boutonniere deformity: case report. J Hand Surg Am. 2014;39:1978–1981. https://doi.org/10.1016/j.jhsa.2014.05.030
[4] Lin SC, Chiu HY. A nonexcision plication method for treatment of bilateral congenital boutonnière deformity: a preoperative biomechanical calculation. Plast Reconstr Surg. 2004;113:1742–1745. https://doi.org/10.1097/01.PRS.0000117372.82981.3C
[5] Singh V, Haq A, Priyadarshini P, et al. Camptodactyly: an unsolved area of plastic surgery. Arch Plast Surg. 2018;45(4):363–366. https://doi.org/10.5999/aps.2017.00759
[6] Wall LB, Ezaki M, Goldfarb CA. Camptodactyly treatment for the lesser digits. J Hand Surg Am. 2018;43(9):874.e1–874.e4. https://doi.org/10.1016/j.jhsa.2018.03.023
[7] Ahmad Salati S. Congenital trigger finger. J Neonatal Surg. 2014;3(3):42. https://doi.org/10.47338/jns.v3.255
[8] Cardon LJ, Ezaki M, Carter PR. Trigger finger in children. J Hand Surg Am. 1999;24(6):1156–1161. https://doi.org/10.1053/jhsu.1999.1156
[9] Li H, Guan S. Progressing flexion deformity of the middle, ring, and small fingers with a rare congenital anatomic difference of flexor digitorum profundus. J Pediatr Orthop. 2020;40(7):e603–e608. https://doi.org/10.1097/BPO.0000000000001485
[10] Xiong G, Gao Y, Zhu J, et al. Congenital contracture of the ulnar digits and its differentiation from ischemic contracture. J Hand Surg Am. 2022;47(6):579.e1–579.e9. https://doi.org/10.1016/j.jhsa.2021.06.008
[11] Bamshad M, Van Heest AE, Pleasure D. Arthrogryposis: a review and update. J Bone Joint Surg Am. 2009;91(Suppl. 4):40–46. https://doi.org/10.2106/JBJS.I.00281
[12] Hall JG, Kimber E, Dieterich K. Classification of arthrogryposis. Am J Med Genet C Semin Med Genet. 2019;181(3):300–303. https://doi.org/10.1002/ajmg.c.31716
[13] Tungshusakul S, Leechavengvongs S, Uerpairojkit C. Bilateral congenital hypoplasia of the extensor tendons of the hand: a case report. Hand Surg. 2011;16(1):77–80. https://doi.org/10.1142/S0218810411005102
[14] Vartanian ED, Cohen MJ, Kulber DA. Congenital hypoplasia of the extensor tendons of the fingers: a case report and review of the literature. J Hand Surg Am. 2020;45(2):162.e1–162.e5. https://doi.org/10.1016/j.jhsa.2019.03.018
[15] Vartany A, Majumdar S, Diao E. Congenital hypoplasia of the extensor tendons of the hand. J Hand Surg Am. 1996;21(6):1045–1047. https://doi.org/10.1016/S0363-5023(96)80313-3
[16] Snow JW. A method for reconstruction of the central slip of the extensor tendon of a finger. Plast Reconstr Surg. 1976;57:455–459. https://doi.org/10.1097/00006534-197604000-00007