ORIGINAL RESEARCH ARTICLE
Do men adapt to lower urinary tract symptoms? An 11-year longitudinal study of male urinary urgency and associated bother
Jonne Åkerlaa,b , Jori S. Pesonenc, Essi Peltonend
, Jori S. Pesonenc, Essi Peltonend , Heini Huhtalad
, Heini Huhtalad , Jukka Häkkinene, Juha Koskimäkia
, Jukka Häkkinene, Juha Koskimäkia , Teuvo L.J. Tammelaa,b
, Teuvo L.J. Tammelaa,b , Anssi Auvinend
, Anssi Auvinend and Antti Pöyhönenf
and Antti Pöyhönenf
aDepartment of Urology, Tampere University Hospital, Tampere, Finland; bFaculty of Medicine and Health Technology, Tampere University, Tampere, Finland; cDepartment of Urology, Päijät-Häme Central Hospital, Lahti, Finland; dFaculty of Social Sciences, Tampere University, Tampere, Finland; eDepartment of Urology, Länsi-Pohja Healthcare District, Kemi, Finland; fCentre for Military Medicine, The Finnish Defence Forces, Riihimäki, Finland
ABSTRACT
Objective: The study objective is to evaluate prognosis and predictors of bother caused by urinary urgency among middle-aged and older men.
Material and methods: A population-based sample of men born in 1974, 1964, 1954, 1944, 1934 and 1924 was followed-up from 2004 to 2015. The course of urgency and associated bother was evaluated with the Danish Prostatic Symptom Score at baseline and follow-up. Logistic regression was utilized to explore risk factors of increased bother at follow-up.
Results: A total of 2,480 men (39%) who had responded at baseline and follow-up were included in the study. Of them, 1,056 men (43%) had persistent mild urgency and 132 men (5%) persistent moderate or severe urgency at follow-up. The proportions of men experiencing at least moderate bother due to persistent urgency at follow-up were 6% (95% confidence interval 4.5–7.3) of those with mild and 79% (71.7–85.9) of the men with moderate or severe urgency. In multivariable-adjusted logistic regression, moderate to severe urgency was strongly associated with bother (odds ratio, OR 55.2, 95% CI 32.1–95.2). Other predictors of bother included cardiac disease (OR 1.8, 95% CI 1.0–31.1), pulmonary disease (OR 1.9, 95% CI 1.1–3.5) and medical treatment (OR 2.7, 95% CI 1.6–4.6).
Conclusions: Most men with urinary urgency have mild symptoms and bother. Only one out of five men with persistent moderate or severe urgency adapt to the symptoms. Men with a history of medical treatment for lower urinary tract symptoms (LUTS) or impaired cardiopulmonary health are more likely to experience bother from urinary urgency.
KEYWORDS: Lower urinary tract symptoms; urinary bladder, overactive; cohort studies; observational studies
Citation: Scandinavian Journal of Urology 2024, VOL. 59, 47–53. https://doi.org/10.2340/sju.v59.18289.
Copyright: © 2024 The Author(s). Published by MJS Publishing on behalf of Acta Chirurgica Scandinavica. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material, with the condition of proper attribution to the original work.
Received: 22 July 2023; Accepted: 4 January 2024; Published: 26 February 2024
CONTACT Jonne Åkerla jonne.akerla@gmail.com Department of Urology, Tampere University Hospital, Tampere, Finland, Teiskontie 35, 33521 Tampere, Finland
Supplemental data for this article can be accessed online at https://doi.org/10.2340/sju.v59.18289
Competing interests and funding: The work of Jonne Åkerla was funded by Finnish Urological Association and Orion Research Foundation. Jonne Åkerla has attended scientific congress as a guest for Ipsen. Jori Pesonen has received a lecture honorarium from Astellas, Boston Scientific and Ferring. Teuvo Tammela has worked as a consultant for Astellas, Pfizer and Bayer AG. Essi Syrjälä, Heini Huhtala, Jukka Häkkinen, Juha Koskimäki, Anssi Auvinen and Antti Pöyhönen declare no conflict of interest.
Introduction
The prevalence of various lower urinary tract symptoms (LUTS) increases with age [1]. Progression of male LUTS is often associated with age-related changes in the morphology and function of the lower urinary tract, such as benign prostatic hyperplasia (BPH) [2]. Furthermore, the etiology of LUTS is typically multifactorial and the course of various symptoms is often modified by comorbidities and behavioral factors, such as metabolic syndrome, diabetes [3, 4].
LUTS can result from dysfunction during bladder filling (storage), emptying (voiding) or post-micturition phase, and symptoms often occur in combination [5, 6]. Responses to LUTS treatment vary widely due to a broad spectrum of dysfunction and differences in the perception of bother. In addition, various comorbidities may pose challenges to the tolerability of treatments, especially among frail elderly patients [7, 8]. Furthermore, despite initial treatment response, many symptoms tend to recur [9].
Cross-sectional studies have shown substantial differences in bother from various male LUTS [5, 6, 10]. However, evidence on long-term adaptation and impact of watchful waiting on symptom perception is, to date, very limited [1, 11, 12]. As only bothersome symptoms are considered patient-important, data on long-term coping with various symptoms from longitudinal studies would serve as an important aid for shared decision making about treatments. Therefore, we measured the longitudinal changes in bother caused by one of the most common male LUTS, urinary urgency, in a population-based cohort of middle-aged and older men.
Materials and methods
This report is based on the population-based Tampere Aging Male Urologic Study (TAMUS). Details of the study protocol have been presented previously [13, 14]. The baseline survey for this analysis was conducted in 2004, with the target population consisting of all male residents in Tampere and 11 surrounding rural communities aged 30, 40, 50, 60, 70 and 80 years. For the follow-up, the same men were approached again in 2015. In the initial survey, men eligible for the study were identified from the comprehensive, nationwide Population Register Centre. For the 2015 repeat survey, updated addresses were acquired from the Population Register Centre. Postal questionnaires were used to collect study information comprising items on severity and bother of LUTS, as well as sociodemographic, anthropometric and behavioral factors and medical conditions. The Tampere University Hospital Committee of Research Ethics approved the study protocol (tracking number #99050).
Symptom assessment
The LUTS were assessed using the Danish Prostatic Symptom Score (DAN-PSS-1) – a validated questionnaire consistent with the International Continence Society definitions [15, 16]. The current study included men with responses available to the assessments of urgency in 2004 and 2015 with no further exclusion criteria. The symptom-specific DAN-PSS question translated back from Finnish to English was as follows: ‘Do you experience a sudden need to void?’. The response options were ‘never – rarely – often – always’. Respectively, the classification of bother was based on four response options as follows: ‘not at all – a little – moderately – very much’. In terms of both symptom severity and bother, each symptom was scored as ‘absent (0 points)’, ‘mild (1 point)’, ‘moderate (2 points)’ and ‘severe (3 points)’. The preceding 2-week period was defined as the reference time frame for the questions.
Registry data sources
To explore care seeking trends among men with LUTS, data on alpha blockers, 5-alpha reductase inhibitors, antimuscarinics and mirabegron medications for BPH and LUTS were obtained from the comprehensive nationwide prescription database of the Social Insurance Institution of Finland. Data on surgical procedures for BPH/LUTS according to the Nordic Classification of Surgical Procedures were obtained from the Care Register for Social Welfare and Health Care (HILMO) maintained by the National Institute for Health and Welfare (Table S1).
Statistical analyses
To examine the association between the changes of urgency and bother over time, questionnaire surveys were conducted in 2004 and 2015 for the cohort of men aged 30–80 years at baseline. In data analyses, prevalence of no or mild (0–1 DAN-PSS point) and moderate to severe bother (≥2 DAN-PSS points) was estimated for increased, decreased and persistent urgency at follow-up for the age groups of 30–40, 50–60 and 70–80 years (at baseline). To further assess possible exposure-response relationship, urgency severity and bother were cross-tabulated to illustrate frequencies of symptom progression (an increase of 1 vs. ≥2 DAN-PSS points from baseline to follow-up), symptom resolution (a decrease of 1 vs. ≥2 DAN-PSS points at follow-up), and unchanged symptom status (similar DAN-PSS score at baseline and follow-up).
Multivariable logistic regression was utilized to explore the impact of various potential determinants on adaptation to urgency among men with persistent urgency at follow-up. A subgroup analysis was conducted for men with persistent mild urgency to explore potential predictors of bother independently of symptom severity. Selection of co-variables was based on previous literature on potential risk factors of bothersome male LUTS [3, 4, 17, 18] and factors with potential impact on psychosocial coping and general symptom perception [19, 20]. For comparison, separate analyses were conducted to explore the association of an identical set of covariables with urgency independently of bother. Statistical analyses were performed using Stata 12.1 (StataCorp, College Station, TX, USA).
Results
In 2004, the participation proportion was 59% (4,384 of 7,470 men) and in 2015, 48% (3,063 of 6,358 men). A total of 2,480 men (39%) who had responded to the assessments of urgency both at baseline and follow-up were included in the analysis. Urinary urgency was the most common symptom of the 12 assessed LUTS with prevalence of 66% in 2004 and 73% in 2015 (Figure 1).
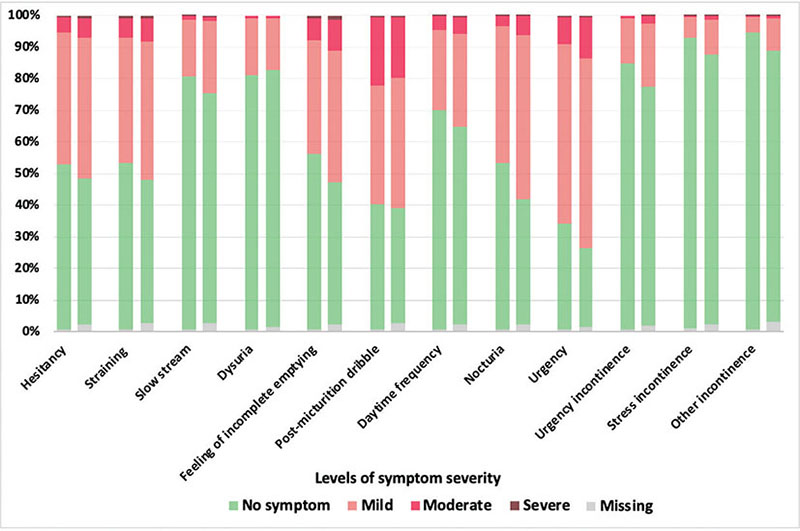
Figure 1. Periodical prevalence of LUTS in 2004 (left) and 2015 (right).
Although the majority of men remained married or cohabiting at 11-year follow-up, the prevalence of single or widowed men increased in the oldest age group: the proportions of single/widowed men were 24%, 24% and 29% in the age groups of 30–40, 50–60 and 70–80 (in 2004) at the follow-up in 2015. Smoking showed a decreasing trend in all age groups while the majority of the assessed comorbidities increased with age with exceptions of obesity and depression. The prevalence of previous medical treatment of BPH/LUTS in 2004 were 1%, 6% and 29% among men aged 30–40 years, 50–60 years and 70–80 years, respectively. In 2015, the respective proportions were 6%, 28% and 52%. In 2004, none of the men aged 30–40 had a previous history of operative treatment for BPH/LUTS, while among men aged 50–60 and 70–80, the proportions were 0.3% and 5%. In 2015, the proportions of men having received operative treatment were 0.1%, 4% and 11% in the three respective age groups (Table 1).
| Age at baseline | ||||||||||||
| 30–40 years (n = 895) | 50–60 years (n = 1,193) | 70–80 years (n = 392) | ||||||||||
| 2004 | 2015 | 2004 | 2015 | 2004 | 2015 | |||||||
| n | % | n | % | n | % | n | % | n | % | n | % | |
| Single or widowed | 276 | 30.9 | 213 | 24.1 | 260 | 21.8 | 284 | 23.8 | 62 | 15.8 | 114 | 29.1 |
| Current smoker | 240 | 26.8 | 177 | 19.8 | 301 | 25.2 | 208 | 17.4 | 28 | 7.1 | 22 | 5.6 |
| BMI ≥30 | 106 | 12.0 | 170 | 19.0 | 232 | 19.6 | 266 | 22.6 | 61 | 15.9 | 49 | 12.8 |
| Diabetes | 13 | 1.5 | 36 | 4.0 | 71 | 6.0 | 201 | 16.9 | 50 | 12.8 | 98 | 25.0 |
| Hypertension | 97 | 10.8 | 149 | 16.7 | 414 | 34.7 | 534 | 44.8 | 212 | 54.1 | 222 | 56.6 |
| Cardiac dis. | 12 | 1.3 | 32 | 4.3 | 99 | 8.3 | 234 | 19.6 | 133 | 33.9 | 207 | 52.8 |
| Pulmonary dis. | 33 | 3.7 | 34 | 3.8 | 118 | 9.9 | 114 | 9.6 | 79 | 20.2 | 70 | 17.9 |
| Cerebrovascular dis. | 5 | 0.6 | 8 | 0.9 | 34 | 2.9 | 55 | 4.6 | 37 | 9.4 | 50 | 12.8 |
| Neurological dis. | 23 | 2.6 | 28 | 3.1 | 45 | 3.8 | 53 | 4.4 | 18 | 4.6 | 25 | 6.4 |
| Cancer | 10 | 1.1 | 21 | 2.4 | 32 | 2.7 | 116 | 9.7 | 54 | 13.8 | 88 | 22.5 |
| Depression | 77 | 8.6 | 98 | 11.0 | 109 | 9.1 | 92 | 7.7 | 21 | 5.4 | 27 | 6.9 |
| LUTS medicationa | 4 | 0.5 | 53 | 5.9 | 70 | 5.9 | 339 | 28.4 | 115 | 29.3 | 205 | 52.3 |
| LUTS operationb | 0 | 0.0 | 1 | 0.1 | 4 | 0.3 | 43 | 3.6 | 20 | 5.1 | 41 | 10.5 |
| LUTS: lower urinary tract symptoms. | ||||||||||||
| aIncludes alpha-blockers, 5-alpha reductase inhibitors and anticholinergics, no initiations of mirabegrone as first-line treatment during the follow-up (not available until 2013); bendoscopic and surgical procedures during the follow-up for benign prostatic hyperplasia and overactive bladder listed in Table S1. | ||||||||||||
Association between symptom severity and bother
Frequency of persistent urgency increased with age (Figure 2). Of the 1,056 men (43%) with persistent mild urgency at follow-up, 6% (4.5–7.3) experienced moderate or severe bother with no differences between the age groups. Of the 132 men (5%) with persistent moderate or severe urgency at follow-up, 79% (71.7–85.9) experienced moderate or severe bother with no differences between the age groups (Table 2).
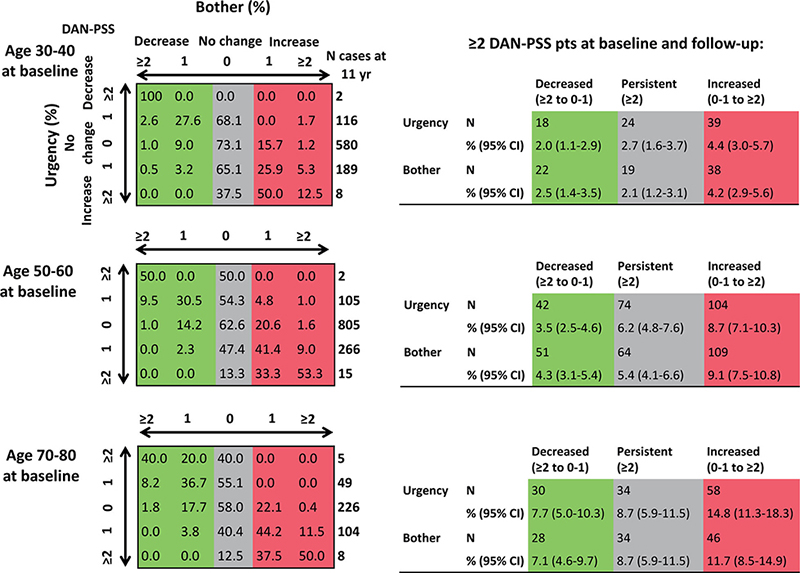
Figure 2. Course of urgency and associated bother at follow-up.
Fluctuation in urgency severity and bother was common, with either increase or decrease occurring in the majority of affected men (Figure 2). Of the 465 men (17%) with mild urgency at follow-up but not at baseline, the proportion of men experiencing moderate to severe bother at follow-up was highest in the oldest age group: 17% (8.4–25.8) among men aged 70–80 years (in 2004) compared with approximately 5% in the younger age groups. The proportion of men with moderate to severe bother at follow-up due to increased urgency was lowest in the youngest age group: 31% (15.6–45.9) among men aged 30–40 years, with 63% (53.0–72.0) in those aged 50–60 and 48% (35.0–61.5) at ages 70–80 years (in 2004). Similarly, the proportion of men reporting moderate to severe bother in spite of decreased urgency at follow-up was lowest in the youngest age group: 6% (0.0–17.3), while it was 19%–33% in the older men (Table 2). Between 2004 and 2014, a total of 607 men (27%) received either medication or surgery. Among the treated men, only 8% (6.2–10.7) experienced symptom resolution from at least moderate urgency to no or mild urgency. Among the 50 men with decreased urgency at follow-up and a history of LUTS treatment, the proportion of those reporting moderate to severe bother at follow-up was non-significantly higher compared to the 40 untreated men reporting bother in spite of decreased urgency: 28% (16.2–42.5) versus 13% (4.2–26.8).
Predictors of bother among men with persistent urgency
In logistic regression including 1,188 men with persistent urgency, that is stable mild or at least moderately severe urgency at follow-up, several factors were significantly associated with bothersome urgency including: severity of urgency, age older than 70 years, previously diagnosed diabetes, hypertension, cardiac disease, pulmonary disease, cerebrovascular disease, neurologic disease, depression and previous treatment of LUTS with medication or operation. In multivariable-adjusted logistic regression, severity of urgency remained strongly associated with bother in addition to previously diagnosed cardiac and pulmonary disease and a history of medically treated LUTS: the adjusted odds ratios were 55.2 (32.1–95.2, p < 0.001), 1.8 (1.0–3.1, p = 0.042), 1.9 (1.1–3.5, p = 0.026) and 2.7 (1.6–4.6, p < 0.001), respectively (Table 3). In subgroup analysis including 1,056 men with persistent mild urgency, cardiac disease was borderline significantly associated with increased bother, while pulmonary disease and medically treated LUTS remained significantly associated: the adjusted odds ratios were 1.9 (1.0–3.5, p = 0.053), 2.0 (1.0–4.0, p = 0.036) and 2.7 (1.5–4.9, p < 0.001), respectively (Table S2). For comparison, in multivariable-adjusted analysis of predictors of urgency independently of bother including all 2,480 men, older age, being single/widowed, previously diagnosed pulmonary disease as well as cerebrovascular disease, neurologic disease, depression and a history of medically treated LUTS were associated with at least moderately severe urgency at follow-up (Table S3).
| Bother ≥2 DAN-PSS pts at follow-up | Odds ratio | ||||||
| Unadjusted | Adjusted | ||||||
| % | 95% CI | OR | 95% CI | OR | 95% CI | p | |
| All (n = 1,188) | 14.0 | 12.0–15.9 | |||||
| Urgency ≥2 DAN-PSS pts | 78.8 | 71.7–85.9 | 59.5 | 35.6–100.6 | 55.2 | 32.1–95.2 | <0.001 |
| Age 50–60a | 14.4 | 11.7–17.1 | 1.1 | 0.8–1.5 | 0.8 | 0.4–1.4 | |
| Age 70–80a | 18.2 | 12.9–23.5 | 1.5 | 1.0–2.2 | 0.5 | 0.2–1.2 | |
| Single or widowed | 16.6 | 12.4–20.8 | 1.3 | 0.9–1.9 | 0.9 | 0.5–1.5 | |
| Obesityb | 14.9 | 10.3–19.5 | 1.1 | 0.7–1.7 | 0.6 | 0.3–1.1 | |
| Smokingc | 13.8 | 9.0–18.6 | 1.0 | 0.6–1.5 | 0.9 | 0.5–1.7 | |
| Diabetes | 22.5 | 16.3–28.7 | 2.0 | 1.3–3.1 | 1.1 | 0.6–2.0 | |
| Hypertension | 17.0 | 13.9–20.1 | 1.6 | 1.1–2.3 | 1.2 | 0.7–2.0 | |
| Cardiac dis. | 21.5 | 16.6–26.4 | 2.1 | 1.4–3.0 | 1.8 | 1.0–3.1 | 0.042 |
| Pulmonary dis. | 25.0 | 18.4–31.6 | 2.4 | 1.6–3.6 | 1.9 | 1.1–3.5 | 0.026 |
| Cerebrovasc. dis. | 26.6 | 16.6–36.5 | 2.4 | 1.3–4.2 | 1.1 | 0.5–2.4 | |
| Neurologic dis. | 26.7 | 16.4–36.9 | 2.4 | 1.3–4.2 | 1.3 | 0.6–3.2 | |
| Cancer | 15.5 | 9.2–21.8 | 1.1 | 0.7–1.9 | 0.7 | 0.3–1.4 | |
| Depression | 26.3 | 19.2–33.4 | 2.6 | 1.7–3.9 | 1.6 | 0.9–3.0 | |
| LUTS medicationd | 26.6 | 21.9–31.2 | 3.8 | 2.7–5.4 | 2.7 | 1.6–4.6 | <0.001 |
| LUTS operatione | 29.6 | 17.0–42.2 | 2.8 | 1.4–5.2 | 0.9 | 0.3–2.5 | |
| LUTS: lower urinary tract symptoms. | |||||||
| aAge at baseline, reference group aged 30–40, bBMI ≥30 at follow-up, ccurrent smoker at follow-up, dincludes alpha-blockers, 5-alpha reductase inhibitors and anticholinergics, no initiations of mirabegrone as first-line treatment during the follow-up (not available until 2013), eendoscopic and surgical procedures during the follow-up for benign prostatic hyperplasia and overactive bladder listed in Table S1. | |||||||
Discussion
During the 11-year follow-up, approximately 60% of the men had mild, that is occasional urinary urgency and the vast majority of them – over 90% – experienced no or mild bother. Furthermore, approximately 30% of the men younger than 50 years and up to 60% of men aged over 50 reported no or mild bother in spite of symptom progression. These findings suggest that mildly bothersome urgency can be considered a part of normal aging among men. However, in spite of high trends of care seeking for LUTS among older men – up to 50% of men aged over 70 having received medical treatment – the incidence of bothersome urgency increased with age suggesting treatment resistance due to frailty and comorbidity. The proportion of widowers and single men increases with age, but we found no evidence for an effect of marital status on bother. Among the few men – approximately 5% of the cohort – with urgency occurring frequently and as a long-term symptom, 80% experienced moderate or severe bother. Furthermore, approximately 10% of the men aged under 50 and up to 30% of men aged over 50 reported moderate or severe bother despite alleviated urgency at follow-up. This suggests that factors weakening men’s coping with urgency and causing treatment resistance to become more common with age. In addition, men with a history of medical treatment for LUTS or impaired cardiopulmonary health were substantially more likely to experience bother due to urinary urgency even with mild symptoms.
Few longitudinal population-based studies have evaluated the relation between changes of LUTS and symptom-specific bother. The comparison of the findings across studies is challenging due to variation in follow-up times, symptom definitions, as well as their assessment tools. A Scottish study evaluated the changes of various LUTS and symptom-specific bother assessed with the American Urological Association Symptom Index (AUA-SI) from baseline to 5-year follow-up in men aged 40–79 years [1]. They found that increase in bother was pronounced for all LUTS, and even a small increase in symptom level could cause a large increase in bother. Furthermore, the results suggested decreasing tolerance for symptoms over time. A US study utilized biennial assessments of symptoms with AUA-SI to evaluate changes of symptoms and associated bother during a 7-year follow-up among men aged 40–79 years [11]. Their results indicated that changes in symptom frequency and bother track closely together. However, some men did not report increased bother despite an increase in symptom frequency, which possibly represents adaption. Furthermore, a Japanese study used the International Prostatic Symptom score in a 15-year follow-up of men also aged 40–79 years [12]. Their study also showed a correlation between changes of LUTS and bother. In the previous studies, no detailed data on progression or resolution for symptom-specific bother in relation to changes of symptom severity was available for urinary urgency.
The strengths of our study include the rigorous symptom definitions based on a validated questionnaire and the comprehensive registry data on LUTS treatments. Instead of composite scores to assess the overall LUTS status, the present study investigated urgency separately, providing a patient-centered perspective for a symptom with major population-level burden, typically accompanied by various other LUTS and often considered when choosing treatments [10]. Furthermore, our study was able to utilize a long follow-up time with a broad age spectrum and, to our knowledge, is the first to explore predictors of urgency-specific bother in a longitudinal setting.
The main limitation of the study is the satisfactory, but suboptimal participation, being nearly 60% in 2004 and 50% in 2015. The proportion of eligible participants was further reduced to 39% due to inclusion criteria restricting the analyses only to men who had responded to the assessments of urgency both at baseline and follow-up, thus increasing the risk of selection bias. With the exception of LUTS treatments, the data on co-variables included in logistic regression were based on self-report and frequently imprecise and uncertain. Especially lower urinary tract malignancies, such as prostate cancer, would warrant inclusion in the analyses for their association with urgency-related bother. While detailed cancer data was not available, inclusion of any previously diagnosed cancer in the analyses can be justified by the impact of cancer diagnosis on men’s general symptom perception [19]. Some of the included men had a history of treatments, potentially modifying their coping with symptoms. However, our objective was to explore the relation between long-term symptoms and bother, not the occurrence of symptoms (or bother) in itself. We did not consider it likely that BPH treatments would importantly modify the relation between dysfunction and bother and therefore decided not to consider them in the analysis. Further, the numbers of men with specific treatment were too small for a meaningful analysis. Furthermore, taking into account the fluctuating nature of LUTS, the single re-evaluation of symptoms is a limitation. As bother is intrinsically subjective and cannot be evaluated in an objective, the results on symptom adaptation based on self-reported bother should be interpreted cautiously. This highlights the importance of a validated questionnaire in the assessments. While the long interval between symptom assessments can be regarded as a limitation, it can differentiate short-term fluctuation from long-term changes.
Understanding changes in symptom bother related to functional treatment response can guide clinical decision making. Treatment of urgency can be challenging due to uncertain course of bother, especially among older patients. Therefore, it is important to weigh the risks and benefits of the treatments and to consider the psychological aspects affecting men’s tolerance to symptoms especially among frail older men. Although long-term data on the effects of medical and surgical treatments for male LUTS is lacking [21–24], several treatment options – also other than medical or surgical – are available. These include behavioral modification, as well as physical training for pelvic floor dysfunction, and especially among frail older men, functional incidental training, including prompted voiding, for impaired motility and toileting skills [25, 26].
In conclusion, the vast majority of men with urinary urgency present with mild symptoms and bother. However, only one out of five men with persistent moderate or severe urgency adapts to his symptoms. Symptomatic men with a history of cardiac or pulmonary disease or medical treatment for LUTS tend to present with worse coping skills in terms of urinary urgency. This highlights the importance of including the assessment of general health in the management of male LUTS. Future investigations should address the impact of preventative health strategies on bothersome urinary urgency.
Acknowledgements
The TAMUS study was financially supported by Päivikki and Sakari Sohlberg Foundation and the Competitive State Research Financing of the Expert Responsibility area of Tampere University Hospital (9V065 and 9X055). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- [1] Lee A, Garraway W, Simpson R, et al. The natural history of untreated lower urinary tract symptoms in middle-aged and elderly men over a period of five years. Eur Urol. 1998;34:325–332. https://doi.org/10.1159/000019749
- [2] Berry S, Coffey D, Walsh P, et al. The development of human benign prostatic hyperplasia with age. J Urol. 1984;132:474–479. https://doi.org/10.1016/S0022-5347(17)49698-4
- [3] Gacci M, Vignozzi L, Sebastianelli A, et al. Metabolic syndrome and lower urinary tract symptoms: the role of inflammation. Prostate Cancer Prostatic Dis. 2013;16:101–106. https://doi.org/10.1038/pcan.2012.44
- [4] Mondul A, Giovannucci E, Platz E. A prospective study of obesity, and the incidence and progression of lower urinary tract symptoms. J Urol. 2014;191:715–721. https://doi.org/10.1016/j.juro.2013.08.110
- [5] Sexton C, Coyne K, Kopp Z, et al. The overlap of storage, voiding and postmicturition symptoms and implications for treatment seeking in the USA, UK and Sweden: EpiLUTS. BJU Int. 2009;103:12–23. https://doi.org/10.1111/j.1464-410X.2009.08369.x
- [6] Irwin D, Milsom I, Kopp Z, et al. Prevalence, severity, and symptom bother of lower urinary tract symptoms among men in the EPIC study: impact of overactive bladder. Eur Urol. 2009;56:14–20. https://doi.org/10.1016/j.eururo.2009.02.026
- [7] Chrischilles E, Rubenstein L, Chao J, et al. Initiation of nonselective alpha1-antagonist therapy and occurrence of hypotension-related adverse events among men with benign prostatic hyperplasia: a retrospective cohort study. Clin Ther. 2001;23:727–743. https://doi.org/10.1016/S0149-2918(01)80022-9
- [8] Heesakkers J, te Dorsthorst M, Wagg A. Safety and tolerability of fesoterodine in older adult patients with overactive bladder. Can Geriatr J. 2022;25:72–78. https://doi.org/10.5770/cgj.25.530
- [9] Taylor J, Harrison S, Assassa R, et al. The pattern and progression of lower urinary tract symptoms after transurethral prostatectomy compared with those seen in the general population. Eur Urol. 2007;51:1023–1029. https://doi.org/10.1016/j.eururo.2006.10.012
- [10] Agarwal A, Eryuzlu L, Cartwright R, et al. What is the most bothersome lower urinary tract symptom? Individual- and population-level perspectives for both men and women. Eur Urol. 2014;65:1211–1217. https://doi.org/10.1016/j.eururo.2014.01.019
- [11] Sarma A, Jacobsen S, Girman C, et al. Concomitant longitudinal changes in frequency of and bother from lower urinary tract symptoms in community dwelling men. J Urol. 2002;168:1446–1452. https://doi.org/10.1097/00005392-200210010-00035
- [12] Fukuta F, Masumori N, Mori M, et al. Natural history of lower urinary tract symptoms in Japanese men from a 15-year longitudinal community-based study. BJU Int. 2012;110:1023–1029. https://doi.org/10.1111/j.1464-410X.2011.10866.x
- [13] Koskimaki J, Hakama M, Huhtala H, et al. Prevalence of lower urinary tract symptoms in Finnish men: a population-based study. Br J Urol. 1998;81:364–369. https://doi.org/10.1046/j.1464-410x.1998.00565.x
- [14] Pöyhönen A, Häkkinen J, Koskimäki J, et al. Prevalence of hesitancy in 30–80-year-old Finnish men: Tampere Ageing Male Urological Study (TAMUS). BJU Int. 2012;109:1360–1364. https://doi.org/10.1111/j.1464-410X.2011.10443.x
- [15] Hansen B, Flyger H, Brasso K, et al. Validation of the self-administered Danish Prostatic Symptom Score (DAN-PSS-1) system for use in benign prostatic hyperplasia. Br J Urol. 1995;76:451–458. https://doi.org/10.1111/j.1464-410X.1995.tb07744.x
- [16] D’Ancona C, Haylen B, Oelke M, et al: The International Continence Society (ICS) report on the terminology for adult male lower urinary tract and pelvic floor symptoms and dysfunction. Neurourol Urodyn. 2019;38:433–477. https://doi.org/10.1002/nau.23897
- [17] Fitzgerald M, Link C, Litman H, et al. Beyond the lower urinary tract: the association of urologic and sexual symptoms with common illnesses. Eur Urol. 2007;52:407–415. https://doi.org/10.1016/j.eururo.2007.03.014
- [18] Kim S, Bang W, Choi H. Analysis of the prevalence and associated factors of overactive bladder in adult Korean men. PLoS One. 2017;12: e0175641. https://doi.org/10.1371/journal.pone.0175641
- [19] Dempster M, Howell D, McCorry N. Illness perceptions and coping in physical health conditions: a meta-analysis. J Psychosom Res. 2015;79:506–513. https://doi.org/10.1016/j.jpsychores.2015.10.006
- [20] August K, Sorkin D. Marital status and gender differences in managing a chronic illness: the function of health-related social control. Soc Sci Med. 2010;71:1831–1838. https://doi.org/10.1016/j.socscimed.2010.08.022
- [21] Cornu JN, Ahyai S, Bachmann A, et al. A systematic review and meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic obstruction: an update. Eur Urol. 2015;67:1066–1096. https://doi.org/10.1016/j.eururo.2014.06.017
- [22] Fusco F, Creta M, De Nunzio C, et al. Alpha-1 adrenergic antagonists, 5-alpha reductase inhibitors, phosphodiesterase type 5 inhibitors, and phytotherapic compounds in men with lower urinary tract symptoms suggestive of benign prostatic obstruction: a systematic review and meta-analysis of urodynamic studies. Neurourol Urodyn. 2018;37:1865–1874. https://doi.org/10.1002/nau.23554
- [23] Michel M, de la Rosette J. Role of muscarinic receptor antagonists in urgency and nocturia. BJU Int. 2005;96:37–42. https://doi.org/10.1111/j.1464-410X.2005.05651.x
- [24] Gacci M, Sebastianelli A, Spatafora P, et al. Best practice in the management of storage symptoms in male lower urinary tract symptoms: a review of the evidence base. Ther Adv Urol. 2017;10:79–92. https://doi.org/10.1177/1756287217742837
- [25] Hall L, Aljuraifani R, Hodges P. Design of programs to train pelvic floor muscles in men with urinary dysfunction: Systematic review. Neurourol Urodyn. 2018;37:2053–2087. https://doi.org/10.1002/nau.23593
- [26] Ouslander J, Griffiths P, McConnell E, et al. Functional incidental training: a randomized, controlled, crossover trial in Veterans Affairs nursing homes. J Am Geriatr Soc 2005;53:1091–1100. https://doi.org/10.1111/j.1532-5415.2005.53359.x