Abstract book for the 34th Congress of the Scandinavian Association of Urology (NUF)
PREFACE
The 34th Congress of the Scandinavian Association of Urology (NUF2023) took place in Bergen, Norway June 7-10th, 2023.
The organizers would like to thank all the contributors for their efforts to help elevate the scientific level of the meeting.
NUF2023 had an all-time high number of abstract submissions and acceptance. We hope this is a trend that will be carried over to the next meeting in Gothenburg in June 2025.
We also would like to express our gratitude to the Scandinavian Journal of Urology for the collaboration and publication of this abstract book.
Bergen - Norway, July 12th, 2023
The NUF2023 Organizing Committee
Christian Beisland (Congress president)
Bjarte Almås (Chief of the Scientific Committee)
Jannike Mohn
Øyvind Ulvik
Hanne Merete Landro
Gigja Gudbrandsdottir
Karin M. Hjelle
Stine Nøttveit
Patrick Juliebø-Jones
Rachel Maheswaran
Peder Gjengstø
Citation: Scandinavian Journal of Urology 2023, VOL. 58, Supp. 222. https://doi.org/10.2340/sju.v58.18375.
Copyright: © 2023 The Author(s). Published by MJS Publishing on behalf of Acta Chirurgica Scandinavica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Published: August 13, 2023
ABSTRACTS
SESSION I - ORAL PRESENTATIONS – PROSTATE
AS-1.001
High yield isolation of circulating tumour cells to identify adaptive treatment responses in prostate cancer
Rudolfsson S1, Thellenberg Karlsson C2, Wikström P3, Stoecklein N4, Toss F5, Magnusson C6, Laurell T7, Welén K8, Josefsson A9
1Surgery and perioperative sciences, Urology, Umeå, Sweden, 2Umeå University, Department of radiation therapy, Umeå, Sweden, 3Umeå University, Department of medical bioscience, Umeå, Sweden, 4Heinrich Heine University Düsseldorf, Department of General, Visceral and Pediatric Surgery, Düsseldorf, Germany, 5Umeå University, Department of Clinical Microbiology, Clinical Immunology, Umeå, Sweden, 6Lunds University, Department of Clinical Chemistry, Lund, Sweden, 7Lunds University, Department of Biomedical Engineering, Lund, Sweden, 8Univeristy of Gothenburg, Department of clinical sciences, Urology, Gothenburg, Sweden, 9Umeå University, Surgery and preoperative sciences, Umeå, Sweden
Background: Liquid biopsies utilizing circulating tumour cells (CTCs) - which reflect the metastases - show great potential as a tool for precision medicine. The overall goal is to overcome current limitations and implement CTC-based precision medicine in prostate cancer.
Methods: Patients at the Urology clinic at University Hospital of Umeå with either metastasized disease at diagnosis or PSA relapse following surgery are included in this prospective clinical study. By using the clinically available apheresis methodology, nucleated cells including CTCs are “harvested” from the whole blood volume. Aliquots of the fresh apheresis product is processed for CTC isolation include by a label free acoustophoresis method CellSearch, AdnaTest. We will also perform both whole transcriptomic profiling and single cell RNA and DNA sequencing.
Results: AcouWash protocol using spiked-in GFP transfected PC3-cells at different concentration gave a recovery rate between 60-80% and purity in the center outlet is increased at least 35x compared to the inlet sample. The apheresis product (50-100 ml) from the whole volume contains 1000-10000 times more CTCs compared to the CellSearch protocol using only 5 ml blood sample. We have further identified CTCs by apheresis and acoustophoresis also in the PSA relapse situation where imaging by PSMA-PET and CTC detection with CellSearch were negative. We are by the protocol able to freeze and thaw apheresis product for acoustophoresis and/or FACS with possibility to achieve transcriptomic profiling. CTCs isolated by acoustophoresis and AdnaSelect show similar profiles by whole transcriptomics.
Conclusions: We show the first results of a method using clinically available apheresis combined with a scalable label-free method, indicating the possibility to achieve molecular subtyping of CTCs from a patient before metastases are detectable, enabling precision medicine at an early state of metastatic disease.
AS-1.002
Survival and biomarkers in a prospective non-randomized phase I trial of dendritic cell-based (DC) cryoimmunotherapy (CryoIT) combined with checkpoint inhibitors in metastatic castration resistant prostate cancer (mCRPC)
Thomsen L C V1, Honorè A2, Reisæter L A R3, Almås B2, Børretzen A4, Helle S I5, Førde K2, Kristofersen E K6, Kaada S H6, Melve G K6, Haslerud T M3, Biermann M3, Bigalke I7, Kvalheim G7, Azeem W8, Olsen J R8, Gabriel B8, Knappskog S9, Halvorsen O J10, Akslen L A10, Pantel K11, Riethdorf S11, Gjertsen B T1, Øyan A M8, Kalland K-H1, Beisland C2
1University of Bergen, Centre for Cancer Biomarkers CCBIO, Department of Clinical Science, Bergen, Norway, 2Haukeland University Hospital, Department of Urology, Bergen, Norway, 3Haukeland University Hospital, Daprtment of Radiology, Bergen, Norway, 4Haukeland University Hospital, Department of Pathology, Bergen, Norway, 5Haukeland University Hospital, Department of Oncology, Bergen, Norway, 6Haukeland University Hospital, Department of Immunology and Transfusion Medicine, Bergen, Norway, 7Oslo University Hospital, Department of Cellular Therapy, Oslo, Norway, 8University of Bergen, Department of Clinical Science, Bergen, Norway, 9University of Bergen, K.G. Jebsen Center for Genome-Directed Cancer Therapy, Department of Clinical Science, Bergen, Norway, 10University of Bergen, Centre for Cancer Biomarkers CCBIO, Department of Clinical Medicine, Bergen, Norway, 11Universitätsklinikum Hamburg-Eppendorf, Institut Für Tumorbiologie, Zentrum Für Experimentelle Medizin, Hamburg, Germany
Background: In this trial, mCRPC patients were treated with DC-based CryoIT as monotherapy or combined with checkpoint inhibitors, enabling systemic attacks on heterogenous cancer cells by lymphocytes introduced to tumor-associated antigens. Primary endpoints showed that the treatment was safe. The secondary aims included survival and biologic outcomes.
Methods: mCRPC patients (n=18) progressing on standard treatment were included. After prostate cancer tissue biopsy and cryoablation, autologous immature DCs were injected intratumorally. Doses were escalated in a 3+3 design (n=9) followed by dose expansion combined with either ipilimumab (n=6) or pembrolizumab (n=3). Progression was evaluated by PSA and PET/CT, MRI and bone scintigraphy at 14, 22 and 46 weeks (by iRECISTv1.1). Biologic findings were examined according to treatment response. Pre-treatment cancer tissues were examined for leukocytes by immunohistochemistry (IHC). Ultradeep T-cell receptor (TCR) sequencing quantified T-lymphocyte clonotypes before treatment and during follow-up.
Results: At data cut-off median OS and PFS were 40.7 and 10.5 months, respectively. Of the 8 patients still alive 43 to 85 months post-CryoIT, 7 had progressed and received other treatment. Early decreases in PSA (p=0.002) and LDH (p=0.01) levels 6 weeks after CryoIT indicated better outcomes at 22 weeks. All patients had aggressive cancer, with ISUP grade group 4 or 5 at inclusion. At baseline, higher serum ALP correlated with higher regulatory T-cells (p=0.047), FoxP3+/CD3+ratios (p=0.014) and FoxP3+/CD8+ratios (p=0.004) in tissues. Longer OS correlated with lower tissue ratios of CD4+/CD3+cells (p=0.002) and CD4+/CD8+cells (0.007). TCR sequencing revealed a high incidence of new T-cell clonotypes after treatment in all patients.
Conclusions: CryoIT demonstrates non-inferior OS and PFS compared to other mCRPC trials. Lower CD4+cell fractions of lymphocytes on IHC indicate better OS and immune activation was suggested by high incidence of new T cell clones after CryoIT.
AS-1.003*
Cholesterol lowering simvastatin enhances the efficacy of anti-androgen treatment in treatment-resistant prostate cancer cells
Siltari A1,2, Korhonen O3, Välitalo K3, Raittinen P3, Bläuer M3, Syvälä H3, Tammela T L2,3, Murtola T J3,4
1Tampere University, Prostate cancer research center, Tampere, Finland, 2Tampere University Hospital, Department of Urology, Tampere, Finland, 3Tampere University, Tampere, Finland, 4Tampere University Hospital, Tampere, Finland
Background: Bicalutamide (Bic) and enzalutamide (Enza) are androgen receptor (AR) signalling inhibitors (ARSIs) that are commonly used in the treatment of castration-resistant prostate cancer (CRPC). However, the development of treatment resistance by prostate cancer (PCa) cells remains a major clinical challenge. Recent research has suggested a link between androgen signalling and lipid and cholesterol metabolism, which may contribute to the development of treatment resistance. While statins are known to inhibit the cholesterol-producing mevalonate pathway, it is unclear whether statin treatment could enhance the efficacy of ARSIs in treating CRPC.
Methods: We examined the combined impact of simvastatin (Sim) with or without Bic or Enza on VCaP-derived PCa cell lines that were resistant to these ARSIs. We evaluated changes in cell growth, stage of cell cycle, gene expression, and protein expression for AR signalling and cholesterol metabolism.
Results: The combination treatment with Sim + Bic/Enza reduced cell growth more than Sim alone in Bic or Enza-resistant cell lines. In Bic and Enza-resistant cells, the combination treatment upregulated 60 and 26 genes and downregulated 33 and 48 genes, respectively, compared to control cells. In total, 16 genes expression were altered similarly in both cell lines in response to combination therapy. Over 70% of all gene changes were found on AR-regulated genes.
Conclusions: We demonstrated that combined treatment with ARSI and Sim was more effective in inhibiting cell growth than Sim alone in ARSI-resistant cell lines. This indicates that inhibiting the mevalonate pathway may enhance androgen signaling inhibition and potentially overcome ARSI resistance mechanisms. This phenomenon is supported by epidemiological studies indicating that patients treated with anti-androgens had better outcomes when simultaneously treated with statins. Further studies are needed to determine whether interventions in lipid and cholesterol metabolism can improve the treatment of CRPC.
*Winner of third prize for best abstract in the field of Urologic cancer
AS-1.004
Association Between Regional Tradition of Uptake of active surveillance (AS) for Prostate Cancer in Sweden, and Long-Term Outcomes of AS
Ahlberg M1, Garmo H2,3, Holmberg L2,4, Bill-Axelson A2
1Uppsala University Hospital, Department of Surgical Sciences, Uppsala, Sweden, 2Uppsala University, Department of Surgical Sciences, Uppsala, Sweden, 3Regional Cancer Center Uppsala/Örebro, Uppsala, Sweden, 4King’s College London, School of Cancer and Pharmaceutical Sciences, London, United Kingdom
Background: Geographical differences in uptake of active surveillance (AS) for low- and intermediate-risk prostate cancer illustrates inequality in treatment strategy. The aim of this study was to investigate the association between regionally bound differences in AS uptake and transition from AS to radical treatment, start of androgen deprivation therapy (ADT), watchful waiting, or death.
Methods: Men in the National Prostate Cancer Register in Sweden with low- and favorable intermediate-risk prostate cancer who started AS from Jan 1st, 2007, to Dec 31st 2019 were included in the study. The exposure was the regional tradition of immediate radical treatment defined as three groups with a regional tradition of low, intermediate, or high proportion immediate radical treatment. We analysed the association between the proportion immediate radical treatment and the outcome defined as the probability of transition from AS to radical treatment, start of ADT, watchful waiting and death from other causes. We made a sensitivity analysis of the added effect of early transition from AS to radical treatment the first three years of AS.
Results: In all, 13679 men starting AS with a median age of 66 years and a median PSA of 5.1 ng/ml were followed in median 5.7 years. Men from regions with a high uptake of AS, had lower probability of transition to radical treatment (36%) compared with men from regions with low uptake of AS (40%) (absolute difference 4.1% (95% CI 1.0-7.2)), but not a higher probability of AS failure defined as start of ADT (absolute difference 0.4% (95% CI -0.7-1.4)). There was no significant difference in probability of transition to watchful waiting or death from other causes between the groups.
Conclusions: A tradition of high uptake of AS is associated with lower probability of transition to radical treatment but not with higher risk of AS failure. Low uptake of AS suggests overtreatment.
AS-1.005
Robot-assisted Radical Prostatectomy with the HUGO Robotic System: Initial Experience in Helsinki University Hospital
Matikainen M, Kilpeläinen T, Pétas A, Santti H, Rannikko A
Helsinki University Hospital, Department of Urology, Helsinki, Finland
Background: Robotic-assisted surgery in urology is well-established worldwide. We describe the perioperative results of the first 44 robot-assisted radical prostatectomies (RARPs) performed between January 12 and March 14, 2023, using the HUGO™ RAS system (Medtronic, Minneapolis, MN, USA) at Helsinki University Hospital, Finland. Before HUGO RAS platform we have used DaVinci platforms at our institution in > 4700 robotic-assisted surgeries since 2009.
Methods: After official training for the entire OR team, 44 patients underwent RARP, 13 of whom also underwent lymph node dissection (LND). Clinical characteristics, surgical time points, and peri- and postoperative data were collected from the hospital’s EHR system. Preoperatively, three patients were staged as cT3, nine cT2 and 32 cT1c. 26 of the men had ISUP Grade (GG) 2 disease, nine GG 3, five GG 4 and four GG 5. Median PSA was 7.6 ug/L (range 3.8 - 30.3) and median prostate size was 35 cm3(range 17 – 81). Median BMI of the patients was 26 (range 22 – 32). Five urologists performed the procedures.
Results: All procedures were completed as planned, with no conversions or placement of additional ports. Minor technical failures, such as malfunction in robot arms or in instruments, were recorded 10 times, but system functions were restored perioperatively in all cases. Only one ≥Clavien 3 complication (ureteric obstruction) was observed postoperatively in a man with significant adhesions and fibrosis a in the surgical field. Median blood loss was 200 ml (range 20-550ml). Median length of hospital stay was one day. All surgeons seem to follow the same learning curve for console time. System start-up and docking were relatively rapid, and increasingly accelerating processes for a properly trained surgical team.
Conclusions: Our initial experience shows the safety and feasibility of RARP with the HUGO RAS system in our hospital and provides data on the learning curve and perioperative results that may help early adopters of this platform.
AS-1.006
Positive surgical margin and oncological outcomes after RALP in different CAPRA-risk groups with a minimum follow up of 10 years
Hagman A1, Lantz A1, Carlsson S1, Akre O1, Olsson M1, Egevad L2, Wiklund P1
1Karolinska Institutet, Department of Molecular Medicine and Surgery, Stockholm, Sweden, 2Karolinska Insititutet, Department of Oncology and Pathology, Stockholm, Sweden
Background: A positive surgical margin (PSM) might increase the risk of having an adverse oncological outcome. There are no studies investigating the impact of PSM’s extent and preoperative risk groups on oncological outcomes in long-term follow up after robot-assisted radical prostatectomy (RALP).
Methods: Retrospective cohort study of 1039 patients subjected to RALP for localized prostate cancer (PCa) at a single European institution between 2002 and 2007. PSM was stratified by extent (focal/extensive). CAPRA-score was used for risk group stratification. BCR was defined as postoperative PSA>0.2 ng/mL. Additional treatment was defined as salvage radio therapy (RT) and/or androgen deprivation therapy (ADT).
Results: A total of 227 patients had a PSM (21.8%). When compared to a negative surgical margin, an extensive PSM was associated with an increased risk of BCR (HR 2.16 (2.09-8.29), 3.76 (2.33-6.06), 2.35 (1.03-5.38)) and RT (HR: 3.75 (1.45-9.7), 4.57 (2.47- 8.43), HR: 9.32 (1.06 -14.82)) in low intermediate and high-risk groups, respectively. For patients with a focal positive margin the high-risk group showed an increased risk of BCR (HR 5.79 1.62-20.65), RT (HR 9.32 1.7-50.95) and ADT (HR 4.11 1.08-15.57) whereas in low-risk and intermediate risk patients a modest effect on BCR but no significant effect on RT or ADT was found.
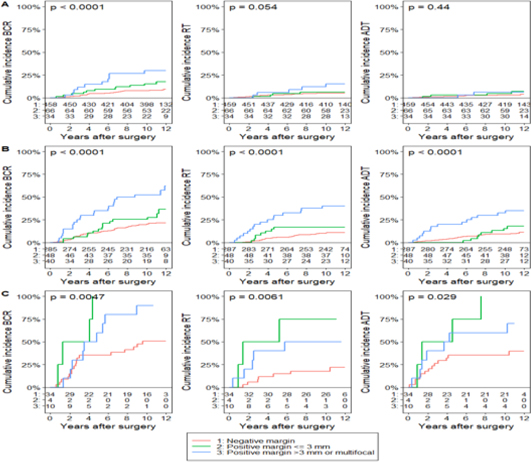
Figure 1. Cumulative incidence plots of BCR, RT and ADT for CAPRA risk groups A: Low risk, B: Intermediate risk, C: High risk and PSM.
Conclusions: While an extensively positive surgical margin is associated with an increased risk of recurrence in all risk groups, a focal PSM was associated with additional treatment only among men with high-risk tumours. Prioritizing urinary and sexual function while tolerating focal positive margins may therefore be considered among men with low and intermediate risk tumours.
AS-1.007
Unifocal prostate cancer: a more aggressive entity associated with increased risk of biochemical recurrence in the first year after radical prostatectomy
Aas K1,2, Bogaard M3,4, Myklebust T Å5,6, Axcrona K1,4, Axcrona U3,4, Skotheim R4,7
1Akershus University Hospital, Department of Urology, Lørenskog, Norway, 2University of Oslo / Institute of Clinical Medicine, Oslo, Norway, 3Oslo University Hospital Radiumhospitalet, Department of Pathology, Oslo, Norway, 4Oslo University Hospital Radiumhospitalet / Institute for Cancer Research, Department of Molecular Oncology, Oslo, Norway, 5Cancer Registry of Norway, Oslo, Norway, 6Møre and Romsdal Hospital Trust, Department of Research and Innovation, Ålesund, Norway, 7University of Oslo / Faculty of Mathematics and Natural Sciences, Department of Informatics, Oslo, Norway
Background: The aim of this study was to compare clinicopathological features of unifocal and multifocal prostate cancer (PCa) and to study the association between tumour focality and early biochemical recurrence (BCR) in men treated with radical prostatectomy (RP).
Methods: A multi-sampled, prospective cohort of treatment-naïve men treated with RP in a tertiary referral centre in 2010–2012. Median follow-up was 8.1 years. The χ2 test of independence or Fishers exact test was used to compare categorical variables and the Wilcoxon rank sum for continuous variables. Multivariable Cox regression analyses assessed the association of tumour focality and BCR within one year of RP. A p-value of < 0.05 was considered statistically significant.
Results: In total, 515 patients were included. Unifocal tumours were identified in 33% (171/515) and multifocal in 67% (344/515) of patients. Unifocal tumours showed more adverse pre-operative features (higher PSA, more extensive local tumour growth on digital rectal examination and MRI, higher ISUP grade groups) and pathological findings in the specimens (positive surgical margins, pathological T- and N-category). Overall, 38 patients experienced BCR in the first year. On multivariate Cox regression analyses, patients with unifocal tumours had an increased risk of BCR (HR 2.45, 95% CI 1.11-5.42) compared to men with multifocal disease.
Conclusions: Unifocal prostate cancers have more adverse clinicopathological features and are associated with increased risk of early BCR after RP compared to multifocal cancers. These findings may impact PCa risk stratification.
AS-1.008
Additional treatment in patients with ISUP (International Society of Urological Pathology) grade
group (GG) 5 after radical
prostatectomy (RP)
Ilstad H, Eri L M, Qvigstad L F, Berge V
University of Oslo, Institute of Clinical Medicine, Department of Urology, Oslo, Norway
Background: During recent years, there has been a steady increase in the number of patients with ISUP GG 5 in the RP specimen at our institution. The aim of this study is to assess the frequency of postoperative radiation therapy (RT) and/or permanent androgen deprivation therapy (ADT) in the follow up of this high-risk group.
Methods: Patients operated with RALP (Robot Assisted Laparoscopic Radical Prostatectomy) during 2009–2021 and with ISUP GG 5 in the surgical specimen were identified in our prospective prostate cancer registry. The occurrence and timing of postoperative RT and permanent ADT was registered. Adjuvant ADT in connection with postoperative RT is not recorded. Survival time free of salvage RT (sRT) and ADT was estimated by Kaplan-Meier (KM) curves.
Results: 406 patients were identified. Twenty-seven patients operated with salvage RALP were excluded. Of the remaining 379 patients, 34 patients (9%) died during the study period, 17 patients died due to prostate cancer. 143 patients (38%) were without postoperative RT and ADT with median follow up (FU) 53 months (range 29–159 months). Thirty-four patients (9%) had adjuvant RT defined as RT for patients with PSA < 0.2 ng/ml at 3 months post-RALP. 142 patients (38%) had sRT. KM curves showed 93 months (95% CI: 84 – 101 months) as mean time for start of sRT (Figure 1). Similarly, 108 patients (29%) started permanent ADT and mean time for start of ADT was 111 months (95% CI: 104 – 118 months). Fifty patients (13%) had sRT followed by permanent ADT.
Conclusions: There is a high risk for sRT and ADT in patients with ISUP GG 5 in the RP specimen.
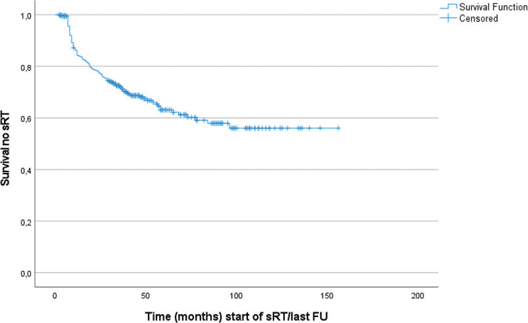
Figure 1. Kaplan-Meier curve sRT free survival.
AS-1.009
Management of functional outcomes after radical prostatectomy in the Nordic countries: A survey of uro-oncological centers
Nolsøe A B1, Oestergren P B1, Holm H V2, Murtola T J3, Fode M1
1Copenhagen University Hospital, Herlev and Gentofte Hospital, Department of Urology, Herlev, Denmark, 2Oslo University Hospital Rikshospitalet, Department of Urology, Oslo, Norway, 3TAYS Cancer Center, Tampere, Department of Urology, Tampere, Finland
Background: To describe the clinical practice regarding erectile dysfunction (ED) and urinary incontinence (UI) after radical prostatectomy (RP) in the Nordic countries.
Methods: A 37-item online survey about pre- and post-RP evaluation and rehabilitation of sexual and urinary function was sent to 42 uro-oncology centers.
Results: Twenty-seven centers in Denmark (n=6), Norway (n=8), Finland (n=7), and Sweden (n=6) responded (64.3%). Sexual function was evaluated by 24 centers both before and after RP. One center only evaluated function before RP and 1 center only did so after. The majority used validated questionnaires. Pre-RP urinary function was evaluated by 25 centers and post-RP function by 24 centers. Again, the majority used validated questionnaires, but objective measures (uroflowmetry, residual urine volume, and/or pads per day) were also used by 9 centers pre-operatively and 9 centers post-operatively.
Twenty-one centers offered sexual rehabilitation but only 12 described their protocols. In all cases, men undergoing nerve-sparing RP were offered PDE5Is. In 2 centers this was combined with a vacuum erection device (VED). Three centers offered second-line treatment with either VED, injections, or urethral suppositories. Finally, 2 centers offered a third line of injections. Two centers offered rehabilitation to patients who had undergone non-nerve-sparing surgery and 1 center reported to offer a consultation with a sexologist.
Twenty-three centers provided pelvic floor muscle training via a physiotherapist. In 4 centers this was done preoperatively and in 16 centers it was offered to all patients following RP. The last 3 centers provided training to men with UI. One additional center used medical support with duloxetine, while 1 center stated to offer support for UI without providing details.
Conclusions: There are vast differences regarding evaluation and rehabilitation of ED and UI related to RP in the Nordic countries.
AS-1.010
One-year post-RALP urinary function in men ≥ 70 years
Qvigstad L F1, Aas K2, Fosså S3, Eri L M1, Diep L M4, Berge V5
1Oslo University Hospital, Urology, Oslo, Norway, 2Akershus University Hospital, Urology, Nordbyhagen, Norway, 3Oslo University Hospital, Onclogy, Oslo, Norway, 4Oslo University Hospital, Regional Forskningsstøtte, Oslo, Norway, 5Oslo University Hospital, Department of urology, Oslo, Norway
Background: During the last 15 years RALP has increasingly been performed in men aged ≥ 70 years. Our multivariate analyses assess the impact of age of the patient undergoing RALP (Robot assisted laparoscopic radical prostatectomy) on urinary function 12 months post-RALP.
Methods: Data was based on 1494 patients who responded to EPIC26 questions at baseline and 12 months after RALP. The answers were transformed into scales ranging from 0 (worst) to 100 (best) and summary score of urinary incontinence and of urinary irritative/obstructive score was constructed. A score ≥ 80 represented continence for urine. Postoperative increase of the urinary irritative/obstructive score by ≥ 5 points indicated clinical relevant improvement. Level of significance: p<0.05.
Results The mean summary score of urinary incontinence at 12 months was 75 (SD 25). The mean decrease in score from baseline for men < 70 years and ≥ 70 years was 19 (SD 25) and 21 (SD 27), respectively (p=0.08). The mean summary score of irritative/obstructive score at 12 months was 89 (SD 12). The mean improvement from baseline for men < 70 years and ≥ 70 years was 5 (SD 15) and 7 (SD 15), respectively (p=0.02). In multivariate logistic regression age group was not statistically significant associated with urinary continence. Nervesparing was associated with improved urinary continence while comorbidity was associated with decreased urinary continence. Improvement of irritative/obstructive voiding symptoms was associated with preoperative prostate volume.
Conclusions: One-year post-RALP urinary function in patients ≥ 70 years of age at RALP was similar with patients < 70 years. Irritative/obstructive voiding symptoms improved in both age groups.
AS-1.011
Changes in urinary function following robot-assisted radical prostatectomy: A longitudinal study of men with prostate cancer (The HAARP-Study)
Alison B1#, Alhusseinawi H2,3#, Collinson E4, Robson W4, Christopher H4, Drinnan M3, Aning J5
1The Newcastle upon Tyne Hospitals NHS Foundation Trust, Department of medical physics, Newcastle, United Kingdom, 2Aalborg University Hospital, Department of Urology, Aalborg, Denmark, 3Aalborg University, Department of Clinical medicine, Aalborg, Denmark, 4The Newcastle upon Tyne Hospitals NHS Foundation Trust, Urology and Renal Services Directorate, Newcastle, United Kingdom, 5North Bristol NHS Trust, Bristol Urological Institute, Bristol, United Kingdom
Background: To investigate changes in urinary function and quality of life in men undergoing robot-assisted radical prostatectomy (RARP) to treat prostate cancer.
Methods: We conducted a prospective observational study between October 2018 and February 2019. Fifty-five patients were enrolled at 2 centres, 33 participants were included in the final data analysis. Primary outcome included changes in urinary flow rate (Qmax), while secondary outcomes included changes in urinary frequency, nocturia, voided volume, and completion of two validated questionnaires, (ICIQ-MLUTS) and (FACT-P). Questionnaires were collected before surgery and at 3- and 12-months post-surgery.
Results: Qmax significantly improved after RARP at three and 12 months. Changes from baseline were 2.67 mL/s (95%CI: 0.42-5.35 mL/s) (p=0.02), and 3.57 mL/s (95%CI: 1.25-5.23 mL/s) (p=0.003), respectively. Urinary frequency significantly decreased after 12 months also, -1.0 (95%CI: -1.8 to -0.3) (p=0.01). There was a statistically significant decrease in voided volume at 3 months, -35.7 mL (95%CI: -55.1 to -17.2) (p=0.001), with a return to pre-surgery status by 12 months. No statistically significant changes in fluid intake were noted in the cohort ( p=0.17). There were no statistically significant changes in the number of night-time voids(p=0.30) or the ICIQ-MLUTS scores(p=0.14). There were also no statistically significant changes in FACT-P total score at either three or 12 months(p=0.50). Analysis of ICIQ-MLUTS domains shows worsening in the incontinence score during three and twelve months, 3.4 (95%CI2.1-4.6) (p=0.001), 1.9 (95%CI: 0.7-3.1) (p=0.002) respectively, accompanied by improvement in the voiding function throughout the observation period -1.4 (95%CI:-2.5- -0.3))(p=0.01)-1.8 (-2.9- -0.7)(p=0.001)
Conclusions: Our study suggests that RARP may significantly improve Qmax and voiding symptoms. Worsening incontinence symptoms accompany this improvement. This information may be used to counsel men undergoing RARP.
# Authors contributed equally
SESSION II - ORAL PRESENTATIONS – BLADDER
AS-2.012
Intradetrusor injection with botulinum toxin A (BTX) in children at Haukeland University Hospital (HUH) from 2001-2020
Myskja M, Bergesen A, Beisland C, Gudbrandsdottir G, Roth I, Hjelle K M
Haukeland University Hospital, Department of Urology, Bergen, Norway
Background: High intravesical pressure impose a threat to kidney function and quality of life in children and adolescents with neurogenic bladders. Treatment options in this group have been limited. As BTX is an established treatment in adult neurogenic bladder, we aimed to evaluate our practice patterns regarding BTX in children and adolescents at HUH
Methods: Retrospective registration identified 18 patients (≤ 18 years) treated with intradetrusor injection with BTX from 2001-2020. Data was retrieved from medical records as part of a clinical audit, and is exempt from requirement of ethical approval
Results: Median age was 10 years (IQR 5-15). Two of the patients had idiopathic overactive bladder and 16 were diagnosed with neurogenic bladder (13 myelomeningoceles, two spinal cord injuries, one cerebral palsy). Cystometry was performed pre-BTX treatment in all patients and in 17 during follow-up (FU) cystometry. There was significant reduction in both maximum detrusor pressure during filling (from 53 cmH2O to 29 cmH2O) and increased cystometric capacity (from 256 to 303 ml), p=0.02 and p=0.01, respectively (paired T-test). Fifteen patients had their first BTX-injection done in general anesthesia and three in local anesthesia. Nine patients are still on BTX treatment. Six patients terminated treatment due to either urinary diversion, or to lack of indication or effect. The last three were referred to another hospital.
In 67 % of the patients, the BTX start dose was 200 IU and lower in 33%. Eight patients needed later dose escalation. FU time for patients still under BTX treatment (n=9) was median 7 years (IQR 3-13). No complications requiring hospitalization has been registered.
Conclusions: Intradetrusor injection with BTX is a safe and effective treatment also in children and adolescents with overactive bladder both due to neurological and idiopathic overactivity. Thorough selection of patients and a careful follow up is needed.
AS-2.013
Patient preference regarding local anesthesia versus sedation/general anesthesia during intravesical treatment with Botulinum Toxin A (Botox) for overactive bladder (OAB)
Bryde Laursen R, Petersen H, Thiele I-M, Schou J
Herlev/Gentofte Hospital, Department of Urology, Copenhagen, Denmark
Background: The aim was to evaluate the optimal anesthesia regimen in relation to treatment with intravesical Botox.
Methods: One hundred patients planned for Botox treatment in our department were offered and accepted treatment in an out-patient setting from May 2017-February 2018. The procedure was carried out in only gel-anesthesia (Instillagel) and via a flexible cystoscope. 100-300 IE Botox were dissolved in 10 ml of saline, and the drug were distributed in 10 depots of 1 ml. Average procedure time: 4-5 minutes. All 100 treatments were performed by the same doctor and nurse.
After the procedure, the patients filled in a questionnaire comprising of eight questions including a Visual Analog Scale (VAS). Demographics: 59 females and 41 males were treated. Age 30-79 years. Two failed the questionnaire and were excluded. Of the remaining 98 patients, 27 were Botox-treatment naïve.
Results: Pain: (VAS-scale 0-10). Score 0-1: 32%, 2-3: 30%, 4-5: 22% and 6-10: 15%. Overall satisfaction with the procedure: Rated 1-10 with 10 being best. 93 % found the outpatient treatment fully satisfying (9-10); 4% rated 7-8; and 3% 1-4. Eighty-four % of females and 98 % of males were satisfied with the preoperative oral and written information about risk of urinary retention and 98 % of all patients were satisfied with information on pain, bleeding, and other complications.
Conclusions: A vast majority of patients (at least 93%) preferred to have Botox treatments in the outpatient clinic in the future. The patients are willing to accept slight or moderate pain in a few minutes, in order to avoid time – and resource – consuming admission to the hospital ward. A thorough preoperative information is crucial. These findings have totally changed our mindset, so now the standard offer to Botox-naïve patients is a procedure in gel anesthesia. If this is not tolerated, the patient will be offered sedation/general anesthesia with the following treatments.
AS-2.014*
Adjustable transobturator male system (ATOMS) for post-prostatectomy incontinence: Outcomes from a tertiary center over 10 years
Roth I, Beisland C, Juliebø-Jones P, Hjelle K M
Helse Bergen, Department of Urology, Bergen, Norway
Background: The adjustable transobturator male system ( ATOMS ) implant is an established surgical treatment for patients with urinary incontinence post-prostatectomy. Our objective was to evaluate the outcomes in patients receiving this minimally invasive intervention at our center.
Methods: Retrospective analysis was performed for all patients undergoing this procedure at Haukeland University Hospital, a tertiary referral center in Western Norway. Outcomes of interest included operative complication rate, explantation rate and continence recovery. Information was also collected on baseline demographics as well as operative time, length of stay and number of adjustments required. The study was registered as a departmental clincal audit and it was therefore exempt from a requirement for ethical approval accordingly.
Results: Overall, 118 patients underwent ATOMS surgery between 2012 and 2022. Median age at prostatectomy and ATOMS surgery was 64 years (IQR 60-68) and 67 years (IQR 65-70), respectively. Median operative time was 39 minutes (IQR 33-45) and 86% of the patients required only one night stay in the hospital. No intra-operative complications were recorded. At two month follow up, 22% had experienced transient pain in the perineum while only 4% reported persistent pain. The mean pre- and post-treatment pad-weight/day was 225 g and 38g, respectively. Ninety patients experienced no leakage while only 10 patients reported leakage exceeding 50 g a day. The mean number of adjustments was two per patient while 28% required none at all. Fifteen percent (n=18) of the study sample required re-operation. This included port adjustments/removals (n=9), conversion to AMS800 (n=3) and complete removal due to pain, erosion, or infection (n=6).
Conclusions: Our results support ATOMS as an effective treatment option for post-prostatectomy incontinence, which also maintains a low morbidity profile. Careful patient selection and thorough counselling prior to surgery allow for outcomes to be optimised accordingly.
*Nominee for best abstract in the field of benign Urology
AS-2.015
Location of retroperitoneal lymph node metastases in upper tract urothelial carcinoma – results from a prospective lymph node mapping study
Bobjer J1,2, Gerdtsson A1,2, Abrahamsson J1,2, Baseckas G2, Bergkvist M3, Bläckberg M4, Brändstedt J1,2, Jancke G5, Hagberg O1,2, Kollberg P6, Lundström K-J6,7, Löfgren A1,2, Nyberg M1,2, Rian Mårtensson L8, Saemundsson Y1,2, Ståhl E1,2, Sörenby A1,2, Warnolf Å1,2, Liedberg F1,2
1Lund University, Institution of Translational Medicine, Malmö, Sweden, 2Skåne University Hospital, Department of Urology, Malmö, Sweden, 3Karolinska University Hospital, Medical Unit Pelvic Cancer, Stockholm, Sweden, 4Helsingborg County Hospital, Department of Urology, Helsingborg, Sweden, 5Linköping University, Department of Clinical and Experimental Medicine, Division of Urology, Linköping, Sweden, 6Umeå University, Department of Surgical and Perioperative Sciences, Urology and Andrology, Umeå, Sweden, 7Östersund County Hospital, Department of Urology, Östersund, Sweden, 8Trondheim University Hospital, Department of Urology, Trondheim, Norway
Background: To investigate location of lymph node metastases in upper tract urothelial carcinoma situated in the renal pelvis/proximal ureter and short-term complications after radical nephroureterectomy with lymph node dissection.
Methods: Prospective Nordic multicenter study (four university hospitals, two county hospitals) 2009-2022. Patients with clinical suspicion of locally advanced upper tract urothelial carcinoma (>stage T1) and/or clinical lymph node positive (cN+) disease were invited to participate. Participants were subjected to a pre-defined and side-specific template-based fractionated retroperitoneal lymph node dissection in conjunction with radical nephroureterectomy. Location of lymph node metastases in the lymphadenectomy specimen and retroperitoneal lymph node recurrences during follow-up was recorded. Postoperative complications within 90 days of surgery were ascertained from patient charts. Descriptive statistics were applied.
Results: Lymph node metastases were present in the lymphadenectomy specimen in 23/100 patients, and 9/100 patients had a retroperitoneal recurrence. Distribution per side showed lymph node metastases in the lymphadenectomy specimen in 11/38 (29%) patients with right-sided tumors using the anatomically larger right-sided template, compared to 12/62 (19%) patients with left-sided tumors applying a more limited template. High-grade complications (Clavien grade ≥3) within 90 days of surgery were registered in 13/100 patients. The study is limited in size and not powered to assess survival estimates.
Conclusions: The suggested and prospectively applied templates for right-sided and left-sided lymphadenectomy in patients with advanced upper tract urothelial carcinoma included the majority of lymph node metastases. High-grade complications directly related to the lymphadenectomy part of the surgery were limited.
AS-2.016
Tumour ADC at a preoperative MRI is a predictor of tumour stage in upper tract urothelial carcinoma
Almås B1, Hjelle K M1,2, Reisæter L A R3, Beisland C1,2
1Haukeland University Hospital, Urology, Bergen, Norway, 2University of Bergen, Department of Clinical medicine, Bergen, Norway, 3Haukeland University Hospital, Department of Radiology, Bergen, Norway
Background: The correct preoperative staging of upper tract urothelial carcinoma (UTUC) can be challenging. Precise staging can help select patients for intensified treatment such as neo-adjuvant chemotherapy before nephroureterectomy (NU). The purpose of the present study was to investigate the predictive abilities of a preoperative MRI among patients with a verified UTUC.
Methods: Written consent was obtained from potential participants. 35 UTUC patients treated with radical surgery were examined with a preoperative MRI and prospectively included during 2017-2022. The CT scans and MRIs were assessed for radiological stage, and the apparent diffusion coefficient (ADC) in the tumours at the MRI was registered. The radiologist was blinded for final pathology. The radiological variables were analysed regarding their abilities to predict non-organ confined disease (NOCD, pT3+ or N+) and tumour grade at final pathology after NU. The predictive abilities were assessed using chi-square tests, Student’s t-test and a ROC curve. P-values <0.05 were considered statistically significant.
Results: Mean age was 72 years, 8 patients were female and 9 patients had NOCD. Radiological stage at CT or MRI did not predict NOCD in the present cohort. The ADC values in the tumours were significantly lower for patients with NOCD and high-grade tumours compared to patients with localized disease and low-grade tumours (922 vs 1166, p=0.003 and 1018 vs 1216, p= 0.009). The area under the curve for ADC to predict NOCD in a ROC curve was 0.84 (CI 0.70-0.97, p=0.003). Having an ADC <1000 predicted NOCD at final pathology with a sensitivity and specificity of 78% and 81% respectively.
Conclusions: Tumour ADC at the MRI emerges as a potential biomarker for aggressive disease. A tumour ADC value < 1000 indicates an aggressive tumour where intensified treatment can be considered. This study further underlines the difficulty in the preoperative staging of UTUC using conventional examinations.
AS-2.017
Epitranscriptomic Regulation in Bladder Cancer
Monshaugen I1,2, Su Z3, Dutta A3, Klungland A2, Ougland R1,2
1Bærum Hospital, Vestre Viken HF, Department of Surgery, Gjettum, Norway, 2Oslo University Hospital, Department of Microbiology, Oslo, Norway, 3University of Alabama, Department of Genetics, Birmingham, United States of America
Background: The transcriptional output of the human genome, the transcriptome, is indispensable for cellular functions. These transcripts are highly decorated with chemical modifications to regulate their structure and function. The discovery of a reversible nature of these modifications opened the field of “epitranscriptomics”, and aberrant epitranscriptomic regulation is a hallmark of carcinogenesis. We aim to decipher epitranscriptomic mechanisms underlying development and progression of bladder cancer to identify molecular targets for novel anti-cancer therapy. We will pinpoint normal and malignant RNA methylation pattern in small non-coding RNAs using human surgical specimens and elucidate the effect of writers, readers and erasers of these marks on the cellular phenotype in tumor-mimicking model systems.
Methods: Paired tumor and non-tumor bladder tissue specimens were obtained from patients undergoing transurethral resection of NMIBC. Short non-coding RNAs (less than 50 bp) were analyzed by genome-wide profiling using a modified protocol to quantify 1-methyladenosine abundance and positions. The human bladder cancer cell line 5637 with SV-HUC1 control cell line were used to modulate the expression of the epitranscriptomic writers and erasers TRMT6/61A, ALKBH1 and ALKBH3. Tunicamycin was used to induce the unfolded protein response (UPR) pathways.
Results: In bladder cancer, higher expression of the methyl transferase complex TRMT6/61A is accompanied by increased m1A on 22-nucleotide long 3’ fragments of tRNA (tRF-3b). This mechanism regulates UPR via the tRF-3 targets MBTPS1 and CREB3L2 in ATF6 branch of UPR. Downregulation and overexpression of TRMT6/61A, and the epitranscriptomic erasers ALKBH1 and ALKBH3 in human bladder cancer cell lines affect tumor cell proliferation through m1A on tRF-3b and UPR activity.
Conclusions: Epitranscriptomic mechanisms, specifically m1A on tRFs, regulate tumor cell behavior and may represent a molecular target for novel anti bladder cancer drugs.
AS-2.018*
Developing non-invasive and cost-effective methods for urothelial cancer detection using a urine DNA panel (UCLIB diagnostic panel)
Nikkola J1,2, Kallio H2,3, Ryyppö L2,3, Jämsä P1, Selin H2,3, Vuorinen J2,3, Kaipia A1, Pekkarinen T1, Åkerla J1, Nykter M2,3, Veitonmäki T1, Annala M2,3
1Tampere University Hospital, Department of Urology, Tampere, Finland, 2Tampere University, Faculty of Medicine and Health Technology, Tampere, Finland, 3Tampere University Hospital, Tays Cancer Centre, Tampere, Finland
Background: Detection of cancer associated DNA in plasma or urine samples (urine tumor DNA, utDNA) has been shown to have great potential in urothelial cancer detection and surveillance. As part of an ongoing study to detect residual disease after surgery, we studied the potential of utDNA for diagnostic purposes in urothelial cancers.
Methods: Urine prior to surgery and fresh frozen tumor tissue from the operation was collected from enrolled patients. We developed a hybridization capture assay targeting the coding regions of the 21 most commonly mutated genes in urothelial tumors, as well as 8 frequently copy number altered loci. Samples were sequenced using Illumina instruments. Mutations, copy number alterations, and chromosomal rearrangements were computationally identified.
Results: Pre-surgical urine samples were positive for cancer-derived DNA in 50 / 52 (96%) patients with bladder cancer (pTa low grade - pT4) and 15 / 18 (83%) patients with upper tract urothelial carcinoma (pTa low grade - pT3). Urothelial cancer associated mutations were found in 1 / 47 (2%) control urine samples from healthy volunteers and kidney cancer patients (one TERT promoter mutation in a kidney cancer patient). Median cancer fraction pre-surgery was 30% for bladder cancer and 43% for upper tract urothelial carcinoma patients. All mutations found in primary tumor tissue were also detected in urine, but urine revealed additional subclonal driver mutations in several patients. The most frequently mutated regions were the TERT promoter (90% patients), TP53 (67%), FGFR3 (35%), PIK3CA (31%), and ERBB2 (25%). We evaluated both urine cell pellet DNA and urine cell-free DNA, and found similar cancer DNA fractions in the two analytes, but higher DNA yields for urine cell pellet DNA.
Conclusions: These early results using UCLIB diagnostic panel show promise in urine DNA based cancer diagnostics even in patients with pTa low grade tumors. The panel is designed to offer a non-invasive and cost-effective alternative for cystoscopies.
*Nominee for best abstract in the field of urologic cancer
AS-2.019
To sample and molecularly classify muscle-invasive bladder cancer without fractionating the specimen: Urodrill - a novel MRI-guided endoscopic biopsy technique
Eriksson P1, Berg J2, Bernardo C1, Bobjer J3,4, Brändstedt J3,4, Löfgren A3,4, Simoulis A3,5, Sjödahl G3, Sundén F4, Wokander M4, Zackrisson S2,3, Liedberg F3,4
1Lund University, Department of Clinical Sciences, Division of Oncology, Lund, Sweden, 2Skåne University Hospital, Department of Diagnostic Radiology, Malmö, Sweden, 3Lund University, Institution of Translational Medicine, Malmö, Sweden, 4Skåne University Hospital, Department of Urology, Malmö, Sweden, 5Skåne University Hospital, Department of Pathology, Malmö, Sweden
Background: The current pathway for patients with muscle-invasive bladder cancer (MIBC) is CT-urography, cystoscopy, transurethral resection (TURB) to histologically confirm MIBC, neoadjuvant chemotherapy (NAC) and radical cystectomy (RC). The vesical imaging-reporting and data system (VI-RADS) have been suggested to identify MIBC patients with high specificity using MRI, however a recent randomized trial reported misclassification in one out of three patients. We aim to investigate a new endoscopic biopsy-device (Urodrill) to confirm MIBC and to assess molecular subtype (Lund Taxonomy) by gene expression in patients with suspicion of MIBC on MRI.
Methods: In a feasibility study, we included 10 patients with clinical suspicion of MIBC that were further investigated by MRI and categorized as VI-RADS 4 or 5. Through a flexible cystoscope, Urodrill-biopsies were directed into the muscle-invasive portion of the tumor (according to the MRI) under general anaesthesia before a conventional TURB was performed with a 26 Ch resectoscope.
Results: In 9/10 patients a Urodrill-sample could be obtained, where 6/9 verified MIBC and 7/9 contained detrusor. In 7/8 patients where the Urodrill-biopsy was subjected to RNA-sequencing, molecular subtype could be determined. No complications related to the biopsy device occurred in the ten patients.
Conclusions: A randomized trial comparing this new diagnostic pathway for patients with clinical suspicion of MIBC with the current standard TURB is suggested.
AS-2.020
Potential pathological advantages of En Bloc-resection of non-muscle invasive bladder tumours – a multicentre randomised trial
Nielsen N K1, Milling R V1, Vásquez J L2, Fabrin K3, Haug E S4, Olsen K Ø5, Geertsen L6, Rudlang T M7, Sepp T8, Kovtun M9, Zarkovski M10, Vjaters E11, Juodelis G12, Kingo P S1, Jakobsen J K1, Lam G W7, Jensen J B1
1Aarhus University Hospital, Dept. of Urology, Aarhus N, Denmark, 2Zealand University Hospital, Dept. of Urology, Roskilde, Denmark, 3Aalborg University Hospital, Dept. of Urology, Aalborg, Denmark, 4Vestfold Hospital Trust, Dept. of Urology, Tønsberg, Norway, 5Gødstrup Regional Hospital, Dept. of Urology, Gødstrup, Denmark, 6Odense University Hospital, Dept. of Urology, Odense, Denmark, 7Herlev and Gentofte Hospital, Dept. of Urology, Herlev, Denmark, 8North Estonia Medical Centre, General and Oncology Urology Centre, Tallinn, Estonia, 9East Tallinn Central Hospital, Centre of Urology, Tallinn, Estonia, 10Tartu University Hospital, Department of Urology and Kidney Transplant, Tartu, Estonia, 11Paula Stradina Clinical University Hospital, Urological Center, Riga, Latvia, 12Hospital of Lithuanian University of Health Sciences, Dept. of Urology, Kaunas, Lithuania
Background: En Bloc-resection (EBR) of non-muscle invasive bladder cancer (NMIBC) can potentially overcome the flaws of conventional transurethral resection of bladder tumours (cTURB), particularly regarding pathological quality of the specimen.The aim of this study is to evaluate the pathological advantages of EBR compared with cTURB of NMIBC in terms of complete tumour removal, pathological quality, and correct staging.
Methods: The study is a multicentre randomised controlled trial. Patients with suspected NMIBC tumours ≥1cm and ≤6cm are randomised to either EBR or cTURB. We will include 220 patients, 110 in each group. A central pathology revision will be performed of all specimens, and the primary endpoint will be proportion of patients with unaltered T-stage following pathology revision and second resection (reTURB), compared with the initial pathology assessment. Data include tumour features (size, location), surgical features (instrument for resection and extraction, operative time), pathological features (primarily: T-stage, grade, presence of detrusor muscle (DM), and at revision: ability to assess resection margins, presence of tissue fragments with no epithelium or DM, rate of thermal damage), residual tumour at re-TURB, progression and recurrence free survival, and patient reported outcome.
Results: As of March 13th, 2023, 60 patients are included from 6 sites, 6 sites are pending. 34 EBRs have been performed, 24 (70.6%) successfully, 7 were converted to piecemeal resection. Median tumour size is 2.30cm (IQR: 1.50;3.20) in the EBR group, 2.25cm (IQR: 1.50;2.85) in the TURB group. Median operative time is 30min (IQR: 25;61) for EBR, 28min (IQR: 18;44) for cTURB. Final results regarding primary endpoint are expected in 2024.
Conclusions: This study can evaluate the ability of EBR to remove NMIBC tumours with better pathological quality and certainty compared with cTURB. Positive results could potentially redefine guidelines on golden standard for preferred resection technique in future NMIBC patients.
AS-2.021
Bladder Cancer: Correlation between immune response and side effects in BCG treated patients
Hartmann K D1, Munk L1, Strandgaard T2, Dyrskjøt L2, Jensen J B1
1Institut for Clinical Medicine, Department of Urology, Aarhus University Hospital, Aarhus, Denmark, 2Institut for Clinical Medicine, Department of Molecular Medicine, Aarhus University Hospital, Aarhus, Denmark
Background: High risk non-muscle invasive bladder cancer (NMIBC) is recommended to receive adjuvant intravesical instillations with Bacillus Calmette-Guerin (BCG) to reduce the risk of recurrence and progression. Up to 70% of the patients report side effects (SE) from BCG treatment and 15-20% of patients end treatment due to SE. Moreover, 30-40% of patients do not respond to BCG treatment. Theoretically, SE might be correlated to increased response and thereby a good prognosis. Aim: To evaluate the correlation between immune response and inflammation with regards to SE and treatment outcome in patients diagnosed with NMIBC receiving BCG treatment.
Methods: Patients with NMIBC treated with at least five cycles of BCG were retrospectively chosen from a large biobank. Tumor samples were collected before and after BCG treatment. Tumors were analyzed using RNA sequencing and whole-exome sequencing. Information regarding SE after each BCG treatment and treatment response are collected retrospectively from patient records. Treatment response is based on registered tumor recurrence, progression, and survival. Data on immune response will be correlated to the data on SE and treatment response.
Results: 156 patients with BCG-treated NMIBC were included in this study. 123 (79%) of the patients were men and median age of patients were 71 years (IQR 62-76 years). A previous study on the cohort showed that post-BCG high grade recurrence was associated with post-BCG CD8 T-cell exhaustion (p=0.002). Pre-BCG tumors from patients with post-BCG T-cell exhaustion had high expression of genes related to cell-division and immune function. Results regarding SE correlated to these molecular immune function markers are pending and will be presented.
Conclusions: CD8 T-cell exhaustion and change in immune function may be a key factor in post-BCG high grade recurrence. Whether it is correlated to clinical SE will be investigated. If correlated, BCG treatment could potentially be targeted to each patient based on SE to improve the effect.
AS-2.022
The association between BCG treatment in patients with bladder cancer and subsequent risk of developing Alzheimer and other dementia - A Swedish nationwide cohort study from 1997 to 2019
Wang E Y1, Hagberg O2, Malmström P-U3
1Center for Clinical Research, Region Sörmland, Dept of Surgical Sciences, Urology, Uppsala University, Eskilstuna, Sweden, 2Department of Translational Medicine, Lund University, Malmö, Sweden, 3Department of Surgical Sciences, Urology, Uppsala University, Uppsala, Sweden
Background: Alzheimer´s disease (AD) affects 50 million people worldwide. The immune system plays an important role in the pathogenesis of AD. Several retrospective analyses have reported a substantial decreased risk of AD and other dementia in bladder cancer patients treated with immunotherapy using BCG bladder instillations. These studies have used other bladder cancer patients as controls.
Methods: We utilized the database BladderBaSe 2.0 containing tumor-specific, health-related and socio-demographic information for patients with non-muscle invasive bladder cancer (NMIBC) diagnosed between 1997 and 2019. It also contains a matched comparison cohort sampled from the background population with individuals free from cancer in the urinary tract at the time of diagnosis of the index case. Five controls for each index case were randomly selected. Inclusion criteria to identify the participants in this study were the patients who have been diagnosed with a NMIBC and having BCG as primary treatment. The outcome of interest was the subsequent diagnosis of AD or other dementia.
Results: We identified 38,934 patients with NMIBC and of these 6,496 received BCG. AD/Dementia was diagnosed in 6.1% of cases and 7.4% in controls. The cases had overall marginally lower risk of dementia than controls. The risk reduction with high age and female gender were more significant. The associations were similar for AD specifically but not significant. The multivariate Cox analysis showed that BCG treated had a lower risk of dementia than those who did not receive BCG but also bladder cancer patients irrespective of treatment had a decreased risk compared to healthy controls.
Conclusions: In this study, we observed in contrast to previous reports only a marginally decreased risk of developing AD/Dementia correlated to earlier intravesical BCG treatment in patients with NMIBC, and this small benefit mostly affected those with high age and female gender. Bladder cancer patients in general had a lower risk for the disease.
SESSION III - ORAL PRESENTATIONS – MISCELLANEOUS
AS-3.023
Updated findings on biopsies in men with testicular microlithiasis and associated risk factors: Time to refine clinical practice?
Frandsen R H1, Durukan E1, von Rohden E1, Jensen C F S1, Azawi N2, Fode M1
1Copenhagen University Hospital, Herlev and Gentofte Hospital, Department of Urology, Herlev, Denmark, 2Zealand University Hospital, Roskilde, Department of Urology, Roskilde, Denmark
Background: Testicular microlithiasis (TM) has been associated with a risk of germ cell neoplasia in situ (GCNIS) when combined with testicular atrophy, infertility, or cryptorchidism. Men with TM and these risk factors are offered bilateral testicular biopsies, while those with unknown fertility status may have semen samples and biopsies if semen quality is low. We aimed to determine the incidence of GCNIS in men with TM and additional risk factors.
Methods: We conducted a retrospective multicenter chart review of patients with TM who underwent biopsies between 2007 and 2021 in eastern Denmark. We recorded age, laterality of TM, additional GCNIS risk factors, biopsy-related complications, and histological findings. The primary outcome was histological findings grouped according to risk factors.
Results: 169 patients with median age of 33 (range 11-61) underwent biopsies. Risk factors included atrophy (n=12), infertility (n=9), low semen quality (n=33), cryptorchidism (n=24), and combinations of these (n=73); 18 had no risk factors. Minor complications occurred in 23 patients (13.6%). GCNIS was found in 13 patients (7.7%); 3 with atrophy, 2 with low semen quality, and 8 with a combination of atrophy and other risk factors. Risk of GCNIS was 15.9% with atrophy.
Unilateral TM was present in 8 GCNIS positive patients, with GCNIS only on the ipsilateral side. Among 5 with bilateral TM, GCNIS was found on both sides in 1 patient. Patients with unilateral GCNIS underwent orchidectomy, and 7/12 specimens showed pT1 seminoma. The patient with bilateral GCNIS had radiation therapy.
Conclusions: Testicular biopsies remain relevant in the presence of TM combined with testicular atrophy and/or reduced semen quality. Meanwhile, a history of cryptorchidism or infertility without a documented male factor does not seem to infer an increased risk of testicular pathology and biopsies may be omitted in such men. Biopsies may be restricted to testicles harbouring TM.
AS-3.024*
Human papillomavirus (HPV) does not modify the prognostic significance of tumour stage and grade of differentiation in penile carcinoma. A retrospective study spanning 50 years from a tertiary centre
Moen C A1, Nordanger I M1, Thorkelsen T K1, Rio O E2, Honoré A1, Chaudhry A A1, Juliebø-Jones P1,3, Bostad L3,4, Beisland C1,3
1Haukeland University Hospital, Department of Urology, Bergen, Norway, 2Haukeland University Hospital, Section for Cancer Genomics, Department of Laboratory Medicine and Pathology, Bergen, Norway, 3University of Bergen, Department of Clinical Medicine, Bergen, Norway, 4Haukeland University Hospital, Department of Pathology, Bergen, Norway
Background: Human papillomavirus (HPV) infection is a known risk factor for development of penile cancer. In histopathological studies, HPV-related carcinomas are described as more aggressive looking tumours, being associated with histologic high-grade tumour differentiation. We examined whether the HPV can modify the effect of known prognostic factors in penile squamous cell carcinomas (PSCC).
Methods: In this ethically approved study, the local diagnostic biobank was screened for stored tissue samples from patients previously operated for invasive penile cancer at our institution. HPV polymerase chain reaction (PCR) test and subsequent sanger sequencing was performed on eligible samples. HPV status was determined for 200 patients who underwent operative surgery between 1973 - 2022. All histopathological examinations were re-evaluated by a pathologist according to the 2016 UICC TNM classification for penile cancer. Patient journals were analysed for clinical variables and disease course. Investigation of the possible interaction between HPV and histopathological variables for 5-year cancer-specific survival (CSS) was performed by Cox regression.
Results: There was no significant difference in T-stage distribution between HPV positive (n=89) and HPV negative (n=111) patients (p=0.4). Significantly more grade 3 tumors were present in the HPV positive group (p<0.001). Kaplan-Meier plots revealed a natural progressively worse survival for T1-T4 stage (log-rank test p<0.001) and grade 1-3 (log-rank test p=0.06). Similar Kaplan-Meier plots were produced when stratified by HPV status. Furthermore, there was no statistically significant interaction term between HPV status and T-stage (p=0.88) nor between HPV status and grade (p=0.64).
Conclusions: This study suggests that the prognostic significance of the conventional staging system (T-stage and grade of differentiation) does not depend on, and is not modified by, HPV status.
* Winner of the Second prize for best abstract in the field of Urologic cancer
AS-3.025
Scheduled stimulation as penile rehabilitation following radical prostatectomy: Identifying the optimal stimulation parameters in transcutaneous mechanical nerve stimulation (TMNS)
Fode M, Nolsøe A B, Durukan E, Oestergren P B, Jensen C F S, Sønksen J
Copenhagen University Hospital, Herlev and Gentofte Hospital, Department of Urology, Herlev, Denmark
Background: Erectile dysfunction (ED) occurs after radical prostatectomy (RP) due to affection of the cavernous nerves. We previously explored transcutaneous mechanical nerve stimulation (TMNS) as a method to improve nerve recovery with promising results. The objective of this study was to determine the optimal settings for TMNS to improve outcomes further.
Methods: Men without preoperative ED set to undergo nerve-sparing RP were instructed in the use of the Ferticare vibrator and given a device to take home. All men were offered PDE5-inhibitors after normal standard of care. Following surgery, they were asked to use the device daily for 6 months and to adjust the settings according to personal preferences. The men kept a diary of: 1) time spent with TMNS, 2) if an erection was achieved, 3) the settings that gave the best erections, 4) If an orgasm was achieved, 5) the setting that gave the best orgasms. The main outcome was a composite endpoint including time spent and amplitude/frequency of the device, which gave most men an erection.
Results: 19 men were included. All men used TMNS and 17 reported to be satisfied with the stimulation. On average it was performed on 41% of days. Erections with use were experienced by 15 and orgasms were experienced by 16 men. TMNS was most often performed for 5 (range 1 – 26) min at a time. The most frequently reported amplitude and frequency resulting in erections were 1 mm and 90 Hz respectively. For orgasms, amplitudes of 1 and 2 mm were equally reported, while the most common frequency was 90 Hz. At follow-up, 12/19 men were able to have penetrative sex with the help of a PDE5-inhibitor.
Conclusions: TMNS was well accepted and in combination with a PDE5-I it induced erections in most men. The optimal stimulation parameters were at least 5 min of stimulation at an amplitude of 1 mm and a frequency of 90 Hz. A randomized controlled trial is being planned to investigate the effect on erectile function recovery following RP.
AS-3.026, AS-9.098
Urinary tract symptoms and bother among middle-aged women with long lasting type 1 diabetes
Stenzelius K1, Wangel A-M2
1Lund University, Urology, Malmö, Sweden, 2Malmö University, Care Sciences, Malmö, Sweden
Background: Women with type 1 diabetes develop neuropathic and micro vessel angiopathy but does this impact the prevalence and level of bother of urinary tract symptoms among middle-aged women with long-lasting type 1 diabetes?
Methods: A cross-sectional study using a self-reporting questionnaire including validated instruments and background questions was addressed to women aged 45-66 years with type 1 diabetes for at least 15 years. Lower urinary tract symptoms were measured by ICIQ-LUTS. The Patient Health Questionnaire – PHQ-9 was used for depressive symptoms. Social status, education, length, weight, smoking, and current medication complemented the formal instruments. Descriptive statistical analysis of background factors, self-reported occurrence of lower urinary tract symptoms and depression was used. Mean values, standard deviations and frequencies were calculated for nominal data, and median and range for categorical data. The Regional Ethics and Research Board approved the study.
Results: Totally 212 women answered the questionnaire, mean age: 54 years. Mean years of diabetes was 36 years, BMI mean at 26 but 23% had BMI ≥ 30. History of gynaecological or urological surgery was reported by 37% and Caesarean section by 26%. The table present prevalence of urinary tract symptoms. Totally 22.6 experienced UTI during the last year and 40% reported mild to severe depression.
Conclusions: Women having type 1 diabetes for more than15 years reported much higher prevalence of urinary tract symptoms comparing with other studies of the same age group. Furthermore, they had high levels of bother and depressive symptoms. Therefore, special attention is needed for these women.
AS-3.027
Metabolic syndrome is not a predictor of severity of lower urinary tract symptoms (LUTS) and need for surgery in LUTS patients
Hopland-Nechita F V1,2, Andersen J R3, Beisland C2,4
1Førde Central Hospital, Surgical Department, Førde, Norway, 2University of Bergen, Department of Clinical Medicine, Bergen, Norway, 3Western Norway University of Applied Sciences, Førde, Norway, 4Haukeland University Hospital, Department of Urology, Bergen, Norway
Background: The present EAU guidelines states that there is an association between lower urinary tract symptoms (LUTS) and metabolic syndrome. Specifically, there is a positive relationship between lack of physical activity, obesity, BMI, and other measures of the metabolic syndrome with both LUTS and BPH (including prostate volume). However, increased physical activity appears to have a protective effect.
The aim of the study was to explore this alleged association between the metabolic syndrome and LUTS severity and need for surgical treatment.
Methods: This is a prospective cohort study following strict inclusion and exclusion criteria. The international prostatic symptom score (IPSS) and IPSS “bother question” (IPSS-BQ) were collected at baseline, together with data on prostate volume (PV), uroflowmetry, PSA, post-voiding residual (PVR) urine, blood samples and medical history. Metabolic syndrome is defined according to NCEP:ATPIII criteria as having at least three of five factors: abdominal obesity, high blood pressure, impaired fasting glucose, high triglyceride levels, and low HDL-cholesterol levels. The follow-up and the surgical indication were both set according to standard of care by EAU guidelines.
Results: We included 63 eligible patients of which 22 underwent surgery during follow-up and 20 controls. The median follow up was 42 months (IQR 30-50). Twenty-one patients had three or more components of the metabolic syndrome. There were no statistically significant differences concerning IPSS (P=0.39), IPSS-BQ (p=0.38), PV (p=0.5), Qmax (p=0.2) or PVR (p=0.4) between the patients with metabolic syndrome and those without. In logistic regression analysis the presence of metabolic syndrome did not predict the need for surgery (OR 0.46 (95%CI: 0.14 – 1.49) p=0.2)
Conclusions: No associations between metabolic syndrome parameters and LUTS severity, prostate volume, Q max or PVR were identified. Furthermore, the presence of metabolic syndrome did not predict the need for surgery.
AS-3.028
Adverse events associated with Urolift: Findings from the US MAUDE registry
Juliebø-Jones P1,2, Nøss Haugland J1, Tzelves L3, Arvei Moen C1, Honoré A1, Somani B4, Beisland C1
1Haukeland University Hospital, Department of Urology, Bergen, Norway, 2EAU YAU Endourology Working Group, Amsterdam, The Netherlands, 3Sismanoglio Hospital, Medical School, National and Kapodistrian University of Athens, Urology, Athens, Greece, 4University Hospital Southampton NHS Foundation Trust, Urology, Southampton, United Kingdom
Background: Urolift is an established intervention for symptoms of bladder outflow obstruction caused by benign prostate enlargement. Reported advantages include its minimally invasive profile, short learning curve and feasibility as a day case procedure. Our aim was to use a national registry as a means to evaluate the nature of complications and device failures that have been documented to occur.
Methods: Retrospective analysis was performed of the US Manufacturer and User Facility Device Experience (MAUDE) database, a prospective register, which contains voluntarily submitted adverse events associated with surgical devices. Information collected include event timing, underlying cause, procedural completion, complications, and mortality status.
Results: Between 2016-2023, 237 adverse events were identified, which occurred during the intra-operative (n= 108) and post operative (n= 129) periods. 43% of the events involved technical problems with the urolift instrument and the majority of these (89%) were due to device failure such as misfire and needle fracture. 140 post operative complications were recorded including haematuria (n=60), sepsis (n=25) and pelvic haematoma (n=10). Other complications included pulmonary embolism (n=3), stroke (n=2) and necrotising fasciitis (n=1). 46 patients required an emergency reoperation and a further 15 patients required embolization in the early post operative period to achieve bleeding control. In total, 5% of the events resulted in an admission to intensive care. 11 post operative deaths were recorded across the study period.
Conclusions: While urolift is recognised as a less invasive intervention compared to alternatives such as transurethral resection of the prostate, serious adverse events have been reported to occur including death. Our findings can provide learning points for surgeons and allow for improved patient counselling and treatment planning accordingly.
AS-3.029
Preliminary results indicate lower perioperative morbidity of robotic assisted simple prostatectomy compared to open simple prostatectomy - a single institution report
Aarsæther E1, Larsen M1, Gullan D2, Roaldsen M1
1University Hospital of North Norway, Department of Urology, Tromsø, Norway, 2Stavanger University Hospital, Department of Urology, Stavanger, Norway
Background: According to the guidelines of the European Association of Urology, open simple prostatectomy should be offered to men with a prostate size exceeding 80 mL suffering from moderate to severe LUTS in the absence of a transurethral enucleation technique.
However, open simple prostatectomy is associated with complications such as bleeding, blood transfusions and increased length of stay compared to minimally invasive procedures. The aim of the study was to compare perioperative data from the first eight robotic assisted simple prostatectomy (RASP) cases to that of patients subjected to open simple prostatectomy (OSP) at our department.
Methods: The patients were identified by a search for the NOMESKO procedure codes for either OSP (KED96) or RASP (KED01). All patients had a history of moderate to severe LUTS and a preoperative prostate volume exceeding 80 mL. In the OSP group enucleation of the adenoma was performed through the prostatic capsule (Millin procedure), while access to the adenoma was gained through the bladder in the RASP group. Complications were scored according to the Clavien-Dindo classification system.
Results: 27 patients who underwent OSP were retrospectively identified and compared to the first eight who were subjected to RASP. The groups were similar with respect to age, body mass index and ASA score. Operative time was significantly shorter in the OSP group compared to the RASP group. Bleeding volume, drop in postoperative hemoglobin and the number of blood transfusions were all significantly higher in the OSP group compared to the RASP group. Average length of stay was 5.5 (2-18) days in the OSP group compared to 1.5 (1-3) days in the RASP group (p<0.001). The number of postoperative complications, Clavien-Dindo>/=2, were significantly higher in the OSP group (11) compared to the RASP group (none, p<0.05).
Conclusions: The introduction of robotic assisted simple prostatectomy significantly reduced perioperative morbidity at our department.
AS-3.030
Can artificial intelligence (AI) improve the management of men with LUTS?
Malmström P-U1, Lauer J K2, Nilsson M3, Hemdan T4
1Uppsala University, Surgical sciences, Uppsala, Sweden, 2Oxelösunds vårdcentral,, Primary care, Oxelösund, Sweden, 3Research Institutes of Sweden, Computing, Kista, Sweden, 4Enköpings sjukhus, Urology, Enköping, Sweden
Background: In a Swedish study of men 40-80 years the overall prevalence of the lower urinary tract symptoms (LUTS) was 24%. The number who sought health care of these was only 4%. In a Danish survey with men aged 20+ the prevalence was almost identical and despite the high prevalence of bothersome LUTS more than one-fifth of men did not discuss their symptoms with either personal nor professional relations. The problems are expected to increase due to an aging population.
AI is being utilized in radiology and pathology but for primary care this seems to be missing.
Our aim is to create an IT solution that provides support and individual advice to men with LUTS in a user-friendly mobile app solution. Secondly to improve the diagnostic quality in primary healthcare with a decision support for GPs
Methods: A virtual patient database was constructed containing age, BMI, other diseases, medication, and patient reported IPSS, urinary diaries and timed assessed micturition. Also the urologists diagnosis based on these variables. This data was analyzed with machine learning models and Bayesian methods with the goal to develop optimal algorithms for individualized recommendations. A prospective clinical study started 2021 after ethical approval with the intent to collect information from men seeking a GP for LUTS. The corresponding database will be used to validate the first version of the AI program.
Results: The first version of the AI program reached the same diagnosis as an urologist in 90 % of tested patients. Inclusion of patients have started at three primary care centers and in a urology clinic. Validation of this database is planned later this year when inclusion of 150 patients have been completed.
Conclusions: Improvement in health care for men with LUTS is urgent. AI based solutions for diagnosis and individualized recommendations is one promising alternative avenue.
AS-3.031*
Treated Urolithiasis in Pediatric Patients at Akershus University Hospital 2014-2023: a single center study of incidence, clinical presentation, treatment and outcomes
Hannestad I, Helgø D, Müller S
Akershus University Hospital, Urology, Nordbyhagen, Norway
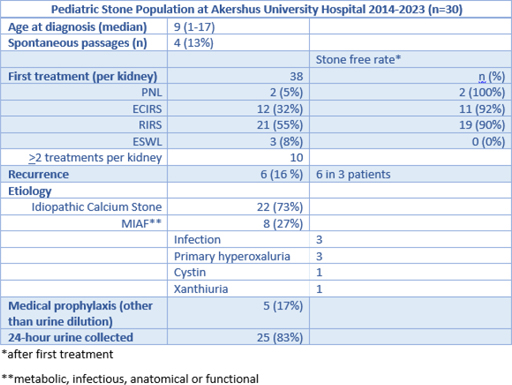
Background: Urolithiasis in children is rare. They are considered a high-risk group of recurrence and follow up investigation is mandatory. The outcome of this study was to determine the pediatric patients treated for urolithiasis at Akershus University Hospital, and define treatment modalities, stone-free rate (SFR) and results of follow-up investigation.
Methods: We performed a single-center retrospective cohort study with prospectively collected data from the urolithiasis database at Akershus University Hospital. It included patients <18 years at time of treatment from 01.01.14 to 01.01.23 at our hospital. From our electronical medical records, we retrieved demographic data (age, gender and ethnicity) and treatment data. Furthermore, recurrence rate, stone-etiology and medical prophylaxis implemented was documented, including follow-up investigation.
Results: 30 children with urolithiasis were identified. Some patients had bilateral stone burden and some had recurrent stones after successful primary treatment. The end-point of all treatments was stone freeness.
Conclusions: The incidence of urolithiasis of the pediatric population at our hospital is low. Only 1.8% of our urolithiasis population is pediatric. Nevertheless, we aim to analyse all stones and complete a 24-hour urine collection after primary stone treatment. All patients with idiopathic calcium stone were recommended urine dilution as primary prophylaxis. In addition, all patients were offered follow-up sessions deciding further prophylaxis in early age to prohibit future stone burden. Five out of eight patients with rare MIAF-stone were started on medical prophylaxis, which highlights the importance of metabolic diagnostics in pediatric stone patients.
*Winner of the Third prize for best abstract in the field of benign Urology
AS-3.032
A novel method for temperature measurements during ureteroscopic laser lithotripsy in patients with indwelling nephrostomy tubes
Æsøy M S1,2, Juliebø-Jones P1,2, Gjengstø P1, Beisland C1,2, Ulvik Ø1,2
1Haukeland University Hospital, Department of Urology, Bergen, Norway, 2University of Bergen, Department of Clinical Medicine, Bergen, Norway
Background: While there are several factors influencing the rise and fall of temperatures during ureteroscopy (URS), the intricacies surrounding them remain in question. We have previously measured temperature profiles in the renal pelvis (RP) during URS in an ex-vivo porcine model using a temperature sensor through a nephrostomy tube (NT). The aim of this study was to evaluate the feasibility of using this method in a clinical setting.
Methods: A 42-year-old woman with a 6mm proximal stone in the left ureter and an indwelling NT was planned for URS lithotripsy with simultaneous temperature measurements. The URS was performed under general anesthesia and with antibiotic prophylaxis. No access sheath was used. Irrigation was gravitational at 60 cmH2O and fluid temperature at 21°C. The stone was moved to the upper calyx for lithotripsy. A temperature sensor was inserted through the NT and positioned in the lower calyx. Thulium Fiber Laser (150μm fiber) was activated at settings of 5W, 10W, 20W and 30W. For each power setting, temperatures were recorded during laser activation for 120 seconds (s), and for another 60s after deactivation. Temperatures of 43°C resulted in immediate deactivation of the laser and measurements were continued for a total of 180s.
Results: Baseline temperatures in the RP varied from 31.8-32.8 °C. Activating the laser resulted in an immediate rise in temperatures for every power setting. Higher power produced higher temperatures. The threshold for thermal injuries (43oC) was not reached when applying either 5W or 10W. However, this threshold was met after 28s and 12.5s when applying 20W and 30W, respectively. After deactivation, temperatures remained above 43°C for more than 15s. The calculated thermal dose (CEM43) was 63s. No complications were reported.
Conclusions: This study demonstrates the feasibility of temperature measurements during URS in patients with indwelling nephrostomy tubes. Our results suggests that high laser power application may result in harmful temperatures.
AS-3.033
Expanding the horizons of endourology: Ureteroscopy outside the urinary tract
Vo A K1, Aesøy M S1, Juliebø-Jones P1,2, Ulvik O1,2
1Haukeland University Hospital, Department of Urology, Bergen, Norway, 2University of Bergen, Department of Clinical Medicine, Bergen, Norway
Background: Technological advancements in the field of endourology has allowed for novel applications to be developed. This includes application in the setting of pancreaticobiliary disease. Our aim was to report our experiences with this technique.
Methods: Retrospective review was performed of patients undergoing gastrointestinal surgery with the assistance of an endourologist between 2020-2023. All procedures including flexible ureteroscopy were registered. Outcomes of interest included technical success in terms of procedural completion and stone free status.
Results: In total, 9 cases were identified. There were two men and seven women with a mean age of 61.6 years (range 32-82). All cases were procedures for pancreaticobiliary conditions. All of these had conditions where conventional ERCP was not feasible due to the limitations of the equipment or due to altered intra-abdominal anatomy after previous gastrointestinal surgery. The endoscopic surgery performed can be categorized into five different procedures: 1) Percutaneous transhepatic recanalization between the common bile duct and duodenum using Thulium fiber laser. 2) Endoscopic laser lithotripsy in the right hepatic duct using a laparoscopic approach via choledochotomy. 3) Percutaneous transhepatic destruction of biliary intra-ductal tumor(s) using Thulium fiber laser. 4) Combined laparoscopic cholecystectomy and endoscopic stone extraction from the common bile duct. 5) Open access abdominal surgery with endoscopic laser disintegration of stone(s) in the pancreatic duct. All patients were treated successfully. Patients with stone burdens achieved endoscopic stone free status.
Conclusions: Combining gastrointestinal surgery with tailored application of flexible ureteroscopes has the potential to save patients from major open and complex surgery. In all 5 of these clinical scenarios, ureteroscopic intervention provides a feasible alternative to more invasive approaches.
SESSION IV - POSTER PRESENTATIONS – KIDNEY
AS-4.034
The use of Renal Mass Biopsies (RMB) has increased at Haukeland University Hospital (HUH) during 2008-2022
Hjelle K M1, Almås B1, Esoy M S2, Beisland C1, Chaudhry A C3
1Haukeland University Hospital, Department of Urology, Bergen, Norway, 2Haukeland University Hospital, Departement of Urology, Bergen, Norway, 3Haukeland University Hospital, Departemnt of Urology, Bergen, Norway
Background: Life expectancy is increasing, as is the number of small renal masses detected incidentally. RMB is recommended to personalize treatment (surveillance, ablation or surgery), The aim of this study is to evaluate aspects of our RMB policy over the last 15 years.
Methods: Patients who underwent RMB at HUH between 2008 and 2022 are included. Data from these 398 patients and 463 biopsies were retrieved from the medical records and presented as median (IQR) or n (%).
Results: The RMB was performed due to primary kidney tumor (PKT) in 279 patients and as a part of a metastatic work-up in 119. As expected, patients with PKT were older than the metastatic patients. Moreover, PKTs were smaller, 3.2cm (2.3-5.0) vs 8.0cm (4.5 -10.5). An increasing number of patients with PKT had RMB, illustrated with 23, 93 and 163 in first, second and third period, respectively. An increased use was also seen in metastatic patients, as 34, 28 and 57 had RBx in the beforementioned periods. For PKT there was a trend towards smaller tumours the latter years. No difference in gender, laterality, ASA or core-length was found. Overall, representative RMB was achieved in 85,1% (394/463) including both primary biopsies and re-biopsies. Only eight patients had registered complications including readmittance due to haematuria or hematomas.
Conclusions: The use of RMB at HUH has increased for both patients with PKT and patient with metastatic disease. As the procedure is performed with few complications and a satisfactory diagnostic yield, it strengthen its role as a valuable and needed tool for clinicians.
AS-4.035
Safety of CT-guided Percutaneous Cryoablation for Renal Cell Carcinoma Stage cT1 in Patients with the Need for a Pre-procedural Double-J stent: An International Multicenter Study
Junker T1,2, Rønnegaard A1, Aarup Duus L1, Lund L2,3, Tivell L4, Hemmert Olesen T5, Acosta Ruiz V4, Dahlman P4, Lönnemark M4, Magnusson A4, Graumann O1,2
1Odense University Hospital, Research and Innovation Unit of Radiology, Odense, Denmark, 2University of Southern Denmark, Department of Clinical Research, Odense, Denmark, 3Odense University Hospital, Department of Urology, Odense C, Denmark, 4Uppsala University, Department of Surgical Sciences - Radiology, Uppsala, Sweden, 5Odense University Hospital, Department of Radiology, Odense, Denmark
Background: Percutaneous cryoablation (PCA) is a minimally invasive procedure reported to have lower rates of complications than partial nephrectomy when treating renal cell carcinoma (RCC). During PCA, a double-J stent can be indicated when the tumor is located close to the ureteropelvic junction, the ureter, or the renal collecting system. However, a double-J stent can cause complications like upper urinary tract infections and intraabdominal abscesses. This study aimed to assess the safety of CT-guided PCA in patients treated for cT1 RCC who had pre-procedural a double-J stent.
Methods: Patients treated between January 2016 to February 2021 at Odense University Hospital, Denmark or Uppsala University Hospital, Sweden, were included in this retrospective cohort study. Treatment decision was based on a multidisciplinary team conference. Relevant cases were identified from local databases. Patients over the age of 18 years with biopsy-verified RCC or suspected malignity were included. All patients had a double-J stent inserted in general anesthesia prior to PCA. Complications were recorded within 30 days and graded according to the Clavien-Dindo classification. Major complications were defined as complications ≥grade 3.
Results: The cohort included 61 patients with a median of age 66 (IQR, year, 55-75). The median tumor size was 33 mm (IQR 24-38), with a median RENAL score of 8 (IQR 7-10). In addition, 56% of patients received prophylactic antibiotics. A complication rate of 36% (n=22) was recorded, and major complications occurred following 10% (n=6) of the procedures. A statistically significant association was found between the number of cryoprobes used during the ablation and complications (OR, 4.45; 95% CI, 1.46-13.57; P=0.009). In addition, no other significant associations were found.
Conclusions: This study found that patients with a double-J stent in connection with PCA have a high risk of complications. However, more extensive studies, preferably with prospectively study designs, are needed.
AS-4.036
Impact of renal function on the treatment decision for surgical treatment type in patients with renal cell carcinoma
Kröger Dahlin B-I, Hlodan J, Ljungberg B
Umea University, Department of Surgical and Perioperative sciences, Urology and Andrology,, Umeå, Sweden
Background: The prognosis for patients with synchronous metastatic renal cell carcinoma (mRCC) remains poor. Despite improvements with single agent tyrosine kinase inhibition (TKI) and additionally clinical gains by immune checkpoint inhibitor (ICI) combinations, the treatment effects remain deficient.
Methods: Patients treated with surgery at the department of urology, Umeå University Hospital between 1994 and 2018 were included, while patients with other treatments were excluded. There were 667 patients with renal cell carcinoma in all stages, 265 women and 402 men, with mean age of 66 years. Data were extracted on renal function using estimated glomerular filtration rate (eGFR), WHO performance status (WHO-PS), Charlson comorbidity index (CCI), surgical type, clinical T-stage, tumor type, tumor size and survival status. Statistical analysis included: Mann-Whitney U and X2 tests and logistic regression analysis.
Results: Of 667 patients, 458 were treated with RN and 209 with PN. 545 patients (82%) had clear cell, 90 (14%) papillary, 24 (4%) chromophobe RCC, while 8 (1%) had other RCC types. In all patients preoperative eGFR in PN, was 80,6 significantly higher than eGFR in patients treated with RN (77,2, p=0.022). Using a logistic regression model CCI (RR 2.39 95%Ci 0.01-0.11), WHO-PS (RR 4.20 95%Ci 0.41-0.11), T-stage (RR 16.49 95 % Ci 0.13 – 0.18) associated significantly with treatment selection, while eGFR, RCC type, age and gender did not. In the subgroup analysis of cTa (≤4cm) RCCs, eGFR in contrast, was significantly higher in patients treated with PN (84.7) than in those treated with RN (75.9, p=0.012). Using a logistic regression model only WHO-PS (RR 4.08 95%Ci 0.09-0.28) associated with treatment selection while eGFR, CCI, RCC type, age and gender were not.
Conclusions: Several clinical variables associated to the clinical treatment decisions in patients with RCC. Renal function as assessed with eGFR seemed not to have a major impact on the treatment strategy in patients with renal cell carcinoma.
AS-4.037
Renal functional outcomes after robot-assisted partial nephrectomy and percutaneous cryoablation of clinical T1 renal cell carcinoma – a prospective study
Junker T1,2, Duus L1,3, Rasmussen B1,4, Vilstrup M H5, Lund L2,6, Pedersen M1,7, Graumann O1,4
1University of Southern Denmark, Research and Innovation Unit of Radiology, Odense C, Denmark, 2Odense University Hospital, Department of Urology, Odense C, Denmark, 3Odense University Hospital, Odense Patient data Explorative Network, Odense C, Denmark, 4Odense University Hospital, Department of Radiology, Odense C, Denmark, 5Odense University Hospital, Department of Nuclear Medicine, Odense C, Denmark, 6University of Southern Denmark, Institute of Clinical Research, Odense C, Denmark, 7Aarhus University, Comparative Medicine Lab, Aarhus, Denmark
Background: Treatment of elderly patients with renal cell carcinoma (RCC) is challenging due to comorbidities, including renal functional impairment. Partial nephrectomy (PN) and thermal ablation (TA) are recommended to minimize the risk of development or progression of chronic kidney disease (CKD).
Our aim was to investigate renal function after robot-assisted PN (RAPN) and percutaneous cryoablation (PCA) in clinical stage T1 (cT1) RCC and evaluate the relationship between baseline renal function and renal functional outcome.
Methods: Patients with cT1 RCC treated with RAPN or PCA between June 2019 and January 2021 were prospectively and consecutively enrolled after a multidisciplinary team (MDT) cenference. Renal function was evaluated using estimated glomerular filtration rate (eGFR), Tc-99m diethylenetriamine-pentaacetate (DTPA) plasma clearance, Tc-99m mercaptoacetyltriglycine (MAG3) renography, CKD stage based on eGFR and DTPA, and renal volume at baseline and 6 months after treatment.
Results: Fifty-six patients were included (18 RAPN, 38 PCA) with a median age 66.5 years (interquartile range (IQR): 56.5-74.0). We found a significantly higher age (68.5 years; p=0.019) and Charlson comorbidity index (3.0; p=0.007) in PCA patients. The median tumor size was 3.3 cm (IQR: 2.5-3.9), and tumor characteristics did not differ significantly between RAPN and PCA. Total renal volume decreased significantly after PCA (-18.2 cm3; p=0.001). Baseline CKD stage IIIb-IV was predictive of a greater reduction in renal volume (-31.8 cm3; p=0.003) but no other renal function measures. Renal function declined significantly after either treatment based on creatinine-based measures and DTPA clearance.
Conclusions: This study found a decrease in renal function 6 months after both RAPN and PCA. Patients with CKD IIIb-IV showed a greater decline in renal volume than patients with baseline normal renal function. The renal functional changes were similar for RAPN and PCA patients.
AS-4.038
Risk factors for new onset chronic kidney disease (CKD) in patients with renal malignancy after radical nephrectomy
Mahdi M B1, Flodgaard C2, Lund F1, Andersen H R P2, Lundbye-Christensen S3, Jakobsen L H K4,5,
Alhusseinawi H1
1Aalborg University Hospital, Department of Urology, Aalborg, Denmark, 2Aalborg University, Faculty of Medicine, Aalborg, Denmark, 3Aalborg University Hospital, Unit of Clinical Biostatistics, Aalborg, Denmark, 4Clinical Cancer Research Center, Aalborg University Hospital, Department of Haematology, Aalborg, Denmark, 5Aalborg University, Department of Mathematical Sciences, Aalborg, Denmark
Background: Patients undergoing radical nephrectomy (RN) due to renal cancer are at high risk of developing chronic kidney disease (CKD). We investigated changes in eGFR and predictive factors of CKD following RN.
Methods: This was a retrospective longitudinal study of patients undergoing RN. Demographic data and possible predictive factors were collected. Patients were followed for 30-40 months, and potential development of CKD was registered. CKD was defined as eGFR < 60 ml/min. Risk factors were identified by logistic regression. Change in eGFR over time was assessed by repeated measures ANOVA. Multivariate logistic regression, incl. previously identified predictors, was compared to logistic least absolute shrinkage and selection operator (LASSO), which incl. all collected potential predictors. Predictive performance was compared by area under the ROC curve with cross-validation.
Results: 120 patients (mean age 66 ±1.0 years, 70% male) were included. CKD occurred in 58 cases (48%) eGFR decreased on the 1st postoperative day, increased after 6-12 and 30-40 months (P<0.01), albeit never regained preoperative levels. Hypertension diminished these increases, diabetes led to a decline after 30-40 months while hypertension with diabetes led to a decline at both 6-12 months and 30-40 months (P<0.05). Univariate predictors of CKD after 30-40 months included sex (OR 2.42, 95% CI 1.08-5.50), age (OR 3.29, 95% CI 1.55-7.00), hypertension (OR 2.36, 95% CI 1.11-5.02), preoperative eGFR (OR 0.22, 95% CI, 0.09-0.54) and eGFR ≤6 months preoperatively (OR 0.34, 95% CI 0.15-0.77). A prediction model fitting these predictors yielded an AUC of .64 vs .72 by LASSO (P=0.08), with difference in fit constituted by ASA-score, tumor staging and histology.
Conclusions: Predictors for development of clinically significant CKD following RN include age, sex, hypertension and preoperative eGFR. LASSO found ASA-score, tumor staging and histology to impose additional significant risk, which may be a topic of exploration in future studies.
AS-4.039
Impact of Partial Nephrectomy and Percutaneous Cryoablation on Health-related Quality of Life Two Years After Treatment – A prospective Comparative Cohort Study
Junker T1,2, Aarup Duus L1, Nørgaard B3, Azawi N4,5, Rasmussen B S B1,2, Lund L2,6, Graumann O1,2
1Odense University Hospital, Research and Innovation Unit of Radiology, Odense, Denmark, 2University of Southern Denmark, Department of Clinical Research, Odense, Denmark, 3University of Southern Denmark, Department of Public Health, Odense, Denmark, 4Zealand University Hospital, Department of Urology, Roskilde, Denmark, 5University of Copenhagen, Department of Clinical Medicine, Odense, Denmark, 6Odense University Hospital, Department of Urology, Odense C, Denmark
Background: Partial nephrectomy (PN) is the gold standard for treating stage cT1 renal cell carcinoma (RCC). However, alternative minimally invasive treatment options, such as percutaneous cryoablation (PCA), have been proposed to minimize the adverse effects on patients’ health-related quality of life (HRQoL). Therefore, this study aimed to evaluate and compare the HRQoL of patients treated with PN or PCA for stage cT1 RCC two years after treatment.
Methods: Patients treated with PN or PCA for RCC stage cT1 between 2019 and 2021 at two university hospitals in Denmark were offered inclusion. Exclusion criteria: insufficient understanding of the Danish language, cognitive deterioration, conversion to nephrectomy, or salvage procedures. The EORCT QLQ C30 questionnaire was distributed at baseline (before surgery), and one and two years postoperatively. A linear mixed-effect model was applied to detect any changes from baseline to follow-up and/or between the groups.
Results: The cohort included 168 patients (PN: 79; PCA: 89). The response rate was 100% at baseline and 88% and 74% after one and two years, respectively. Patients receiving PCA were significantly older (median 69.0 vs. 62.1 years), had a significantly higher score on the Charlson Comorbidity index (3 vs. 2), and were treated for significantly smaller tumors (3.06 vs. 3.75 cm) compared to PN. Patients treated with PCA had lower baseline scores on physical (p < 0.001), role (p = 0.004), and social functioning (p=0.044) compared to PN. A significant difference from baseline to one-year follow-up was found for emotional functioning (p=0.006) with the only HRQoL scale favoring PCA over PN. No significant changes from baseline to two-year follow-up were found for any HRQoL scales.
Conclusions: This study found significant differences between baseline HRQoL between patients treated with PCA and PN. However, no significant differences were observed in any HRQoL scales from baseline to two-year follow-up between the treatment groups.
AS-4.040
Few radically treated renal cell carcinoma (RCC) patients report a high level of distress during follow-up
Hauge E M1,2, Hjelle K M1,3, Beisland E G4, Aarstad H J5, Beisland C1,3
1University of Bergen, Department of Clinical Medicine, Bergen, Norway, 2Stavanger University Hospital, Department of Urology, Stavanger, Norway, 3Haukeland University Hospital, Department of Urology, Bergen, Norway, 4Western Norway University of Applied Sciences, Department of Health and Caring Sciences, Bergen, Norway, 5Haukeland University Hospital, Department of ENT/Head and Neck Cancer, Bergen, Norway
Background: Studies show that distress among cancer patients is common. This study aims to identify whether this applies to radically treated RCC patients during follow-up.
Methods: 278 patients radically treated for RCC (1997-2014) reported self-assessed distress using the General Health Questionnaire (GHQ) at a median (IQR) follow-up of 2.0 (1.4-4.7) years. Distress was scored according to the GHQ-Scoring (GHQ-S) (0-0-1-1) and GHQ-Likert (GHQ-L) (1-2-3-4) scoring systems, with cut-off set to ≥6 (high level of distress) and ≥25 (any level of distress), respectively. Neuroticism was tested using Eysenck Personality Inventory questionnaire. Data concerning patient, tumour, and disease status was retrieved from the local RCC database. All patients consented.
Results: The male: female ratio was 2.3:1. The rate of radical and partial nephrectomy was 155 and 123, respectively. There were 27 in the high, 74 in the intermediate, and 175 in the low risk of recurrence groups. Distress was reported by 19 (7%) and 52 (19%) patients, according to the GHQ-S and GHQ-L scoring systems, respectively. For GHQ-S, distress was correlated with higher level of education and neuroticism (r= 0.154 (p=0.011) and r=0.232 (p<0.001) respectively), but not with age, gender, risk of recurrence, and comorbidity. For GHQ-L, neuroticism and younger age significantly correlated (r=0.384 (p<0.001) and r=0.204 (p<0.001), respectively). In multivariate logistic regression for GHQ-S and GHQ-L, neuroticism was an independent predictor for both, whilst higher level of education and younger age remained predictors by GHQ-S and GHQ-L, respectively. In univariate survival analyses, distress measured by neither GHQ-S nor GHQ-L affected overall survival during follow-up.
Conclusions: In this study, only 7% of radically treated RCC patients reported high levels of distress, less than 19% reported any level of distress, and distress did not affect overall survival. Predictors of distress were neuroticism, higher level of education, and younger age.
AS-4.0413
Renal cancer survival in clear cell renal cancer compared to other types of tumor histology- a population-based cohort study
Sepp T1, Poyhonen A2, Uusküla A3, Veitonmäki T4, Kotsar A5, Murtola T6
1North Estonia Medical Centre, Urology, Tallinn, Estonia, 2Centre for Military Medicine, the Finnish Defence Forced, Riihimäki, Finland, 3Tartu University, Institute of Family Medicine and Public Health, Tartu, Estonia, 4Tampere University Hospital, Tampere, Finland, 5Tartu University Hospital, Tartu, Estonia, 6Tampere University Hospital, Department of Urology, Tampere, Finland
Background: Renal cancer (RC) is a great challenge with its rising incidence and mortality. RC survival depends on many factors, incl. tumor stage and histology. Most guidelines are based on evidence for the most prevalent histological type- clear cell RC. In this population-based study, we compared RC outcomes by histological subtype, emphasizing the effect on Cancer-specific survival (CSS) and overall survival (OS) and treatment outcomes.
Methods: The study is a retrospective population-based cohort study. All RC cases from 1995 until the end of 2017 were identified from the Finnish Cancer Registry. Comorbidities and procedure information for 1995-2018 were gathered from the national health care registry. Data on deaths was gathered from the national death certificate registry. RC cases were categorized according to tumor histology. CSS and OS were compared by histological subtype using Cox regression with adjustment for age, tumor stage, Charlson comorbidity index and surgical treatment strategy.
Results: The most common type of RC was clear cell RCC (ccRCC)(74,7%), followed by papillary RCC (pRCC, 5.7%) and chromophobe RCC (chRCC, 2.1%). CSS was better among ccRCC than all non-ccRCC combined (HR 1.62, 95% CI 1.52-1.72). For specific histological subtypes, CSS was better for chRCC (HR 0.21, 95% CI 0.12-0.37), other known histological subtypes (HR 0.20, 95% CI 0.15-0.28), pRCC (HR 0.57, 95% CI 0.46-0.70). Surgical treatment improved the CSS more for non-ccRCC but less for pRCC and chRCC. In time trend analysis, CSS improved for RC, but a statistically significant improvement in CSS was for ccRCC, not for non-ccRCC.
Conclusions: RC survival varies greatly by histological subtype. Histology should be used more in the clinical decision-making process as it may aid in deciding proper treatment: surgical management for aggressive tumors and conservative for less aggressive histological types.
AS-4.042
‘Internist’s Tumour Into Thyroid : a Case Report
Sarkar P k1, Karanjia R1, Nissanka-Jayasuriya E2, Theokli C1, Eraibey M1, Kommu S1
1Kent and Canterbury Hospital, Urology, Canterbury,Kent, United Kingdom, 2Kent and Canterbury Hospital, Histopathology, Canterbury,Kent, United Kingdom
Background: Renal cell carcinoma (RCC) is well known for its unpredictable and diverse behavior, with tendency to cause synchronous or metachronous metastasis to unusual site, which is why it is called the “internist’s tumor”.Although The thyroid gland is an infrequent site for metastasis of different primary malignancies, metastatic clear cell renal cell carcinoma (RCC) is one of the most common secondary thyroid malignancies, precisely accounted for the majority of metastatic disease to the thyroid gland . A case of Metastatic Renal malignancy to Thyroid is described with clinicopathological features and literature review.
Methods: We present a 87 year-old man who previously underwent left Radical Nephrectomy in 2009 for Grade 3 RCC. He was discharged after cancer free surveillance for 10 years and he also had trial immunotherapy with Sorafenib. He presented with 37*22*28 mm U3 thyroid nodule with euthyroid status in 2020 and subsequent cytology on January,2021 showed low risk changes Thy 3a and repeat cytology on January,2022 showed cystic content (Thy1c). He had no accompanying symptoms, such as stridor, hoarseness, or dysphagia.
Results: As the nodule continued to enlarge at 1 cm growth per year, he underwent right hemithyroidectomy on October ,2022 which showed metastatic clear renal cell carcinoma, confirmed on immunohistochemistry (Vimentin +.CD10 +,PAX8 + But CK7 -,CK20 -,TTF1 -).His subsequent Staging FDG PET CT and CT Chest, Abdomen and Pelvis showed 18 mm indeterminate cortical right renal nodule not seen in previous CT Urogram in 2017.
Conclusions: Thyroid, whilst rare, can be a site of distant metastases for renal cell carcinoma. Diagnosis can be significantly challenging due to delayed as well as unpredictable presentation whereas Early detection offers the best opportunity for metastasectomy with long term control or curative intent. Diagnosis relies on a high index of clinical suspicion in patients with prior RCC, combined with cross-sectional imaging and biopsy.
AS-4.043
Chylous after nephrectomy: A case report and mini-review
Malaguti S1, Lund L2
1Odense University Hospital and University of Southern Denmark, Odense, Denmark, 2Odense University Hospital and University of Southern Denmark, Department of Urology, Odense, Denmark
Background: Chylous is an uncommon complication usually related to gastro-hepato-biliary surgery.
The aim of the study was to evaluate the incidence of post-nephrectomy chylous and its management, with a relevant case report.
Methods: The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (P.R.I.S.M.A) of existing literature in English was used. From the period 1972-2022, we searched literature in Cochrane, Embase and Pubmed databases. Two hundred and sixteen articles were found describing one or more cases of post-nephrectomy chylous. After reviewing abstracts, 46 were read in full text and we deleted 9 doublets.
Results: The 36 articles included a variety of conservative and surgical managements with varying success. Our patients had a daily output of 50 L white chylos. After 2 days the patients was treated conservatively with no oral intake for 14 days, parenteral nutrition and somatostatin intravenously.
Conclusions: Chylous, while uncommon, can be a complication after nephrectomy. According to the literature search, conservative treatment is recommended as first choice.
AS-4.044
Pelvic kidney - a case report from Stavanger University Hospital
Espeland H, Vinje C A
Stavanger University Hospital, Urology, Stavanger, Norway
Background: Pelvic kidney is a range of anatomical abnormalities that occur when the kidney fails to rise from the pelvis during embryogenesis. Most cases are asymptomatic, although they are at greater risk of traumatic injury, infection, stone disease and other urological problems.
Methods: Here we describe the diagnosis, treatment and outcome of an 84-year-old man with a right sided pelvic kidney.
Results: When presenting at our hospital he had experienced hydrocele testis for 15 years and inguinal hernia for 5 years at the ipsilateral side as his pelvic kidney. Initially he was treated with expectancy, but due to progression of his condition with further migration of the pelvic kidney, surgical interventions were required.
Conclusions: Case presentation
AS-4.045
Stone characteristics are an important predictive factor for successful treatment of urolithiasis with shock wave lithotripsy (SWL)
Golos M1, Vinje C A2, Hauge E M2
1Stavanger University Hospital, Urology department, Stavanger, Norway, 2Stavanger Unversity Hospital, Urology department, Stavanger, Norway
Background: SWL has been a safe and effective non-invasive treatment option for nephrolithiasis since the early 1980s. This study aims to find out how stone characteristics predict outcome of SWL treatment.
Methods: This is a retrospective study looking at patients treated with SWL during 2021 and 2022, at Stavanger University Hospital. All patients were followed up with a CT scan 6-8 weeks after treatment. The stones were grouped based on density (<450 Hounsfield Units (HU), 500 – 950 HU, ≥1000 HU) size (<5 mm, 6 –10 mm, and >10 mm), and placement (urethral, upper, middle and lower calyx, and ureteropelvic junction (UPJ)). Result of treatment is grouped into four groups; stone-free rate (SFR), classified as ≤2 mm residual stone, ≥ 50% reduction in size, < 50% reduction in size, and no effect on size.
Results: Are presented as % and with 95% CI. 94 patients were treated with a total of 124 SWL procedures. In 29 (23%, 21.5 – 40.2) procedures the patients were SFR, in 12 (10%, 6.0 – 19.5) procedures the patient had a size reduction of ≥50%, in 36 (38%, 28.5 – 48.1) procedures a size reduction <50%, and in 48 (51%, 41.0 – 61.2) procedures the patient had no effect on stone size. Urethral stones had the highest SFR, N8 (66%, 36 – 96), stones localized in the upper calyx with SFR N7 (35 %, 14 – 55), and middle calyx SFR N8 (29%, 13 – 45). Stones located in lower calyx and UPJ had the lowest SFR, N4 (9%, 3 – 15) and N1 (5%, 0 – 14), respectively. SFR with regards to density, <450 HU, N6 (28.5%, 0 – 88), 500 – 950 HU, N12 (17%, 9 – 25), and ≥1000 HU, N2 (10%, 0 – 52). SFR for stone size <5mm, 6–10 mm, and >10mm was, N11 (37%, 20 – 54), N15 (22%, 13 – 31) and N2 (7%, 0 – 16), respectively.
Conclusions: Both stone size, density and placement have an impact on treatment outcome with SWL. Upper and middle calyx stones are more likely to give SFR compared to lower calyx and UPJ stones. This is also found for stones size <5mm and stones with density <450HU.
AS-4.046
Management of large renal stones with retrograde intra-renal Surgery monotherapy, a prospective descriptive study
Hassan M, Mohammed A
Luton and Dunstable Hospital, Urology, Luton, United Kingdom
Background: To evaluate the safety and efficiency of retrograde intra-renal surgery (RIRS) in the management of partial or complete staghorn renal stones as single modality.
Methods: A total of 15 patients with partial or complete staghorn renal stones who received RIRS with Ho-YAG laser between April 2021 to August 2022 were included in this study. Non contrast CT scan was used to assess for residual stones and the need for further surgery. Single-use Scope Uscope (Zhuhai Pusen Medical Technology) and reusable Flex XC (Karl-Storz Tuttlingen, Germany) used. We used 270 micron laser fibre with the dusting settings (high frequency- low energy).
Results: The patients’ age ranged from 28-82 years. The female to male ratio was 8:7. The BMI range was 21-54.4 with the mean of 32.2. Pain was the initial presentation in 80% of patients. The mean stone density was 1050HU. The group included both complete staghorn (20%) and partial staghorn (80%) as defined by the reporting radiologist. Patient choice was the dominant indication of FURS (53.8%) followed by high BMI and comorbidity in 23.1% for each. All patients had good function kidney on the ipsilateral side (as assessed by DMSA scan if needed). No ureteric access sheath was used. We used 270 micron laser with the dusting setting. The operative time ranged from 100-210 mins with the mean of 152.7 minutes. The hospital stay was mainly from 0-2 days with no post operatively complications reported. Eight patients achieved SCS in a single session (partial to complete ratio 7:1). Five patients achieved SCS in two sessions (partial to complete ratio 4:1). Two patients needed three sessions to achieve SCS (partial to complete ratio 1:1). No Clavien-Dindo complications criteria of 2 or above.
Conclusions: Retrograde intrarenal lithotripsy is a safe and effective mode of surgical management of staghorn renal calculi and can be offered as an alternative to PCNL. It is associated with less morbidity and shorter hospital stay but at the expense of needing more than one session.
AS-4.047
Ureteral stenosis after kidney transplant. Repair using ipsilateral native ureter
Ragnarsson H, Jonsson E, Jonsson J, Hilmarsson R
Landspitali University Hospital, Urology, Reykjavik, Iceland
Background: Ureteral stenosis is a major complication of kidney transplant, especially when the stenosis is at the ureteropelvic junction. Initial treatment to relieve the hydronephrosis is a nephrostomy or ureteral stent. The stenosis can then be dilated endoscopically which is usually a temporary solution requiring repeated interventions. Some patients will need a chronic ureteral stent or nephrostomy. Open surgery provides an opportunity for definitive treatment. We present four cases where the ipsilateral native ureter was anastomosed to the donor renal pelvis (ureteropyelostomy).
Methods: Four patients diagnosed with ureteral stenosis underwent ureteropyelostomy at the Department of Urology from 2012 to 2016. Two women and two men, average age 44 years. Two had renal transplants in Iceland from living donors and two in Sweden from deceased donors.
Results: Median time from kidney transplant to diagnosis of ureteral stenosis was 27,5 months (range 3-123). Time from diagnosis to ureteropyelostomy ranged from one to twenty months (median 7,5). All patients had been treated initially with nephrostomy and/or ureteral stent. The ureteropyelostomy is still patent in all patients with no evidence of restenosis and complete preservation of renal function during follow up which ranges from 3-74 months (average 42). One patient had postoperative superficial wound infection that was treated successfully.
Conclusions: Ipsilateral native ureteropyelostomy is a viable surgical option for the obstructed kidney after transplant.
SESSION V - ORAL PRESENTATIONS – BLADDER II
AS-5.048
Recurrence Free-, Cancer Specific-, and Overall Survival after treatment for urachal cancer – a nationwide retrospective study from Norway
Akhtar S N1, Haug E2, Carlsen B3, Aarsæther E J4, Karlsvik A-K5, Kjøbli E5, Hannestad I6, Müller S6, Brennhovd B7, Dimmen M8, Beisland C1,9, Gudbrandsdottir G1,9
1Department of Urology, Haukeland University Hospital, Bergen, Norway, 2Department of Urology, Vestfold Hospital, Tønsberg, Norway, 3Department of Pathology, Vestfold Hospital, Tønsberg, Norway, 4Department of Urology, University Hospital of North Norway, Tromsø, Norway, 5Department of Urology, St. Olavs University Hospital, Trondheim, Norway, 6Department of Urology, Akershus University Hospital, Lørenskog, Norway, 7Department of Urology, Oslo University Hospital, Oslo, Norway, 8Department of Urology, Bodø Hospital, Bodø, Norway, 9Department of Clinical Medicine, University of Bergen, Bergen, Norway
Background: Urachal carcinoma is a rare type of cancer in the bladder. Overall survival is reported in the range of 46-60 months for these patients, but few updated publications exist. The aim of this study is to establish updated figures for recurrence free (RFS), cancer specific survival (CSS) and overall survival (OS), as well as to explore if symptoms and tumour size is of importance in regard to survival.
Methods: Patients were retrieved from five centers. One center had no eligible patients and the final center has yet to retrieve data. The cohort consist of 38 patients, identified by both administrative registries and the medical records (by ICD and NCSP-codes). RFS, CSS and OS were estimated by use of the Kaplan-Meier (KM) method. The patients were divided into groups according to symptoms (non- symptomatic vs. symptomatic) and size (≥3 cm vs. <3 cm). Potential differences in survival between groups were tested by Log-Rank test. The study is approved by the Ethics Committee in Western Norway.
Results: Median recurrence free survival was 53 months. Median time to recurrence was 61 months. No death of urachal cancer happened after 47 months.
One-, three- and five-year RFS was 74.1%, 56.3% and 49.2%, respectively. For CSS and OS, the one-, three- and five-year figures were 94% and 94%, 69% and 67% and 59% and 54%, respectively. Non-symptomatic patients had better RFS than the symptomatic ones in KM analyses (p=0.019). Size (≥3 cm vs. <3 cm) were not significantly different regarding RFS (p=0.22). For CSS, neither non-symptomatic vs. symptomatic nor the different size groups showed significant differences regarding survival estimates (p=0.17 and p=0.058, respectively).
Conclusions: Overall Survival seems to be comparable or better in comparison with published literature. Larger size and symptomatic debut seem to have a negative impact on both RFS and CSS/OS.
AS-5.049
Adverse events during neoadjuvant chemotherapy for muscle invasive bladder cancer - a Swedish retrospective multicenter study
Eriksson V1, Holmlund J1, Wiberg E1, Johansson M1,2, Huge Y3, Alamdari F4, Svensson J5, Aljabery F3, Sherif A1
1Umeå university, Department of Surgical and Perioperative Sciences, Urology and Andrology, Umeå, Sweden, 2Länssjukhuset Sundsvall/Härnösand, Urology, Sundsvall, Sweden, 3Linköping university, Department of Clinical and Experimental Medicine, Division of Urology, Linköping, Sweden, 4Västmanland Hospital, Department of Urology, Västerås, Sweden, 5Umeå university, Department of Statistics, Umeå School of Business, Economics and Statistics (USBE), Umeå, Sweden
Background: Adverse events (AEs) during neoadjuvant chemotherapy (NAC) for muscle invasive bladder cancer (MIBC) are insufficiently reported. Clinical implications include affected cardiac, pulmonary, urinary, vascular & hematological organ systems. Purpose to evaluate the incidence and severity of AEs. Further investigating possible effects of AEs on downstaging outcomes, a surrogate marker for overall survival (OS).
Methods: A retrospective evaluation of AEs during ongoing NAC for MIBC patients analyzing individual patient data in a clinical database. We identified 687 cystectomies between 2009–2020 at four Swedish urological centers. Inclusion criteria: cT2–4aN0M0 in 261 NAC patients undergoing radical cystectomy (RC). Medical files were reviewed and AEs were assessed, including measurements by the Common Terminology Criteria for Adverse Events (CTCAE) v.5. Data were retrospectively analyzed in SPSS statistics 27.0 with Spearman rank-order correlation coefficient and Mann-Whitney U-test (MWU).
Results: A total of 251/261 patients [95% confidence interval (CI), 93–98%] experienced AEs during NAC pre-RC (mean two AEs/patient). Totally 208 patients (80%) received methotrexate, vinblastine, adriamycin (doxorubicin) and cisplatin (MVAC). Totally 200 (76.6%) received all pre-planned NAC-cycles. Most common AEs were anemia (88.9%), thrombocytopenia (44.8%) and acute kidney injury (40.6%). Patients with prematurely terminated cycles had higher AE-grades (P=0.042 MWU). A correlation between higher AE-grades and decrease in downstaging existed, in the entire cohort (−0.133; p=0.033) and in patients undergoing all pre-planned NAC-cycles (−0.148; p=0.038). Anemia and acute kidney injury were individually associated with decreased downstaging (−0.360, p=0.025 and −0.183, p=0.010, respectively).
Conclusions: NAC in MIBC poses a significant risk for AEs pre-RC with clinical implications. We propose that early detection and prevention of AEs may increase downstaging.
AS-5.050
Central Venous Access and the Risk for Thromboembolic Events in Patients Undergoing Neoadjuvant Chemotherapy and Radical Cystectomy for Muscle Invasive Bladder Cancer
Rydell H1, Huge Y2, Eriksson V1, Johansson M1,3, Alamdari F4, Svensson J5, Aljabery F2, Sherif A1
1Umeå university, Department of Surgical and Perioperative Sciences, Urology and Andrology, Umeå, Sweden, 2Linköping university, Department of Clinical and Experimental Medicine, Division of Urology, Linköping, Sweden, 3Länssjukhuset Sundsvall/Härnösand, Urology, Sundsvall, Sweden, 4Västmanland Hospital, Department of Urology, Västerås, Sweden, 5Umeå university, Department of Statistics, Umeå School of Business, Economics and Statistics (USBE), Umeå, Sweden
Background: Thromboembolic events (TEE) are high-risk complications in patients undergoing neoadjuvant chemotherapy (NAC) and radical cystectomy (RC) for urothelial muscle-invasive bladder cancer (MIBC). The purpose of the study was to investigate any differences in TEE-incidence, comparing peripherally inserted central catheter (PICC) versus a totally implanted port (PORT) as CVA (central venous access) during NAC.
Methods: We identified 947 cystectomized MIBC-patients from four Swedish medical centers in 2009–2021. Inclusion criteria were cT2-T4aN0M0 and 375 patients were finally eligible and evaluated, divided into: NAC-administered (n=283) resp. NAC-naïve-NACeligible (n=92), the latter as tentative control group. Data on TEEs and types of CVA were retrospectively collected and individually validated, from final transurethral resection of the bladder tumor (TUR-B) to 30 days post-RC. Adjusted logistic regression and log rank test were used for statistical analyses.
Results: Amongst NAC-administered, 83% (n=235) received PICCs and 15% (n=42) PORTs. Preoperative TEEs occurred in 38 PICC-patients (16.2%) and in one PORT-patient (2.4%), with 47 individual events registered. We found a significantly increased odds ratio of TEE in NAC-administered PICC-patients compared to in PORT-patients (OR: 8.140, p-value: 0.042, 95% CI 1.078– 61.455).
Conclusions: Our findings indicate a greater risk for pre-RC TEEs with PICCs than with PORTs, suggesting favoring the usage of PORTs in MIBC-NAC-patients.
AS-5.051
Recommended Antimicrobial Prophylaxes Prior to Cystectomy / Urinary Deviation Does Not Cover the Majority of Microbiota Found in the Ileum
Aune E1, Villmones H C2, Halland A3, Löffeler S1, Haug E S1
1Sykehuset i Vestfold, Urology, Tønsberg, Norway, 2Sykehuset i Vestfold, Microbiology, Tønsberg, Norway, 3Porsgrunn Urologi, Porsgrunn, Norway
Background: Urinary diversion (UD) performed associated with radical cystectomy (RC) is an operation with high complication rates. Urinary tract infections (UTIs) and urosepsis contribute significantly to the morbidity associated with RC. Guidelines on antimicrobial prophylaxis for patients undergoing RC and urinary deviation are based on data from colorectal surgery.We identified microbiota found in ileum and analyzed their susceptibility for standard antimicrobial prophylaxis.Norwegian guidelines recommend doksysyklin po/iv 400 mg + metronidazol po/iv.
Methods: 235 consecutive patients (April 2016-May 2020) that underwent urinary diversion at Vestfold Hospital Trust (Tønsberg, Norway) were enrolled in the local quality register based on broad informed patient consent.Microbial specimen were collected during surgery using a swab from the luminal wall approximately 25 cm from the ileocecal valve. Extended cultivation and analysis of the specimen were performed. We categorized microbiota found in the ileum into three groups; colon-like bacteria (Enterobacteriales (gram neg. rods), obligate anaerobes, Enterococcus spp.), oral-like bacteria or fungal (Candida spp.)
Results: In the ileum we detected bacterial growth in 89%. In this group we found that 69.4% had oral-like bacteria, 19.6% had colon-like bacteria. In 54.5% of the patients we detected Candida in the ileum, but mostly in combination with bacteria. In only 3.8% there was growth of Candida only. In 7.2% we found no microbiota growth.
Conclusions: Current guidelines for antibiotic prophylaxis do not fully cover the bacteria found in the ileum.The need of antifungal prophylaxis during urological ileal reconstructive surgery should be considered.
AS-5.052
Microbial trends in infection-related readmissions following radical cystectomy for bladder cancer
Vejlgaard M1, Maibom S L1, Joensen U N1, Moser C2, Røder A1
1Rigshospitalet, Department of Urology, Copenhagen, Denmark, 2Rigshospitalet, Department of Microbiology, Copenhagen, Denmark
Background: One in two patients are readmitted following radical cystectomy (RC) for bladder cancer. The most common cause of readmission is by far infection, yet international guidelines provide no official recommendations on perioperative preventative antibiotics. This study aims to report infection-related readmissions and describe the pathogens obtained at readmissions, including their sensitivity to antimicrobials.
Methods: A retrospective review of 785 patients who had undergone RC for bladder cancer at a tertiary centre in Denmark. All patients received prophylactic cefuroxime preoperatively and mecillinam at stent- or catheter removal on postoperative day 10. Data was collected through the national medical records and microbiology database. Uni- and multivariable regression analyses were carried out to identify risk factors of infection-related readmissions.
Results: Within 90 days of surgery, 314 infection-related readmissions (51% of all readmissions) were registered. The majority were due to infections in the urinary tract. The most common pathogen found was Enterococcus, contributing to 24% of all samples. In blood cultures, the most dominant species were Escherichia and Staphylococcus. Due to the heterogeneity in microbial species, more than one third of the samples where mecillinam was tested showed resistance. Most isolates were sensitive to piperacillin + tazobactam. Orthotopic neobladder and continent cutaneous reservoir were associated with higher risk of infection-related readmission than ileal conduit (odds ratios 2.78 and 3.19, respectively, p-values<0.001). Active tobacco smoking at surgery was associated with a lower risk of infection-related readmissions, compared to non-smokers (odds ratio 0.50, p-value=0.003).
Conclusions: Nearly one third of all patients experienced at least one postoperative infection-related readmission, and microbiological analyses showed a wide range of species responsible for infections.
AS-5.053
Does pre-cystectomy anemia following neoadjuvant chemotherapy in muscle invasive bladder cancer affect survival?
Eriksson V1, Elfving-Long J1, Johansson M1,2, Huge Y3, Alamdari F4, Aljabery F3, Svensson J5, Banday V1, Sherif A1
1Umeå university, Department of Surgical and Perioperative Sciences, Urology and Andrology, Umeå, Sweden, 2Länssjukhuset Sundsvall/Härnösand, Urology, Sundsvall, Sweden, 3Linköping university, Department of Clinical and Experimental Medicine, Division of Urology, Linköping, Sweden, 4Västmanland Hospital, Department of Urology, Västerås, Sweden, 5Umeå university, Department of Statistics, Umeå School of Business, Economics and Statistics (USBE), Umeå, Sweden
Background: Previous studies on patients with mainly NAC (neoadjuvant chemotherapy)-naïve muscle invasive bladder cancer (MIBC) undergoing radical cystectomy (RC), have shown that preoperative anemia (PA) affects the overall survival (OS) negatively. Yet knowledge is lacking regarding PA effects on survival in MIBC NAC-patients. PA is also known as a hematological side effect from NAC. Furthermore, patients with PA are at risk of receiving allogenic blood transfusions (ABTs), which has been associated with worsened cancer-prognosis. The purpose was to evaluate how PA impacts OS in NAC and NAC-naïve MIBC patients, and if ABTs impact survival.
Methods: A total of 248 Swedish patients from four urological centers with MIBC clinically staged T2-T4aN0M0, stratified over NAC or NAC-naïve patients eligible for NAC, undergoing RC between 2009–2021, were analyzed in reference to PA and retrospectively evaluated. NAC-naïve was set as a parallel control group. HR (hazard ratio) was calculated unadjusted and adjusted for CACI, gender, cTNM or pTNM up to 3 yrs.
Results: NAC-patients with PA had a better survival than NAC-naïve patients with PA (Log-Rank p=0.001). The prevalence of PA was higher in the NAC-group (79%) than in the NAC-naïve group (22%). There were no detectible differences in survival in NAC-patients with PA compared to NAC-patients without PA (HR adjusted; 0.7 (0.3-1.7) p= 0.46). ABTs increased death in NAC-naïve patients if they received 1-4 units (HR adjusted; 2.4 CI 1.1-5.4, p=0.029) or ≥5 units; (HR unadjusted; 3.2 CI 1.3-7.8, p=0.012) and in the NAC-group if ≥5 units; (HR unadjusted; 3.3 CI 1.3-8.2, p=0.012).
Conclusions: PA after NAC is not associated with worse survival, with the clinical implication that NAC should not be restricted in reference to risk for PA. ABTs are associated with increased death, regardless of receiving patients were NAC or NAC-naïve.
AS-5.054
DaBlaCa-17: Long term survival of patients with muscle invasive bladder cancer undergoing radical cystectomy before and after implementation of neoadjuvant chemotherapy with gemcitabine-cisplatin: a natural experiment study
Körner S K1,2, Dreyer T1, Carus A3,4, Hammer Dohn L5, Joensen U N6,7, Wrist Lam G8, Jensen N V9, Fabrin K4,10, Knak Jensen T11, Pappot H7,12, Agerbæk M13, Bjerggaard Jensen J1,2
1Aarhus University Hospital, Department of Urology, Aarhus, Denmark, 2Aarhus University, Department of Clinical Medicine, Aarhus, Denmark, 3Aalborg University Hospital, Department of Oncology, Aalborg, Denmark, 4Aalborg University, Department of Clinical Medicine, Aalborg, Denmark, 5Herlev and Gentofte University Hospital, Department of Oncology, Copenhagen, Denmark, 6Copenhagen University Hospital, Rigshospitalet, Department of Urology, Copenhagen, Denmark, 7Copenhagen University, Department of Clinical Medicine, Copenhagen, Denmark, 8Herlev and Gentofte University Hospital, Department of Urology, Copenhagen, Denmark, 9Odense University Hospital, Department of Oncology, Odense, Denmark, 10Aalborg University Hospital, Department of Urology, Aalborg, Denmark, 11Odense University Hospital, Odense, Department of Urology, Odense, Denmark, 12Copenhagen University Hospital, Rigshospitalet, Department of Oncology, Copenhagen, Denmark, 13Aarhus University Hospital, Department of Oncology, Aarhus, Denmark
Background: RTCs report improved survival outcomes following use of neoadjuvant chemotherapy (NAC) in patients with muscle invasive bladder cancer (MIBC). NAC with gemcitabine-cisplatin was implemented nationwide in Denmark on 1 January 2013. Purpose: To compare survival outcomes of patients with MIBC before and after implementation of NAC in Denmark.
Methods: We collected data on all 851 patients undergoing radical cystectomy in 2010-2015 who were potential candidates for NAC based on T-stage, age, and renal function. We compared a cohort before the implementation of NAC (Cohort 2010-12) with a cohort after implementation (Cohort 2013-15). Moreover, patients in Cohort 2013-15 receiving NAC (+NAC) were compared to patients in Cohort 2013-15 not receiving NAC (-NAC). We compared pathological results after radical cystectomy and oncological outcome between the cohorts. Overall survival, disease-free survival, and disease-specific survival were compared with Kaplan-Meier plots, univariate and multivariate Cox regression.
Results: When comparing cohort 2013-15 with Cohort 2010-12, pT0 was more frequent in the late cohort: 34% vs. 18% (p < 0.001); and 46% vs. 16% in +NAC compared with -NAC (p < 0.001) within cohort 2013-15. Overall survival, disease-free survival, and disease-specific survival at 5 years after cystectomy were not improved in Cohort 2013-15 compared with 2010-12 with adjusted hazard ratios of 1.14 (95% CI: 0.89–1.45), 0.98 (95% CI: 0.75–1.27) and 1.08 (95% CI: 0.82–1.42), respectively.
Conclusions: The simultaneous nationwide implementation of NAC in Denmark makes it a natural experiment study with real-world evidence comparing patients before and after NAC implementation. Despite an increase in pathologic downstaging to pT0 in the cystectomy specimen after NAC implementation, we observed no improved survival. Reasons for these findings may include limited effect of NAC with gemcitabine-cisplatin in a modern MIBC patient cohort, or differences in the cohorts that we were unable to account for.
AS-5.055*
DaBlaCa-16: Retrosigmoid versus conventional ileal conduit in robot-assisted radical cystectomy, a randomized controlled trial – 90-day postoperative complications in the MOSAIC trial
Brandt S1,2, Körner S K1,2, Milling R1,2, Nielsen N K1,2, Kingo P S1, Joensen U N3,4, Bro L5, Livbjerg A H6, Fabrin K6, Vrang M7, Vangedal M7, Lam G W7, Jensen J B1,2
1Aarhus university Hospital, Urology, Aarhus, Denmark, 2Aarhus University, Clinical Medicine, Aarhus, Denmark, 3Copenhagen University Hospital, Rigshospitalet, Urology, Copenhagen, Denmark, 4Copenhagen University, Clinical Medicine, Copenhagen, Denmark, 5Odense University Hospital, Urology, Odense, Denmark, 6Aalborg University Hospital, Urology, Aalborg, Denmark, 7Herlev and Gentofte University Hospital, Urology, Copenhagen, Denmark
Background: Radical cystectomy (RC) with ileal conduit is the gold standard when treating muscle-invasive bladder cancer. Up to 15% of patients undergoing RC develop benign ureterenteric strictures within two years, especially on the left side where the ureter is passing behind the sigmoid colon. A modified retrosigmoid ileal conduit has been associated with reduced rate of left-sided strictures. The retrosigmoid ileal conduit has never been investigated in a randomized controlled setting.This study aims to evaluate the safety of robot-assisted RC with the retrosigmoid ileal conduit (MOSAIC) compared with the conventional ileal conduit in bladder cancer treatment.
Methods: The MOSAIC study is a randomized multicenter trial. Patients were randomized 1:1 between intracorporeal conventional ileal conduit ad modum Bricker or retrosigmoid ileal conduit (MOSAIC), where the ileal segment was elongated to go behind the sigmoid, making it possible to shorten the left ureter to the same level as on the right side. The primary endpoint is left-sided strictures within two years, pending results. This study reports the secondary outcome of 90-day postoperative complications using the Clavien Dindo (CD) Classification system. Patients’ individual pre and postoperative renal function was assessed using serum-creatinine and renography.
Results: Recruitment was completed (august 2022) with 303 patients included. Retrosigmoid ileal conduit (MOSAIC) was performed in 137 patients. The RR of CD III or higher was 1.124 [0.964;1.311] (P=0.365) in the retrosigmoid group compared with the conventional group. Intention-to-treat analyses showed no statistically significant difference in operating time, bleeding, bowel function, length of stay or effect on renal function within 90 days.
Conclusions: The intracorporeal retrosigmoid ileal conduit (MOSAIC) with robot-assisted RC was technically feasible and there were no differences in 90-day complications compared with the conventional ileal conduit ad modum Bricker.
* Winner of the First prize for best abstract in the field of Urologic cancer
AS-5.056
Cancer specific survival (CSS) after radical cystectomy (RC) – retrospective study of a 10-year cohort at a tertiary referral center, Haukeland University Hospital
Bergesen A1, Roth I1, Haugland J1, Beisland C1,2, Gudbrandsdottir G1
1Haukeland University Hospital, Department of urology, Bergen, Norway, 2University of Bergen, Department of clinical medicine, Bergen, Norway
Background: To provide bladder cancer patients an optimal pathway, intimate knowledge of local treatment results is crucial. The aim of this study is to report survival estimates following RC, and to identify independent predictors for CSS.
Methods: From medical records, we identified 449 patients who underwent RC for bladder cancer at our institution during 2013- 2022. Data regarding patient characteristics, surgical procedures, histopathology, complications and follow-up were registered. We considered 31 (7%) of the patients palliative due to preoperative metastatic disease or surgical incurable disease, leaving 418 patients for further analyses. The patients were grouped according to tumor stage (localized pT0-3a vs. locally advanced ≥pT3b), lymph node status (negative pN0 vs. positive pN+), surgical margin (negative R0 vs. positive R+) and if they received neoadjuvant chemotherapy (NAC) or not (NAC+ vs. NAC0). Comorbidity was reported using age adjusted Charlson comorbidity index (CCI). CSS was estimated by the Kaplan-Meier method, and we used the Cox PH model for multivariate analyses. The study is a clinical audit, and thus exemption from ethical approval.
Results: Median age at RC was 69 years (IQR 62-74) and 78% were male. The mean age adjusted CCI was three. The 1-, 3- and 5-year CSS was 92%, 78% and 75%. The number of patients having locally advanced, N+ and R+ disease was 69 (17%), 72 (17%) and 23 (6%) respectively. The NAC+ group consist of 140 patients (33%). In univariate analyses, patients with locally advanced tumor, R+, N+ and female gender had poorer survival. NAC- patients had a better outcome. Multivariate analyses showed that locally advanced tumor, R+ and N+ were independent predictors for worse CSS. NAC+, however was an independent predictor for better CSS.
Conclusions: The cancer specific outcome in this study is comparable to published results. Locally advanced tumor, R+ and N+ are independent predictors of worse CSS, whilst patients receiving NAC has better CSS.
AS-5.057
Quality of life following the open vs robot-assisted radical cystectomy (BORARC) trial
Vejlgaard M1, Maibom S L1, Joensen U N1, Thind P O1, Rohrsted M1, Aasvang E K2, Kehlet H3, Røder A1
1Rigshospitalet, Department of Urology, Copenhagen, Denmark, 2Rigshospitalet, Department of Anaesthesiology, Copenhagen, Denmark, 3Rigshospitalet, Section for Surgical Pathophysiology, Copenhagen, Denmark
Background: The impact of radical cystectomy (RC) on quality of life (QoL) is largely unknown, and there is a lack of randomised trials investigating patient reported outcomes between minimally invasive and open surgery. A better understanding of QoL could have implications for treatment choice. The aim of the current study was to examine QoL before and after RC and compare robot-assisted laparoscopy with intracorporeal urinary diversion (iRARC) to open surgery (ORC).
Methods: A predefined secondary analysis of a single-centre, double-blinded, randomised feasibility trial including 50 patients undergoing iRARC with ileal conduit (n=25) or ORC with ileal conduit (n=25). Patients were followed 90 days postoperatively. Primary outcome was patient-reported QoL using the EORTC Cancer-30 and muscle-invasive-bladder-cancer BLM-30 QoL questionnaires before and after RC. Differences between randomisation arms as well as changes over time were evaluated.
Results: All patients underwent the allocated treatment. No difference in QoL was found between randomisation arms, but we report an overall postoperative improvement in QoL in the following domains: future perspectives, emotional functioning, and social functioning. Sexual functioning worsened postoperatively. There was no association between having experienced a major complication or lengthy hospitalisation and worse postoperative QoL.
Conclusions: The QoL does not appear to depend on surgical technique. Apart from sexual functioning, patients report stable or improved QoL within the first 90 postoperative days.
AS-5.058*
What is the role of telemedicine in emergency urology in Covid era?
Fojecki G1, Laigaard J2
1OUH, Urology, Odense, Denmark, 2Hospital of Southern Denmark, Urology, Åbenrå, Denmark
Background: Telemedicine could improve equality in healthcare, cut carbon gasses emission and reduce transmission of infectious diseases. We aimed to evaluate the applicability of telemedicine in emergency urology.
Methods: This prospective qualitative study was approved by the local scientific committee. After being informed about the study, patients, bedside caregivers and urologists filled out questionnaires investigating the satisfaction and applicability of a telepresence robot at the urology ward and emergency department at the Hospital of Southern Denmark, Aabenraa. The robots are equipped with wheels, and two cameras, a microphone, speakers, and a 14-inch screen that allow staff and patients to interact. The urologist operated the robot from a remote location, using a personal computer with internet access and the Beam App. The study was carried out between March 2021 and May 2021. The primary outcome was the number of patient encounters solved without the urologist’s physical presence. We further assessed the satisfaction with the telecommunication.
Results: Most patients were male (79%), with a mean age of 64 (SD ± 17). Two out of the department’s 10 urologists participated in the study. A physical examination was required in 7 out of 54 encounters. The caregivers would have preferred the urologist physically present in 11 cases, in most cases “for the patient’s sake”. Most patients (71%) “agreed” or “strongly agreed” that they were willing to be attended by a telepresence robot at future evaluations and generally, patients gave high satisfaction scores. The most frequent reasons for being seen by a urologist were rounds 12, urinary tract infections 9 , discharge 5, urolithiasis 5, and hematuria 4.
Conclusions: Most patients could be evaluated using a telepresence robot, though implementation among the department’s urologists was a challenge.
*Winner of the Third prize for best abstract in the field of benign Urology
SESSION VI - ORAL PRESENTATIONS – PROSTATE II
AS-6.059
Can Stockholm3 predict post-operative risk (CAPRA-S score) using evidence from the STHLM3 Radical Prostatectomy Cohort?
Palsdottir T
Karolinska Institutet, Medical Epidemiology and Biostatistics, Stockholm, Sweden
Background: Grading of prostate biopsies are used as a proxy for prostate cancer disease evaluation and reclassification of grade on radical prostatectomy (RP) is common. Our aim was to determine if Stockholm3 can predict high post-operative risk using CAPRA-S risk classification as well as compare pre-operative ISUP grade to post-operative grade.
Methods: We used data from the STHLM3 Radical Prostatectomy Cohort, including men that participated in the STHLM3 trial that underwent a RP. The study was conducted 2012-2015 and we included men that had a Stockhom3 test, a systematic biopsy and a RP within one year from the test. We compare the ISUP grading from biopsy to RP as well as explore how well the Stockholm3 represents post-operative risk according to the CAPRA-S score.
Results: We included 803 men from the STHLM3 study that had a RP within a year from the Stockholm3 test. The median time from Stockholm3 to RP was 207 days (IQR: 167-255). Of those, 638 (79%) had a positive Stockholm3 and 681 (85%) had a PSA≥3 ng/ml. In Table 1 the men are divided into Stockholm3 categories and compared to CAPRA-S categories. We see that none (0%) of the operated men with low risk according to Stockholm3 had a high-risk CAPRA-S score (≥7). Results also show that 60% of the men with low pre-operative risk on Stockholm3 had a low CAPRA-S risk (0-1). Furthermore, we compared pre-operative to post-operative ISUP grade and found that 59% were correctly classified on biopsy (same ISUP grade on biopsy and RP) while only 18% were upgraded and 23% were downgraded.
Conclusions: Stockholm3 reflects well the risk evaluated from RP using CAPRA-S score. Furthermore, we show that a higher proportion of men in the STHLM3 study were correctly graded on biopsy compared to previous studies.
AS-6.060
Clinical consequences of biopsies in patients with a positive Stockholm3-test and negative prostate magnetic resonance imaging
Vigmostad M N1,2, Vinje C A1,3, Kjosavik S R2,4, Grönberg H5,6, Gilje B7, Skeie S8
1Stavanger University Hospital, Department of Urology, Stavanger, Norway, 2University of Stavanger, Faculty of Health Sciences, Stavanger, Norway, 3University of Bergen, Department of Clinical Science, Bergen, Norway, 4Stavanger University Hospital, The General Practice and Care Coordination Research Group, Stavanger, Norway, 5Capio St. Göran`s Hospital, Department of Surgery, Stockholm, Sweden, 6Karolinska Institutet, Department of Medical Epidemiology and Biostatistics, Stockholm, Sweden, 7Stavanger University Hospital, Department of Oncology, Stavanger, Norway, 8Department of Research, Stavanger University Hospital, Stavanger, Norway
Background: Magnetic resonance imaging (MRI) combined with the Stockholm3-test can be used to inform biopsy decision making. The clinical consequences of performing biopsies in patients with a positive Stockholm3-test and a negative MRI are unclear. Our objective was to determine the clinical consequences of performing biopsies in men with a positive Stockholm3-test and a negative MRI.
Methods: In a real-life setting, from 2017 to 2020, 438 men with a positive Stockholm3-test and a negative MRI underwent systematic biopsies.
Participants underwent blood sampling for the Stockholm3-test, 1.5/3.0T MRI and systematic biopsies.
The results of the Stockholm3-test are divided into risk classes. The main outcome was to explore clinical consequences of performing biopsies in men with a positive Stockholm3-test and a negative MRI.
Results: Median prostate-specific antigen was 4.5ng/ml (1.5-36) and median age was 69 years. Biopsies detected ISUP ≥ 2 in 48 men (11%, (95% CI 8.0 - 13.9)). Of these, 22 men (5.0%, (95% CI 3.0 - 7.1)) received radical treatment with either radical prostatectomy or external beam radiotherapy, i.e. 5% of the included patients (95% CI 3.0 - 7.1). The remaining 26 that were not treated were followed in active surveillance protocol with a new MRI prior to biopsies within 1 year.Out of 182 patients in Stockholm risk classes 2-6, 6 men (3.3%) were radically treated and 5 (2.7%) followed in active surveillance. In risk class 7, 16 (6.3%) out of 256 patients were treated and 21 (8.2%) followed in active surveillance. Limitations include the lack of follow up data.
Conclusions: These findings provide evidence that for men with a positive Stockholm3-test and a negative MRI there are minimal clinical consequences of performing systematic biopsies in risk classes 2-6. For patients in Stockholm3 risk class 7, the consequences of biopsies should be considered with shared decision making.
AS-6.061*
Reproducibility of cognitive fusion coaxial transperineal prostate biopsies
Honoré A1, Moen C A1, Juliebø-Jones P1,2, Chaudhry A A1, Rawal R1, Sandøy A1, Reisæter L A R3, Gravdal K4, Beisland C1,2
1Haukeland University Hospital, Urology, Bergen, Norway, 2University of Bergen, Department of Clinical Medicine, Bergen, Norway, 3Haukeland University Hospital, Radiology, Bergen, Norway, 4Haukeland University Hospital, Pathology, Bergen, Norway
Background: Debate remains whether cognitive fusion prostate biopsies are adequate to use in clinical practice. One argument is the lack of reproducibility of the procedure between operators, although no study has addressed this issue. There is thus a knowledge gap regarding the number of procedures needed to attain a sufficient level of accuracy.
Methods: Patients who underwent transperineal (TP) prostate biopsy between January 1st, 2018 and May 31st, 2022 in our department were included. Four different urologists performed all biopsy procedures. Cancer detection rate (CDR) was defined as finding cancer on biopsy, either new or confirmatory for patients in active surveillance. Overall pathology detection rate (ODR) was defined as finding cancer but also included other histological changes such as inflammation or atrophy. Lesions on multiparametric MRI of the prostate were described using Pi-RADS v.2.0 and 2.1. The study is approved by the regional ethics committee in Western Norway, and all patients have consented.
Results: 1028 TP biopsies were performed. Total cancer detection rate (CDR) by TP biopsy was 70% and overall pathology detection rate (ODR) was 88.4%. CDR/ODR categorized by PI_RADS score on the MRI finding was 90/ 98% for PIRAD 5, 70%/ 88% for PIRAD 4 and approximately 40/ 70% for PIRAD 3 changes. CDR/ODR stabilized for all operators at approx. 50 procedures.
Conclusions: Coaxial cognitive fusion TP prostate biopsy is highly reproducible and operator independent. The threshold for the number of procedures required to reach the institutional level for CDR and ODR was approximately 50.
*Nominee for best abstract in the field of Urologic cancer
AS-6.062
Relative risk of prostate cancer
diagnosis and death following initial non-malignant biopsies
Stroomberg H, Brasso K, Røder A, Benzon Larsen S, Helgstrand T
Rigshospitalet, Department of Urology, Copenhagen, Denmark
Background: To compare the incidence of subsequent prostate cancer diagnosis and death following an initial non-malignant systematic TRUS biopsy to an age- and calendar-year matched population over a 20-year period.
Methods: This population-based analysis compares a cohort of all men with initial non-malignant TRUS biopsy in Denmark between 1995-2016 (N=37,231) to the Danish population matched by age and calendar year, obtained from the NORDCAN 9.1 database. Age and calendar year corrected standardized prostate cancer incidence (SIR) and prostate cancer-specific mortality ratios (SMR) were calculated and the heterogeneity between age groups assessed with the Cochran’s Q.
Results: Median time to censoring was 11 years, and 4,434 men were followed for more than 15 years. The corrected SIR was 5.2 (95%CI: 5.1-5.4) and corrected SMR was 0.74 (95%CI: 0.67-0.81). Estimates differed between age groups (P<0.001 for both) with a higher SIR and SMR among younger men.
Conclusion: Men with non-malignant TRUS biopsy have a much higher incidence of prostate cancer but a risk of prostate cancer death below the population average. This underlines that the oncological risk of cancers missed in the initial TRUS biopsy is low. Accordingly, attempts to increase sensitivity of initial biopsy are unjustified. Moreover, current follow-up after non-malignant biopsy is likely overaggressive, particularly in men over the age of 60.
AS-6.063
Cause of death registry validation in men with initial non-malignant biopsy
Brasso K, Benzon Larsen S, Helgstrand T, Røder A, Stroomberg H
Rigshospitalet, Department of Urology, Copenhagen, Denmark
Background: Epidemiological research is possible, however, the quality depends on the quality of data. The cause of death registry is accurate for men diagnosed with prostate cancer, however it is unknown if prostate cancer death is attributed to a person, if cause of death is not clear and the man has been under the suspicion of prostate cancer, so called attribution bias. Attribution bias can be important in men unlikely to die of prostate cancer as it could lead to a overestimation of disease-specific death.
Methods: From the Danish Prostate Cancer Registry men with an initial non-malignant biopsy between Jan. 1st, 1995 to Dec. 31st, 2016 who died of PCa (N=964) or other causes (N=9,362) up until 31st of December 2019 were selected. Of the men who died of other causes 1000 men were randomly selected and were together with all prostate cancer deaths manually assessed. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy were calculated for the cause of death registry with the manual assessment as standard accompanied by binomial 95% confidence intervals (95%CI).
Results: There was a total of 428 true positives and 353 false positives prostate cancer-specific deaths. Moreover, 993 true negatives and 7 false negatives were assessed for other cause of death. This led to an NPV of 99.3% (95%CI: 98.6-99.7), a PPV of 54.8% (95%CI: 51.2-58.3), sensitivity of 98.4% (95%CI: 96.7-99.4), specificity of 73.8% (95%CI: 71.3-76.1) and accuracy of 79.8% (95%CI: 77.8-81.6).
Conclusions: In men under the suspicion of prostate cancer, with an initial non-malignant biopsy, the cause of death is highly reliable in defining who does not die of the disease at the cost of overestimating the disease-specific death. This indicates that attribution bias plays a large role in a setting where disease-specific death is unlikely. Thus, future registry studies in similar settings should control the cause of death to assure disease-specific mortality is not inflated.
AS-6.064
Utility of Pre–biopsy Magnetic Resonance Imaging (MRI) in Prostate Cancer (PC) and impact on clinical T-staging in Norway
Haug E S1, Myklebust T A2, Juliebø-Jones P3, Reisæter L A R4, Aas K5, Berg A S6, Müller C7, Hofmann B8, Størkersen Ø9, Nilsen K L2, Johannessen T B2, Beisland C3
1Vestfold Hospital Trust, Urological, Tønsberg, Norway, 2Norwegian Cancer Registry, Oslo, Norway, 3Haukeland University Hospital, Urological, Bergen, Norway, 4Haukeland University Hospital, Radiology, Bergen, Norway, 5Akershus Universityhospital, Urological, Oslo, Norway, 6Vestre Viken Hospital, Oncological, Drammen, Norway, 7Sørlandet Hospital, Oncological, Drammen, Norway, 8Norwegian University of Science and Technology, Health science, Gjøvik, Norway, 9St Olav Hospital, Pathology, Trondheim, Norway
Background: Although MRI was introduced in the 1980’s, MRI of the prostate (MRI-P) was hardly mentioned in clinical practice before 2007. However, when the Norwegian public healthcare system in 2015 introduced pre-biopsy MRI-P as the standard of care for diagnosing PC, it already was in widespread use. The 8th-edition of the TNM classification (2017), contrary to the seventh TNM edition (2010), specifically states that clinical T-staging (cT-stage) in PC should be based on digital rectal exam (DRE) only. Since 2017, cT-stage by different modalities (DRE, MRI) are registered separately 7 in the Norwegian Prostate Cancer registry (NPCR). In this study we wanted to explore the use of MRI-P in Norway and correlate this to staging of PC over time.
Methods: Data on the use of MRI-P was available from Norwegian Health Economics Administration (Helfo) 2013-2021, including the total of MRI-P’s for detection, follow-up and staging. All patients registered in the Norwegian Prostate Cancer Registry 2004-2021 were retrieved. There were 69,892 were eligible patients for analyses of reported cT-stage at diagnosis over the study period.
Results: Around 4,000 MRI-P’s were performed in Norway in 2013, approximating and stabilizing around 14,000 yearly examinations from 2016 onwards. Contribution from private MRI providers reached a maximum of 2000 examinations in 2019 and has been decreasing thereafter. In 2021, a MEAN 2.7 MRI-P’s were performed for every new case of PCa diagnosed. The proportion of non-palpable PCa at diagnosis dropped to 20 % with the increasing utilisation of MRI-P. However, a sudden increase to 50 % was noticed with the introduction of separate reporting of cT-stage by both DRE and MRI-P in 2017.
Conclusions: The annual number of MRI-P in Norway has reached a plateau since 2016. The introduction of MRI-P has affected the reporting of cT-stage. Most likely is the upstaging caused by clinician’s interpretation of visualised tumour extension beyond the findings at DRE.
AS-6.065
Predictors of upgrading from low-grade cancer at prostatectomy in men with biparametric magnetic resonance imaging
Christiansen O1,2,3, Bratt O4,5, Kirkevold Ø1,6,7, Šaltytė Benth J1,2,8, Manoharan P9, Selnes A10, Skaaheim Haug E11, Slaaen M1,2
1Innlandet Hospital Trust, The Research Centre for Age Related Functional Decline and Diseases, Ottestad, Norway, 2University of Oslo, Institute of Clinical Medicine, Oslo, Norway, 3Innlandet Hospital Trust, Department of urology, Hamar, Norway, 4Sahlgrenska Academy, Institute of Clinical Science, Gothenburg, Sweden, 5Sahlgrenska University Hospital, Department of Urology, Gothenburg, Sweden, 6Norwegian Advisory Unit on Ageing and Health, Sem, Norway, 7NTNU, Faculty of Health, Care and Nursing, Gjøvik, Norway, 8Akershus University Hospital, Health Services Research Unit, Lørenskog, Norway, 9Innlandet Hospital Trust, Department of Radiology, Hamar, Norway, 10Oslo University Hospital, Department of Urology, Oslo, Norway, 11Vestfold Hospital Trust, Department of Urology, Tønsberg, Norway
Background: Prostate specific antigen (PSA) density has previously been identified as a predictor of histological upgrading at radical prostatectomy, but how information from pre-treatment bi-parametric magnetic resonance imaging (bpMRI) contributes needs further clarification. The objective of this register-based study was to identify predictors of upgrading at prostatectomy in men with Grade group (GG) 1 and pretreatment bpMRI.
Methods: This single-center study included men with GG 1 cancer on prediagnostic biopsy, who underwent bpMRI and robotic-assisted radical prostatectomy (RARP) between March 2014 and September 2019. We estimated logistic regression models to explore predictors for upgrading. The explored potential predictors were age, PSA density, tumor stage and Prostate Imaging Reporting and Data System (PI-RADS) score (dichotomised 1–3 versus 4–5).
Results: Upgrading was observed in 56% (73/130) of the men. PSA density was the only significant predictor for upgrading (unadjusted OR = 1.7, 95% CI 1.2; 2.4 adjusted OR = 1.7, 95% CI 1.2; 2.5). The probability of upgrading was lower for men with a PIRADS 1–3 than for PIRADS 4–5, but the difference was not statistically significant (adjusted OR 0.4, 95% CI 0.2; 1.1, p = 0.082). Among men with PI-RADS 1–3, the probability increased with increasing PSA density (p = 0.036). With PI-RADS 4–5 the probability of upgrading was high over the entire PSA density range.
Conclusions: PSA density is a clinically important factor to predict upgrading from GG1 when bpMRI shows PI-RADS 1–3. In men with PI-RADS 4–5 on bpMRI, the probability of an undetected GG 2–5 cancer is high regardless of the PSA density.
AS-6.066
Impact of pre-biopsy MRI on concordance of ISUP grade group in prostate biopsies and radical prostatectomy specimens
Norby G O1, Rud E2, Eri L M3, Baco E1, Svindland A3, Berge V1
1Oslo Universitetssykehus, Dept of Urology, Oslo, Norway, 2Oslo Universitetssykehus, Dept of Radiology, Oslo, Norway, 3Universitetet i Oslo, Institutt for klinisk medisin, Oslo, Norway
Background: Biopsy Gleason score/ISUP grade group is essential in prognostic evaluation of prostate cancer patients. Over the recent years, pre-biopsy MRI has become standard in our diagnostic workup in these patients. We wanted to investigate whether MRI and subsequent targeted biopsies is associated with more accurate histopathological grading of the tumour.
Methods: Using data from our prospective prostate cancer registry, we defined two patient groups. Group 1 (n=1104) consists of all patients that underwent radical prostatectomy (RP) in our hospital from 2009 to 2014 without pre-biopsy MRI. Similarly, group 2 (n=1415) consists of all patients operated in the years 2019-2022 following biopsies with MRI/ultrasound fusion technology. In each patient, core needle biopsy and RP specimen ISUP grade group were compared. Predictors of upgrading from biopsy to RP specimen were assessed in multivariate logistic regression analyses. Statistical significance p<0.05.
Results: Concordance between ISUP grade group in biopsy and RP specimen was 52.1 % in group 1, and 59.2 % in group 2 (p<0.001). In group 1 and 2 respectively, 28.3 % and 22.6 % of the patients were upgraded (p<0.001), while 19.6 % and 18.2 % were downgraded (p=0.08).
Conclusions: MRI and image fusion targeted prostate biopsy is associated with an improved concordance and a lower rate of histopathological upgrading from biopsy to RP specimen.
AS-6.067
Membranous urethral length and prostate volume on MRI and continence rates after radical prostatectomy
Nolsøe A, Løgager V1, Jakobsen H2, S. F. Jensen C2, Busch Østergren P2,3, Henrik Bruun N4, Boesen L2,3, Sønksen J2,3, Fode M2,3
1Copenhagen University Hospital, Herlev and Gentofte Hospital, Deparment og Radiology, Herlev, Denmark, 2Copenhagen University Hospital, Herlev and Gentofte Hospital, Department of Urology, Herlev, Denmark, 3University of Copenhagen, Department of Clinical Medicine, Copenhagen, Denmark, 4Aalborg University Hospital, Unit of Clinical Biostatistics, Aalborg, Denmark
Background: We aimed to investigate if preoperative bi-parametric prostate MRIs were predictive of post-operative urinary incontinence (UI) in patients undergoing non-nerve-sparing or unilateral nerve-sparing Robot-Assisted Radical Prostatectomy (RARP).
Methods: Bi-parametric MRI scans were performed preoperatively on 100 continent patients, from December 2018 to June 2022. The membranous urethral length (MUL) was measured in the sagittal plane in cm and as the number of image slices (3 mm/slice), while the prostate volume was calculated. Urinary function was evaluated by the International Consultation on Incontinence Questionnaire (ICIQ-SF), daily pad use, and a 24-hour pad test. Continence was defined as the answer “never” to the ICIQ-SF question: “How often do you experience urinary incontinence?” and the use of 0 pads or a urine loss of less than 8 grams on the 24-hour pad test. Regression with robust variance estimates was used to analyze the predictive power of MRI measurements on outcomes.
Results: Data from 82 patients were available for final analysis. The mean age was 67 years (SD 5.9). At 12 months the mean ICIQ-SF score was 5.5 (SD 5.2) while 63% (n=52) were continent. Mean MUL was 1.58 cm (SD 0.4) and 4.8 slices (SD 1.5), respectively. The mean prostate volume was 43.5 ml (SD 16). A shorter MUL measured in cm was not significantly associated with ICIQ-SF score (p=0.09), but it was associated with UI (RD 26% per cm, p=0.03). Shorter MUL measured in slices was associated with an increase of 0.76 points in the mean ICIQ-SF score per slice (p=0.05). There was a trend towards it being significantly associated with UI (RD 7% per slice, P=0.06). Prostate volume was not associated with the ICIQ-SF score (P=0.19), but a larger prostate volume increased the risk of UI by 1% per ml (p<0.01).
Conclusions: Our study highlights the potential of preoperative bi-parametric MRI measurements in prediction of UI after RARP.
AS-6.068
Functional outcomes and patient satisfaction after low-dose rate brachytherapy for localized prostate cancer
Beji S, Nolsøe A B, Jensen C F S, Oestergren P B, Sønksen J, Bisbjerg R, Jakobsen H, Nørgaard N, Fode M
Copenhagen University Hospital, Herlev and Gentofte Hospital, Department of Urology, Herlev, Denmark
Background: To investigate erectile dysfunction (ED), urinary incontinence (UI), and patient satisfaction after Low-Dose Rate Brachytherapy (LDR-B) for localized prostate cancer.
Methods: Questionnaire study in men who underwent LDR-B at Herlev Hospital from 2010 to 2020. The questionnaire included the Erection Hardness Scale (EHS), the International Consultation on Incontinence Questionnaire (ICIQ-SF), and questions on expectations and treatment satisfaction.
Results: Responses from 178/389 men were available for analyses (46%). The median age was 70 (range 51-83) years, and the median time since LDR-B was 93 (21-141) months. Before LDR-B, the median EHS was 3 (0-4) with 36 men (20%) suffering from ED and 26 (14.6%) taking PDE5-Is. 14 men (8%) suffered from UI. At the time of the survey, 142 men were sexually active with 51 (36%) receiving ED treatment. The median EHS was 3 (0-4) and 107 (75%) men were capable of penetration. 66 (37%) had UI. For 45 of these, it was once a week or less and 63 lost a small amount of urine. The median ICIQ-SF score in men with UI was 4.5 (1 – 20). On multivariate analysis, pre-treatment ED and UI predicted the same issues following LDR-B (p=0.008 and p=0.0003, respectively). Satisfaction with LDR-B was reported by 161 (90%). Sexual and urinary function lived up to the expectations for 98 (56%) and 142 (80%) respectively. Continent men were most likely to be satisfied (OR 4.160, 95% CI 1.38 - 12.6, p=0.01), while there was no correlation between ED and satisfaction (p=0.3). However, men were more likely to be satisfied if sexual function lived up to their expectations (OR 3.021, 95% CI 1.003 - 9.102, p=0.049), and if urinary function lived up to their expectations (OR 9.0, 95% CI 3.0 – 27.0, p=0.014).
Conclusions: The risk of UI and ED following LDR-B is limited and most men are satisfied with the treatment. Correspondence between pre-treatment expectations and actual functional outcomes is the strongest predictor of satisfaction.
AS-6.069*
Overall quality of life and treatment-related side-effects in older prostate cancer survivors, a cross-sectional study
Sletten R1,2,3, Berger Christiansen O2,4, Slaaen M2,5, Oldervoll L M3,6, Åstrøm L7, Kjesbu Skjellegrind H8,9, Šaltytė Benth J2,10,11, Kirkevold Ø2,12,13, Bergh S2,13, Grønberg B H14,15, Rostoft S5,16, Bye A17, Mork P J3
1Innlandet Hospital Trust, Department of Oncology and Centre for Palliative Care, Gjøvik, Norway, 2Innlandet Hospital Trust, The Research Center for Age-Related Functional Decline and Disease, Hamar, Norway, 3Norwegian University of Science and Technology, Department of Public Health and Nursing, Faculty of Medicine and Health Sciences, Trondheim, Norway, 4Innlandet Hospital Trust, Unit of urologic surgery, Hamar, Norway, 5University of Oslo, Institute of Clinical Medicine, Faculty of Medicine, Oslo, Norway, 6University of Bergen, Centre for Crisis Psychology, Faculty of Psychology, Bergen, Norway, 7Uppsala University, Section of clinical and experimental oncology, Department of Immunology, Genetics and Pathology, Uppsala, Sweden, 8Norwegian University of Science and Technology, HUNT Research Centre, Department of Public Health and Nursing, Faculty of Medicine and Health Sciences, Levanger, Norway, 9Nord-Trøndelag Hospital Trust, Levanger Hospital, Levanger, Norway, 10University of Oslo, Institute of Clinical Medicine, Campus Ahus, Oslo, Norway, 11Akershus University Hospital, Lørenskog, Health Services Research Unit, Lørenskog, Norway, 12Norwegian University of Science and Technology, Faculty of Health, Care and Nursing, Gjøvik, Norway, 13The Norwegian National Centre for Ageing and Health, Tønsberg, Norway, 14Norwegian University of Science and Technology, Department of Clinical and Molecular Medicine, Trondheim, Norway, 15St. Olavs Hospital, Trondheim University Hospital, Department of Oncology, Trondheim, Norway, 16Oslo University Hospital, Department of Geriatric Medicine, Oslo, Norway, 17Oslo Metropolitan University, Oslo, Norway
Background: There is limited knowledge on overall quality of life (QoL) in older prostate cancer survivors. We aimed to explore if age at treatment is associated with post-treatment QoL.
Methods: This is a single-center, cross-sectional study in 654 prostate cancer survivors, 3-7 years after curative treatment with robotic-assisted radical prostatectomy (RARP) or external beam radiotherapy (EBRT). QoL was measured with the European Organisation of Research and Treatment in Cancer Quality of life Questionnaire-C30 (QLQ-C30) and the Expanded Prostate Cancer Index Composite (EPIC-26). Multiple linear regression models were estimated to assess associations between age at treatment and QoL outcomes.
Results: For all QLQ-C30 function and symptom scales, there was no clinically significant differences between men who were older (> 70 years) and younger (< 70 years) at the time of treatment. We found no significant associations between age at treatment and global QoL or physical function (QLQ-C30). However, an association between older age and worse sexual (RC -0.77, p < 0.001) and better hormonal/vitality function (RC 0.30, p = 0.006) was found (EPIC-26).
Conclusions: In conclusion, age at treatment seems to have little impact on how men experience their QoL 3-7 years after radical treatment with EBRT or RARP.
*Nominee for best abstract in the field of urologic cancer
SESSION VII - ORAL PRESENTATIONS – KIDNEY
AS-7.070
Dose reduction potential of a vendor-agnostic deep learning CT reconstruction algorithm: an exploratory study of image quality in assessing small renal masses
Borgbjerg J1, Leland-try M1, Kathir A1, Longum A1, Bomer J1, Nasser S1, Nielsen T K2
1Akershus University Hospital, Radiology, Nordbyhagen, Norway, 2Aalborg University Hospital, Urology, Aalborg, Denmark
Background: The cumulative radiation dose incurred during CT-based active surveillance (AS) of small renal masses (SRMs) is a cause of concern. We aimed to investigate the dose reduction potential of a vendor-agnostic deep learning model (DLM, ClariCT.AI) compared with conventional hybrid iterative reconstruction (IR) across various CT dose levels.
Methods: Seven patients underwent contrast-enhanced CT in the portal venous phase of the abdomen as part of AS of a SRM. Images were obtained with Philips CT systems using iDose (IR). Based on these standard-dose CT images, three sets of low-dose (LD) IR images corresponding to a 50, 75, and 90% dose reduction were generated using a validated LD simulation technique. Three additional LD CT image sets were generated where the DLM was applied. Qualitatively, the images (n=49) were reviewed by five radiologist readers in a blinded, randomized fashion using a 5-point Likert scale. For each image, readers evaluated the overall image quality, image noise, and diagnostic confidence in delineating the contour of the SRM. Quantitatively, image noise was measured in a circular region of interest in the abdominal aorta at the level of the SRM.
Results: As seen in Table 1, quantitatively, the DLM demonstrated more than a twofold noise reduction across dose levels compared to IR. With respect to qualitative assessment, DLM LD-90% images were rated comparable to IR LD-50% images, and DLM-75% images were rated similar to IR standard-dose.
Conclusions: Our results suggest a potential for significant dose reduction in AS of SRMs and provide parameters to be used in further contextualization (e.g., evaluation of SRM size assessment reproducibility) in future studies employing a greater number of CT cases and readers.
AS-7.071*
Active Surveillance for Small Renal Masses: Living with a potential untreated cancer
Bak R1, Jensen J B1, Pelant T2, Haase R N3, Zachariae R4, Nielsen T K1,3
1Aarhus University Hospital, Department of Urology, Aarhus, Denmark, 2Regional Hospital Gødstrup, Department of Urology, Gødstrup, Denmark, 3Aalborg University Hospital, Department of Urology, Aalborg, Denmark, 4Aarhus University, Department of Psychology and Behavioural Sciences, Aarhus, Denmark
Background: Small Renal Masses (SRMs) are often benign lesions or early-stage cancers with a very limited metastatic potential. The risk of overtreating of SRMs is a particular concern in elderly or comorbid patients, for whom the risks associated with active surveillance (AS) is lower than the risk and benefits of surgical management. However, the knowledge regarding patient selection, long-term oncological outcomes and psychological side effects of AS is still limited.
Methods: 401 patients in AS between January 2012 and Marts 2023 at three Danish urology centers were retrospectively identified and classified into three groups: AS (n=201), delayed intervention (DI) (n=47), and terminated AS (n=153). The possible concern associated with AS was investigated using an adjusted Fear of Cancer Recurrence Inventory-Short Form (FCRI-SF) survey in the AS cohort and compared to the fear of cancer recurrence in cryoablation patients treated in 2021 and 2022. The survey analysis included 141 AS and 83 cryoablation patients.
Results: Mean age for the three groups was 71, 68, and 76 yr (p<0.001), mean initial tumour size was 16, 19, and 21 mm (p<0.001), and mean growth rate (GR) was 0.5, 4.8 and 1.1 mm/yr (p<0.001) One patient metastasised under AS. The survey analysis showed no different FCRI-SF score between AS and cryoablation patients (10.9 vs 10.2, p=0.52). The cryoablation patients were younger (67 vs 71 yr, p<0.001) and had a greater tumour size (23 vs 15mm, p<0.001) compared to AS patients. The AS subgroup analysis showed a higher FCRI-SF score for patients <72 years compared to older patients (12.1 vs. 9.7 points, p=0.039).
Conclusions: Age and tumour size were lower for AS and DI patients compared to terminated patients. Mean GR was higher for DI patients. The FCRI-SF survey analysis showed no additional anxiety associated with AS in relation to fear of cancer progression compared to cryoablation patients. Patients <72 years had a higher FCRI-SF score indicating more psychological affection being in an AS program.
*Nominee for best abstract in the field of urologic cancer
AS-7.072
Real world management of oncocytomas diagnosed by renal mass biopsy (RMB)
Nordanger I M1, Almås B1, Akhtar S N1, Æsøy M S1, Beisland C1,2, Hjelle K M1,2
1Haukeland University Hospital, Department of Urology, Bergen, Norway, 2University of Bergen, Department of Clinical Medicine, Bergen, Norway
Background: The optimal treatment of oncocytomas is still under debate. The aim of this study was to assess the outcome of patients diagnosed with oncocytic neoplasm by RMB and evaluate if non-intervention (NoI) with active surveillance (AS) and watchful waiting (WW) have been oncologically safe.
Methods: Retrospective registration of RMB from 2008-2022 detected 71 patients with oncocytic neoplasm. Data were obtained by reviewing medical records as part of a clinical audit and is exempt from requirement of ethical approval. Logistic regression analyses were performed to assess potential predictors for surgery.
Results: Median age at diagnosis was 74 (IQR 67-79) years. Three patients underwent immediate surgery while 68 patients were managed with NoI. 39 were in AS with follow-up (FU) at the outpatient clinic, while 27 had WW only. Two patients had metastatic renal cancer, despite a finding of oncocytoma at RMB. Median FU was 44 (IQR 22-68) months. Conversion from NoI to surgery occurred in 7 cases. Patients who underwent surgery were significantly younger than those in NoI (Median 67 vs 74 years, p<0.03). Histopathology was conclusive for oncocytomas in 61 (86%) patients. Five of these underwent surgery, with one malignancy. The pathologist expressed doubt about the diagnosis in ten patients, of whom five underwent surgery with three having cancer in the surgical specimen. Overall, final histology after surgery showed 60% oncocytomas, 30% chromophobe and 10% papillary tumours. No patients died due to delayed surgery, and no patients developed metastases. Indication for surgery was tumour growth (n=4), malignant re-biopsy (n=1) or uncertain histology (n=5). All patients operated due to tumour growth showed oncocytoma in the final report. Uncertain histology was a significant predictor for surgery (OR 13.2, p=0.003), comorbidity and tumour size were not.
Conclusions: Surveillance of RMB oncocytoma is a safe oncological option, careful consideration of the histopathology is important when treatment choice is made.
AS-7.073
Percutaneous Image-guided Cryoablation of Endophytic Renal Cell Carcinoma
Junker T1,2, Greve Jensen C1, Dybdahl M1, Valtersson J1, Mussmann B1,2, Aarup Duus L1, Pietersen P I1,2, Lund L2,3, Welch B4, Graumann O1,2
1Odense University Hospital, Research and Innovation Unit of Radiology, Odense, Denmark, 2University of Southern Denmark, Department of Clinical Research, Odense, Denmark, 3Odense University Hospital, Department of Urology, Odense C, Denmark, 4Mayo Clinic, Department of Radiology, Rochester, MN, United States of America
Background: Treatment of endophytic renal cell carcinoma (RCC) stage cT1 is a challenge. Due to difficulties in visualizing tumor tissue during nephron-sparing surgery, image-guided percutaneous cryoablation (PCA) is an attractive alternative. The minimally invasive nature of PCA makes it favorable for patients with comorbidities and patients in which nephrectomy is contraindicated. The purpose of this study was to access oncological outcome and complications after PCA of endophytic biopsyproven RCC.
Methods: This was a retrospective study. Patients treated with PCA at Odense University Hospital, Denmark, from January 2015 to November 2021 were eligible for inclusion. Inclusion criteria were biopsy-proven RCC stage cT1 and 100% endophytic tumor localization treated with PCA with at least one year of follow-up. The oncological outcome was categorized into two; incomplete ablation, defined as an enhancement in the ablation cavity detected or suspected at three months follow-up, or local recurrence, defined as an enhancement in the ablation cavity after the initial follow-up showed no residual tumor. Complications were reported according to the Clavien-Dindo classification within one year after treatment.
Results: A total of 56 patients with 56 endophytic tumors were included. The treated tumors had a median RENAL score of 9 (IQR 2), and a mean tumor size of 25.7 mm (SD 8.9). The mean follow-up was 996 days (SD 559). Four patients (7%) had incomplete ablation and four had recurrence (7%) No patients progressed to metastatic RCC within the follow-up period. Major complications (grade ≥ 3) occurred in three patients (5.4%). The major complications were two cases of iatrogenic pneumothorax, treated within the procedure, and one patient with cardiac arrest after extubating, all discharged in their habitual state.
Conclusions: This study found that PCA of endophytic RCC cT1 is safe with few incomplete ablations and major complications. Four patients had biopsy proven recurrence, but none developed metastatic disease.
AS-7.074
Salvage cryoablation: are some tumors untreatable with cryoablation?
Støttrup M S1, Lagerveld B2, Keeley Jr F X3, Breen D J4, King A4, Strijen M v5, Graumann O6, Kerviler E d7, Alcorn D8, Borgbjerg J9, Zondervan P10, Wah T M11, Nielsen T K1,12
1Department of Urology, Aarhus University Hospital, Aarhus, Denmark, 2Department of Urology, OLVG, Amsterdam, The Netherlands, 3Bristol Urological Institute, Bristol, United Kingdom, 4Department of Radiology, Southampton University Hospitals, Southampton, United Kingdom, 5Department of Radiology, St. Antonius Hospital, Nieuwegein, The Netherlands, 6Department of Radiology, Odense University Hospital, Odense, Denmark, 7Radiology Department, Saint-Louis Hospital, Paris, France, 8Department of Interventional Radiology, Gartnavel General Hospital, Glasgow, United Kingdom, 9Department of Radiology, Akershus University Hospital, Oslo, Norway, 10Department of Urology, Amsterdam UMC, Amsterdam, The Netherlands, 11Department of Diagnostic and Interventional Radiology, Institute of Oncology, St. James’s University Hospital, Leeds, United Kingdom, 12Department of Urology, Aalborg University Hospital, Aalborg, Denmark
Background: Renal cryoablation has a high success rate in treating tumors, with less than 5% of patients experiencing residual unablated tumors or late local recurrence. However, there are currently no widely accepted standards or recommendations for salvage treatment in these cases. While the tumor is typically small and salvage ablation is feasible, limited data exist regarding the outcome of repeated cryoablation. The present study aims to evaluate the efficacy of salvage cryoablation following failure of initial cryoablation in patients with small renal masses (SRMs).
Methods: A total of 116 patients with sporadic T1N0M0 SRMs who failed initial cryoablation and were retreated with salvage cryoablation were identified from 14 European institutions within the European Registry for Renal Cryoablation (EuRECA) and included for this retrospective analysis of efficacy.
Results: A total of 70 patients (62.5%) remained disease-free with a median follow-up time of 21 months (95% CI: 16-25) after salvage cryoablation. The highest success rates of salvage cryoablation were found in patients treated with either 3D-cone CT (71.4%) or conventional CT-guided (68.1%) cryoablation. Laparoscopic and ultrasound-guided procedures showed the lowest success rates, with 47.6% and 25%, respectively. Available covariates (age, BMI, tumor size, and initial failure type) did not significantly predict the outcome of salvage cryoablation.
Conclusions: While salvage cryoablation is technically feasible, its success rate is lower than what is known from initial cryoablation. When planning salvage treatment, it’s important to discuss this aspect with the patient. The reasons for this discrepancy are not well understood and require further investigation.
AS-7.075
The implementation of robotic surgery for renal tumors significantly reduces the number of radical nephrectomies
Müller S1,2, Skogen I1, Kongsrud T1, Nilsen F S1
1Akershus University Hospital, Department of Urology, Lørenskog, Norway, 2University of Oslo, Institute of Clinical Medicine, Oslo, Norway
Background: Minimal invasive surgery has obvious advantages compared to open surgery. Since 2009, laparoscopic technique has been our preferred method for renal surgery. We implemented robotic surgery at our department in 2018. Although robotic surgery increases costs, the technical potential of robotic surgery has made it our preferred method for renal surgery, particularly for partial nephrectomy. We have compared peroperatve outcomes of laparoscopic and robot-assisted partial nephrectomy for renal tumors performed at our institution.
Methods: Analysis of data from our Institutional Review Board approved database with consecutive patients undergoing surgery for renal tumors. Peroperative outcomes from 2015-2017 (laparoscopic surgery) and 2020-2022 (robot-assisted surgery) were compared. In the laparoscopic group, 14 patients that underwent a combination of laparoscopic and open access were excluded. Conversions from partial to radical nephrectomy were excluded in both groups.
Results: The results are presented in the table. Most outcomes are comparable between the groups. Median length of stay was reduced by one day and tumor complexity was higher in the robotic group. During the robotic period, the number of radical nephrectomies fell drastically resulting in a proportion of partial nephrectomy of 79% of our total renal tumor surgery volume.
Table: Peroperative outcomes of Laparoscopic and Robotic renal surgery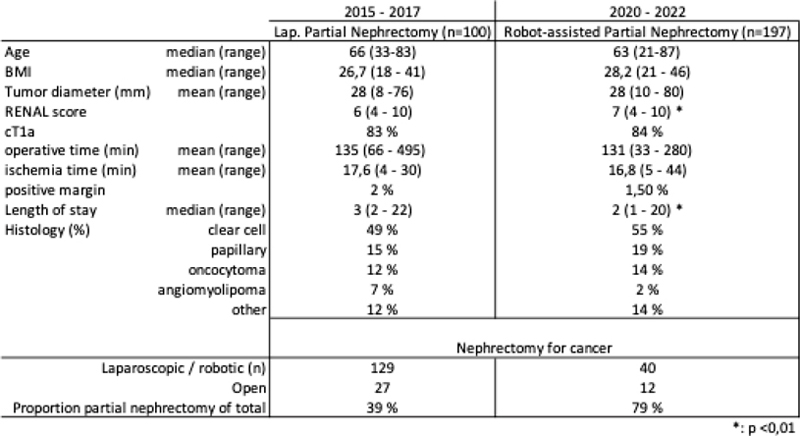
Conclusions: The implementation of robotic surgery has led to a change of practice in our department. A significant higher proportion of patients can be offered nephron-sparing surgery with the advantages of minimally invasive surgery.
AS-7.076
What is the optimal surgical treatment of patients with clinical T1b renal cell carcinoma - histopathological upstaging, recurrence, and survival in a national population-based cohort
Ljungberg B1,2, Lundstam S3, Karlsson Rosenblad A4,5, Ljungberg B1,2
1Umeå University Hospital, Department of Urology, Umeå, Sweden, 2Umeå University, Department of surgical and perioperative sciences, Urology and andrology, Umeå, Sweden, 3Sahlgrenska Academy, Departments of Urology, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden., Göteborg, Sweden, 4Regional Cancer Centre Stockholm-Gotland, Region Stockholm, Stockholm, Sweden, Regional Cancer Centre Stockholm-Gotland, Stockholm, Sweden, 5Department of Medical Sciences, Division of Clinical Diabetology and Metabolism, Uppsala University, Uppsala, Sweden, Division of Clinical Diabetology and Metabolism, Uppsala, Sweden
Background: Patients withT1 renal cell carcinoma (RCC) generally have a good prognosis. Partial nephrectomy (PN) is recommended when technical feasible also for T1b RCC. Despite a favorable prognosis there remains a risk for upstaging and recurrence, and the place for PN in clinical T1b tumors is questionable. We have therefore characterized clinical and morphological variables including histopathological upstaging, disease recurrence, and overall survival (OS) in a national real-world population-based cohort.
Methods: Patients without metastases registered in the National Swedish Kidney Cancer Register (99% of RCCs diagnosed in Sweden) 2005-2014 with clinical T1b (4-7cm), being surgically treated and having 5 years follow up time, were included.
Results: There were 2137 patients, 1300 males and 837 females with a mean age of 66 years, 82% had clear cell (ccRCC), 11% papillary (pRCC) and 6% chromophobe (chRCC). Radical nephrectomy (RN) was done in 1836 patients and PN in 301 patients. After histopathological examination, 435 (20%) of the cT1b RCC were upstaged to pathological T3 stage, 21% ccRCCs, 13% pRCC and 20% chRCCs. Recurrent disease within a 5-years follow-up time was diagnosed in 29% (127) of patients with pT3 and in 14% (238) of patients with pT1b. Of these 322 (18%) patients had ccRCC, 127 (11%) pRCC and 5% had chRCC. Lung was the most common recurrence site 52 % and 144 (39%) of the patients had two or more metastatic sites. Patients with pT3RCC had a 67% 5-year OS compared to 83% in pT1b (p<0.001). In multivariable analyses lower age, female sex, tumor size, T-stage, N-stage, and RCC-type all significantly associated with OS time. A hazard ratio 0.93 CI [0.65-1.32] for PN showed that PN was non-inferior to RN in patients with cT1b RCC.
Conclusions: Clinical T1bRCC is a malignant disease with risk for upstaging and tumor recurrence. Nonetheless the results show that PN was non-inferior to the treatment with RN and support the recommendation to offer PN in patients with cT1bRCC.
AS-7.077
Survival after lymph node dissection in Conjunction with Nephrectomy as treatment for stage III Renal Cell Carcinoma – a Danish nation-wide, retrospective cohort study
Nadler N1,2, Mosholt K S S3, Geertsen L4,5, Axelsen S S6, Christensen J7, Jensen N V8, Fristrup N6, Dalton S O7,9, Donskov F10, Lund L4,5, Azawi N1,2
1Zealand University Hospital, Department of Urology, Roskilde, Denmark, 2University of Copenhagen, Department of Clinical Medicine, Copenhagen, Denmark, 3Rigshospitalet, Department of Urology, Copenhagen, Denmark, 4Odense University Hospital, Department of Urology, Odense, Denmark, 5University of Southern Denmark, Institute of Clinical Medicine, Odense, Denmark, 6Aarhus University Hospital, Department of Oncology, Aarhus, Denmark, 7Danish Cancer Society, Copenhagen, Denmark, 8Odense University Hospital, Department of Oncology, Odense, Denmark, 9Zealand University Hospital, Department of Clinical Oncology & Palliative Care, Næstved, Denmark, 10Southern Denmark University Hospital, Department of Oncology, Esbjerg, Denmark
Background: The management of renal cell carcinoma (RCC) through lymph node dissection (LND) remains a topic of ongoing debate. The objective of this study was to investigate the impact of LND on both overall survival (OS) and recurrence-free survival (RFS) in patients with stage III RCC.
Methods: The study utilized a retrospective cohort design and included 501 patients with stage III RCC listed in the Danish Renal Cancer Registry (DaRenCa) between 2014 and 2016. The intervention involved lymph node dissection in conjunction with nephrectomy. Patient demographics, clinical and histopathological features were evaluated. Cox regression analysis was performed for OS and RFS. Two models were introduced to adjust for pathological and clinical features. Model 1 adjusted for age, gender, tumor stage, tumor size, Fuhrman grade, necrosis, and sarcomatoid component. Model 2 further adjusted for BMI, symptoms, smoking, hypertension, ASA score, performance status, and MDT decision. Results were reported at 95% confidence intervals (CIs) and p-values ≤0.05.
Results: Out of the 501 patients with stage-III RCC, 95 (19%) underwent LND, and 32 (34%) had positive lymph nodes (pN1). The one-year mortality hazard ratios were 0.23 (0.04–1.32) in model 1 and 0.20 (0.04–1.04) in model 2 for patients who underwent LND. The RFS for patients who underwent LND was 1.48 (0.96–2.28) in model 1 and 1.42 (0.90–2.25) in model 2. Limitations include the absence of a standard template for LND, retrospective cohort data, and potential selection bias. Strengths are combined national registry data and medical record reviews.
Conclusions: This study suggests that LND may provide a survival advantage for patients with stage III RCC, as demonstrated by lower one-year mortality hazard ratios. However, the results did not reach statistical significance in either of the two models used. Further research with larger sample sizes and longer follow-up periods is necessary to determine the significance of LND in the management of stage III RCC.
AS-7.078
Neoadjuvant effects in a randomized phase 2 study with a cell-based immune primer plus sunitinib versus sunitinib alone in patients with metastatic Renal Cell Carcinoma
Ljungberg B1,2, Lindskog M3,4, Karlsson-parra A5, Ljungberg B1,2
1Umeå University Hospital, Department of Urology, Umeå, Sweden, 2Umeå University, Department of surgical and perioperative sciences, Urology and andrology, Umeå, Sweden, 3Uppsala University, Department of Immunology, Genetics and Pathology,, Uppsala, Sweden, 4Karolinska Institutet, Department of Oncology,, Stockholm,, Sweden, 5Uppsala University, Department of Immunology, Genetics and Pathology, Section of Clinical Immunology, Uppsala, Sweden
Background: The prognosis for patients with synchronous metastatic renal cell carcinoma (mRCC) remains poor. Despite improvements with single agent tyrosine kinase inhibition (TKI) and additionally clinical gains by immune checkpoint inhibitor (ICI) combinations, the treatment effects remain deficient.
Methods: 88 patients with synchronous mRCC, were included in a randomized (2:1) phase 2 multicenter study to the treatment either with a combination of two doses of allogeneic monocyte-derived dendritic cells (ilixadencel) and sunitinib (ILIXA/SUN) (58 patients) or with sunitinib only (SUN) (30 patients) and nephrectomy. The ilixadencel was administrated intratumorally two weeks apart, followed by nephrectomy and sunitinib. Primary endpoints were 18-month survival rate and overall survival (OS). A secondary endpoint was objective response rate (ORR). Statistic evaluations included Kaplan-Meier, log-rank tests, Cox regression and stratified Cochran–Mantel–Haenszel tests.
Results: Median OS was 35.6 months in the ILXA/SUN arm versus 25.3 months in the SUN arm (HR 0.73, 95%CI:0.42-1.27), while the 18-month OS rate was 63% and 66% in the ILIXA/SUN and SUN arms, respectively. ORR in ILIXA/SUN arm was 42.2% (19/45), including 3 patients with complete response (CR), versus 24.0% (6/25) in the SUN arm (p=0.13) without any CR. At the last scheduled imaging follow-up at 18 months two additional patients in the ILIXA/SUN arm (total 5 of 45 = 11%) had developed CR and one in the SUN arm (1/25). All 5 ILIXA/SUN CR patients were alive at the latest survival follow up, while the SUN CR patient had died.
Conclusions: The study failed to meet primary endpoints. However, neoadjuvant ilixadencel in combination with sunitinib, associated with a numerically higher response rate, including longstanding CRs, as compared with sunitinib, suggesting an immunologic effect of the experimental treatment.
AS-7.079
Prediction of clinically significant recurrence after partial nephrectomy. Data from the Cancer Register of Norway and more than 5 years follow up
Pedersen E1, Barniou O1, Johannesen T B2, Diep L M3, Hjelle K4, Beisland C5
1Sørlandet Sykehus, Kristiansand, Norway, 2Kreftregisteret i Norge, Oslo, Norway, 3Oslo Universitetssykehus, OCBE, Oslo, Norway, 4Haukeland Sykehus, Urologisk avdeling, Bergen, Norway, 5Haukeland Sykehus, Bergen, Norway
Background: The purpose of the study was to determine the incidence of recurrence after partial nephrectomy (PN) and to find a prediction model for local recurrence and metastasis.
Methods: We retrospectively evaluated a cohort of 524 PN patients from the Cancer Registry of Norway, operated between January 2014 and December 2015 with more than 6 years of follow-up. Patient demographics and pathological characteristics were correlated with recurrence and progression free survival using Kaplan-Meier and Cox regression analyses.
Results: We recorded a median patient age of 64 and a median tumor size of 2.6 cm. Overall, 85.1% of tumors were stage pT1a, 70% were clear cell type and a nucleolar grad 2 was registered in 60% of the patients. A 42% of the patients were operated robot-assisted and 67.3% in an intermediate- or high-volume hospital. We found 11.5% positive surgical margins (PSM) and a 3.4% and 3.2% rate for local recurrence and metastasis, respectively. PSM (HR 55.4, 95% CI 12.55-244.6), tumor number (HR 45.4, 95% CI 6.5-316.1) and stage (HR 33.5, 95% CI 5.4-205.3) were independent predictors for local recurrence. Undetermined margins’ status was found to be a risk factor for LR. Tumor stage (HR 41.05, 95% CI 8.52-197.76) was also a predictor for metastasis together with presence of tumor necrosis (HR 1.3, 95% CI 0.4-4.31) and age (HR 1.07, 95% CI 1.01-1.14).
Conclusions: Both local and distant recurrence after partial nephrectomy is rare and pT-stage is a common predictor factor. Positive or undetermined status for surgical margins and tumor multifocality are predictors for local recurrence, while age at surgery and presence of tumor necrosis predict metastasis.
AS-7.080
Predictors of renal cancer prognosis in elderly patients – a population-based cohort study
Pajunen H1, Murtola T1, Veitonmäki T1, Nikkola J1, Pöyhönen A2, Huhtala H3
1Tampere University, Faculty of Medicine and Health Technology, Tampere, Finland, 2The Finnish Defense Forces, Center for Military Medicine, Helsinki, Finland, 3Tampere University, Faculty of Social Sciences, Tampere, Finland
Background: Mortality in renal cell cancer (RCC) is high in the elderly population. However, comorbidities often impact overall prognosis among this group. It is important to know which comorbidities have most prognostic impact in elderly RCC patients to identify those who most likely benefit from curative treatments.
Methods: New RCC in people 75 years or older were collected between 1995-2018 from the Finnish cancer registry, a total of 5,357 cases. Information on comorbidities were collected from national registry. Charlson Comorbidity Index (CCI) was used to reflect comorbidity in analyses on the risk of death. The risk for RCC death and overall mortality were analyzed using Cox regression analysis. Individual prognostic role of CCI components were evaluated by multivariable Cox regression model. We constructed a nomogram to predict RCC mortality using the most important comorbidities and clinical characteristics predicting mortality.
Results: Statistically significant predictors of RCC death were tumor morphology, gender, primary operative treatment, age, primary tumor extend and CCI. The strongest predictors of overall mortality were tumor extent, tumor morphology and operative treatment. Among the components of CCI, the most prognostic variables were age at diagnosis, dementia, heart failure, kidney deficiency and male gender.
Conclusions: RCC mortality is high in the elderly population. Curative treatment in selected elderly patients is efficient and should be considered in those who can tolerate it and have only limited comorbidities. Operative treatment and patient age were the strongest predictors of survival, whereas dementia and heart failure were the conditions that had the greatest impact on survival. Our nomogram helps predict RCC-related mortality while taking in account both clinical factors and comorbidities, which facilitates treatment decisions in elderly RCC patients.
SESSION VIII - ORAL PRESENTATIONS – RECONSTRUCTIVE UROLOGY
AS-8.081
Multiple transverse incisions grafted with Tachosil in Peyronie’s disease: An ongoing, prospective, non-randomized study
Tryfonyuk L1, Castro A1, Bernal J1, Iatsyna O2, Martins F3
1Universidade de Lisboa, Hospital Santa Maria, Urology, Lisbon, Portugal, 2National Cancer Institute of Ukraine, Urology, Kiev, Ukraine, 3Universidade de Lisboa, Hospital Santa Maria, Urology, Lisboa, Portugal
Background: Peyronie’s disease (PD) can be both physically and psychologically distressing. Although invasive, surgery remains the most reliable and effective treatment option. However, complications are not negligible. We present our preliminary data of an ongoing, prospective, non-randomized study of potent patients with PD who underwent multiple transverse incisions (MTI) covered with Tachosil. Severe dorsal/dorsolateral deformity and/or further penile shortening were the primary therapeutic endpoints.
Methods: Patients with dorsal/dorsolateral deformity and stable PD were included. All patients underwent a penile duplex ultrasound study (PDUSS) and SHIM-5 (Sexual Health Inventory for Males) questionnaire to assess erectile function objectively and subjectively before and after surgery. PGI-I (Patient Global Impression of Improvement) was used to assess patient satisfaction.
Results: Between January 2018 and February 2020 29 patients underwent MTI (median 4; range 3-6) with Tachosil. Median age was 66 years (range 49-76). Median preoperative compound curvature was 60 degrees (range 30- 90), 24 had dorsal, 3 had dorsolateral and 1 lateral curvature. Total straightness was achieved in 24 patients and residual curvature was evidenced in 5. Erectile rigidity sufficient for penetrative intercourse was maintained in all patients at last follow-up, not displaying erectile dysfunction progression. There were no significant changes in PDUSS scores. SHIM-5 scores improved from 13 (range 12-16) to 19 (range 18-21). Median postoperative PGI-I scores were 2 (much better). No penile length reduction was observed. One patient experienced self-limiting penile hematoma, 5 patients noted transient glandular hypoesthesia with 1 developing prolonged sensation impairment.
Conclusions: MTI with Tachosil grafting is feasible, well tolerated, easy and quick to perform for PD. It avoids creation of large tunical defects with subsequent veno-occlusive dysfunction and provides additional hemostasis, while preserving erectile function.
AS-8.082
Dorsolateral Approach For buccal mucosal Graft Urethroplasty In Long segment anterior Urethral Stricture
Abdelghfour A T
Zagazig university, Department of Urology, Zagazig, Egypt
Background: Evaluation of the results of dorsolateral buccal mucosal augmentation urethroplasty in patients with long- segment anterior urethral strictures.
Methods: This prospective study included 76 patients with anterior urethral strictures. Inclusion criteria were: non traumatic non-obliterative anterior urethral strictures more than 2 cms long who were scheduled for (BMG) urethroplasty. Preoperative IPSS IIEF scores were filled by the patients and Uroflowmetry was done for all patients. Patients were followed for a minimum of one year after urethroplasty (3, 6 and 12 months). Both urethroplasty and sexual outcomes were evaluated.
Results: Mean age of the patients was 44.16±13.55 years. Mean length of the urethral stricture was 6.53±1.69. Mean duration of operation was 142.0±6.61 minutes. The mean Qmax preoperative was 6.6±1.7, and the mean Qmax at 3m, 6m, and 1y post operative was 22.4±2.17, 21.12±2.33, 20.08±2.12. The mean IPSS score preoperative was 25.84±2.01, and the mean IPSS score at 3m, 6m, and 1y post operative was 5.04±1.01, 4.64±1.23, 4.79±1.19. The mean IIEF score preoperative was 27.82±1.66, and the mean IIEF score at 3m, 6m, and 1y post operative was 24.6±1.67, 26.88±1.86, 26.5±1.22. Six patients developed recurrent urethral stricture. Four patients were corrected by VIU and included in the dilatation program. Two patients needed redo Urethroplasty. Five patients had wound infection that was managed conservatively.
Conclusions: Dorsolateral buccal mucosal augmentation urethroplasty is a surgical option that can be used in the treatment of long segment anterior urethral strictures with high success and low complication rates.
AS-8.083
Female urethral stricture: Still an underestimated and neglected entity?
Tryfonyuk L1, Iatsyna O2, Bernal J1, Martins F3
1Universidade de Lisboa, Hospital Santa Maria, Urology, Lisbon, Portugal, 2National Cancer Institute of Ukraine, Urology, Kiev, Ukraine, 3Universidade de Lisboa, Hospital Santa Maria, Urology, Lisboa, Portugal
Background: Female urethral stricture (FUS) is considered relatively uncommon. It is associated with an important financial cost and potentially debilitating outcomes. Understanding its epidemiology is critical to identify risk factors to produce better treatment outcomes and quality of life, and simultaneously reducing costs. Objective: Compare patients undergoing surgical repair vs repeat urethral dilatation (UD) for FUS.
Methods: A retrospective multicenter study of patients treated for FUS was done. We compared patients treated with UD only (G1) with patients who underwent urethroplasty (G2). Patients were evaluated with AUA Symptom Score (AUA-SS and AUA-QoL), Urogenital Distress Inventory (UDI-6), maximum flow rate (Qmax), postvoid residual (PVR), voiding cystourethrogram, and urethroscopy.
Results: We included 97 patients treated for FUS 2008-2020, 80 in G1 and 17 in G2. Duration of symptoms varied from 1-9 years (mean 4.1 in G1 and 3.9 in G2). The change in AUA-SS was from 32 to 9 in G1 and from 28 to 3 in G2; Qmax increased from 3 to 30 in G1 (mean 16 ml/s), and from 4 to 49 in G2 (mean 27 ml/s). AUA-QoL score decreased after treatment from 6 to 2 in G1 and from 6 to 0 in G2. UDI-6 changed from 53.5 to 31.7 in G1 (mean 37, and 57.6 to 22.3 in G2 (mean 44). Overall urethral patency rate (allowing passage of 16F catheter) was 51% for G1 and 85% for G2 after first 6 months following respective procedures.
Conclusions: Despite lack of solid scientific evidence supporting UD in FUS, it is still common, and many urologists find it a useful tool in treating FUS. However, urethroplasty is a safe, apparently less costly, and effective therapeutic option for FUS, providing better long-term QoL Therefore, urethroplasty should be considered over UD in the majority of clinical circumstances.
AS-8.084
Novel treatment of recurrent bulbar urethral stricture – The Scandinavian experience with Optilume DCB
Holm H V1, Haase R N2, Reus C3
1Oslo University Hospital Rikshospitalet, Dept of Urology, Oslo, Norway, 2Aalborg University Hospital, Dept of Urology, Aalborg, Denmark, 3Karolinska University Hospital, Dept of Urology, Stockholm, Sweden
Background: Mechanical dilation and direct vision internal urethrotomy (DVIU) are the most widely utilized treatments for urethral stricture. Although first-time endoluminal therapy has about 50% success rate, repeat treatment is rarely successful long-term and recurrence rates approach 100%. Patients with recurrent bulbar strictures treated with Optilume® paclitaxel-coated balloon have previously shown significant improvement in symptomatic and functional outcomes through 4 years post treatment (ROBUST I). The Scandinavian experience from three centres (Oslo, Stockholm, Aalborg) with up to one-year follow-up will be presented.
Methods: Men with urethral strictures treated with Optilume drug-coated balloon (DCB) were included. Pre-treatment evaluation and follow-up differed somewhat between the three centres. All patients were diagnosed with urethrography or urethrocystoscopy. Most patients had a free uroflowmetry pre-treatment and at each follow-up. Two centres also used validated questionnaires (IPSS-2, USS-PROM, IIEF-5). The primary safety endpoint was serious urinary adverse events. The primary efficacy endpoint was the proportion of stricture free patients. Secondary outcomes included quality of life, freedom from repeat intervention, erectile function, flow rate, and post-void residual volume.
Results: A total of 51 men were enrolled and treated; most had a recurrent bulbar stricture ≤ 3 cm with ≥1 prior endoscopic treatment or urethroplasty and of unknown aetiology (idiopathic), few of traumatic or iatrogenic aetiology. Baseline characteristics included age of median 44 (range 18-79), number of prior treatments of median 2 (range 0-7), and stricture length of median 15 mm (range 1-100). There were no serious adverse events related to the treatment procedure and short-term follow-up. The results of their 3-12 month follow-up will be presented at NUF2023.
Conclusions: Optilume DCB is an easy and durable treatment option for patients with urethral stricture and should be considered after first recurrence.
AS-8.085
Artificial urinary sphincter in high-risk urethral scenarios: A multi-institutional study
Tryfonyuk L1, Bernal J1, Holm H V2, Fisch M3, Ludwig T A3, Angulo J4, Hofer M5, Lumen N6, Peterson A7, Brandes S8, Kurtzman J9, Simhan J10, Palma dos Reis J11, Nikolavsky D12, Loh-Doyle J13, Venkatesan K14, Sandul A11, Martins F15
1Universidade de Lisboa, Hospital Santa Maria, Urology, Lisbon, Portugal, 2Oslo University Hospital, Urology, Oslo, Norway, 3University Medical Center Hamburg-Eppendorf, Urology, Hamburg, Germany, 4Hospital Universitario de Getafe, Universidad Europea de Madrid, Urology, Madrid, Spain, 5San Antonio Urology, San Antonio, TX, Urology, San Antonio, TX, United States of America, 6Ghent University Hospital, Urology, Ghent, Belgium, 7Duke University Medical Center, Durham, NC, Urology, Durham, United States of America, 8Columbia University, New York, NY, Urology, New York, NY, United States of America, 9Columbia University, Urology, New York, United States of America, 10Fox Chase Cancer Center, Temple University, Urology, Philadelphia, United States of America, 11University of Lisbon, School of Medicine, Hospital Santa Maria, Urology, Lisbon, Portugal, 12SUNY Upstate Medical University, Urology, Syracuse, NY, United States of America, 13University of Southern California, Keck School of Medicine, Urology, Los Angeles, CA, United States of America, 14MedStar Washington Hospital Center, Georgetown University School of Medicine, Urology, Washington, DC, United States of America, 15Universidade de Lisboa, Hospital Santa Maria, Urology, Lisboa, Portugal
Background: The artificial urinary sphincter (AUS) remains the standard of care in men with severe stress urinary incontinence (SUI). The main drawback is a high complication rate leading to surgical revision, explantation, and urethral frailty. Objective: to report the impact of urethral risk factors and other patient systemic adverse features on infection-erosion rates and device survival outcomes.
Methods: A retrospective, multicentre study of men with ≥ 2 AUS explantations from 2008 to 2020. Minimum follow-up was 24 months after last explantation. Patient and disease characteristics, including comorbidities and adverse factors, leading to AUS explantation, were evaluated.
Results: Of the 184 patients identified with AUS implantations, 82 had ≥ 2 AUS explantations. All patients exhibited ≥ 1 risk factor including cardiovascular disease (N=59), current smoking (N=14), history of radiotherapy (N=40). Prior first line therapy included pelvic surgery (N=72), radical prostatectomy (N=64), TURP ± radiotherapy (N=13). Urethral stricture was present in 30 and urethroplasty done in 21. The number of AUS in each patient ranged from 2 to 5, with a median of number 2. Cause of second revision included urethral atrophy (N=6), erosion/infection (N=69), mechanical failure (N=5), other (N=2). None had osteomyelitis. Cystectomy was performed in 11 (13%) and urinary diversion in 59 patients (72%).
Conclusions: Patients following several AUS explantations with risk factors such as radiation, prior urethroplasty and other multiple urethral procedures, including AUS revisional surgery, are prone to developing a frail urethra and, therefore, are at higher risk of failing further repeated, eventually futile reconstructive attempts. Urethral stricture and vesicourethral anastomotic stenosis are two important and common issues that should be included in the discussion prior to AUS implantation for severe UI. A significant number of such patients ultimately opt for urinary diversion as a trade-off for quality of life.
AS-8.086*
Complications following urinary diversions (UD) for benign conditions- retrospective study of a 10-year cohort at a tertiary referral center, Haukeland University Hospital (HUH)
Haugland J N1, Bergesen A K1, Roth I1, Hjelle K M1,2, Beisland C1,2, Gudbrandsdottir G1,2
1Haukeland University Hospital, Urology, Bergen, Norway, 2University of Bergen, Clinical Medicine, Bergen, Norway
Background: Patients requiring UD for benign conditions is a heterogenic group. UD and cystectomy are procedures associated with high risk of complications. The aim of this study is to report short- and long-term complications after UD for benign conditions.
Methods: This retrospective cohort study includes all patients who underwent UD for benign conditions with or without cystectomy at our institution from 2013-2022. We obtained information about the primary surgery, complications and subsequent need for secondary surgical procedures from medical records for 72 patients. Comorbidity was defined by use of Charlson Comorbidity Index(CCI) and complications are scored according to the Clavien-Dindo system(CD). The study is an internal clinical audit, exempted from need for ethical approval.
Results: Median age was 61(IQR 42-71) years and male to female ratio was 1:1. Median CCI was 2(IQR 1 -4). Ileal conduit was done in 90% and continent reservoir (a.m. Lundiana) in 10%. Four patients had intraoperative complications. Overall (CD ≥2) short-term (≤30 days) complications was 64%(n=46). Major (CD ≥3a) complications occurred in 20(28%) patients. One patient died. There is a correlation between preoperative CCI and postoperative complications (r=0.294, p=0.012). Ten patients needed reoperation ≤ 30 days due to ileus (n=3), stoma ischemia (n=2), wound dehiscence (n=2), bowel leakage (n=1) and parastomal hernia (n=1). Previous radiotherapy correlates with reoperations (r=0.242, p=0.041). Median hospital stay was 10.5(IQR 8-19) days. Late complications (≥90 days) were seen in 34 patients. The most frequent complications related to UD were strictures (n=8), stoma complications (n=9) and reservoir complications (n=5). Thirteen had symptoms from native bladder, two underwent deferred cystectomy. Median follow up was 37(IQR 16-62) months.
Conclusions: Comorbidity is a risk factor for short-term postoperative complications and previous radiotherapy increases the risk of early reoperation. ~50% experience late complications.
*Winner of the First prize for best abstract in the field of benign urology
AS-8.087
Devastated urinary bladder and outlet – Norwegian patients 2008-2019
Holm H V, Nilsen O J
Oslo University Hospital Rikshospitalet, Dept of Urology, Oslo, Norway
Background: The objective of the study was to describe the outcome of patients with devastated bladder and/or outlet caused by iatrogenic injury after a diverse range of treatments in Norwegian patients.
Methods: After institutional review board approval, we did a retrospective study of patients treated with urinary diversion (UD) at OUS RH during the years 2008-2019. Only patients operated due to a devastated bladder and/or outlet caused by iatrogenic injury were included in the study.
Results: Forty-three patients were identified, previously treated for prostate cancer (PCa) (22), rectal/anal cancer (3), cervix or uterine cancer (3), TURP and/or TVP (5), tension-free vaginal tape (TVT) (3), and urethral stricture (one male, one female). Twenty-seven had received radiotherapy (RAD), either primary (18) or adjuvant (9).
Primary complications after index treatment included severe urinary incontinence (32), vesicourethral anastomosis stenosis (VUAS) post-radical prostatectomy (7/10 RAD), posterior urethral stenosis (PUS) post-TURP/TVP (1/12 RAD), severe bladder and sphincter dysfunction with urethral stricture (5 RAD), various urinary fistulas (9) and TVT erosion (3).
All but six patients had minor or major surgery (artificial urinary sphincter (AUS), removal of TVT/AUS, fistula repair, urethroplasty, incisions for VUAS/PUS, etc) before UD. Number of failed treatments after index treatment and before UD ranged from one to 20. Types of UD included continent urinary reservoir (2), continent catheterizable channel (8), and ileal conduit (33). Twenty had further complications: Stomal stenosis (6) or leakage (4), ureteral stricture (5), parastomal hernia (1), difficult CIC (1), intestinal obstruction (1), other (3). At final follow-up, all but one scored 5 on global response assessment (GRA) score and all would undergo UD again.
Conclusions: Treatment of pelvic cancers and benign lower urinary tract disorders may cause severe adverse events leading to devastated bladder and/or outlet. Urinary diversion may be warranted.
AS-8.088
Urinary diversion for the management of devastated lower urinary tract: Indications for cystectomy
Martins F1, Bernal J2, Tryfonyuk L2, Holm H V3, Simhan J4, Venkatesan K5, Fisch M6, Gomez R7, Hofer M8, Brandes S9, Horiguchi A10, Lumen N11
1Universidade de Lisboa, Hospital Santa Maria, Urology, Lisboa, Portugal, 2Universidade de Lisboa, Hospital Santa Maria, Urology, Lisbon, Portugal, 3Oslo University Hospital, Urology, Oslo, Norway, 4Fox Chase Cancer Center, Temple University, Urology, Philadelphia, United States of America, 5MedStar Washington Hospital Center, Georgetown University School of Medicine, Urology, Washington, DC, United States of America, 6University Medical Center Hamburg-Eppendorf, Urology, Hamburg, Germany, 7Universidad Andres Bello, Hospital del Trabajador, Urology, Santiago Chile, Chile, 8San Antonio Urology, San Antonio, TX, Urology, San Antonio, TX, United States of America, 9Columbia University, New York, NY, Urology, New York, NY, United States of America, 10National Defense Medical College, Urology, Tokorozawa-City, Saitama, Japan, 11Ghent University Hospital, Urology, Ghent, Belgium
Background: Devastated bladder outlet (DBO) is associated with necrosis, refractory stenosis, and intractable urinary incontinence (IUI) making reconstruction unfeasible. This study aims to characterize adverse features that make DBO patient’s candidates for cystectomy.
Methods: Patients who received some form of urinary diversion (UD) as ultimate management of severe complications resulting from primary (oncologic or benign) treatment were retrospectively identified. Outcomes measured included resolution of significant complications from primary oncologic treatments (POTs), such as rectourethral fistula (RUF) and IUI. Patients were categorized into two groups: following radiotherapy and/or other high energy-ablation treatments (HEAT) with/without surgery (G1) and following surgery alone (G2). History, UD type and need for extirpative procedures (salvage prostatectomy, cystectomy or total pelvic exenteration) were evaluated.
Results: G1 included 80 patients. Diagnosis was prostate cancer (PCa) in 76, rectal cancer (RCa) in 4. Complications of POT occurred in 78/80 patients; vesicourethral anastomotic stenosis (VUAS) in 24/80; prostatic urethral stenosis (PUS) in 11/80; bulbomembranous urethral stenosis (BMUS) in 4/80; RUF in 12/80, IUI in 27/80. Failed reconstructive attempts prior to UD were median 2.9 (range 0-15). Cystectomy was done in 29/80 (36%). G2 included 58 patients. Primary diagnosis was PCa in 14, RCa in 1, and benign disease in 43. Complications of primary surgical treatment were VUAS in 7/58; PUS in 9/58; BMUS in 4/58; RUF in 4/58; UI in 11/58; pyocystis in 6/58. Median failed reconstructive attempts prior to UD were 3.4 (range 1-14). Cystectomy was performed in 10/58 patients (17%), significantly fewer than after RT/HEAT (p=0.0144).
Conclusions: Irradiated/high energy-ablated patients have a higher risk of developing more severe complications requiring cystectomy. Benign patients undergoing UD have a significant risk of subsequent cystectomy.
AS-8.089*
Improvement in symptoms of pelvic late radiation tissue injury 6 months after Hyperbaric Oxygen Treatment – results from a prospective study
Mueller B1, Hjelle K M2, Velure G K1,3, Hauken M A3
1Helse Bergen, Haukeland University Hospital, Dpt of Occupational Medicine, Hyperbaric Medicine Unit, Bergen, Norway, 2Helse Bergen, Haukeland University Hospital, Department of Urology, Bergen, Norway, 3University of Bergen, Faculty of Psychology, Centre for Crisis Psychology, Bergen, Norway
Background: Radiotherapy for pelvic cancer leads to late radiation tissue injuries (LRTI) in 5-15%. Hyperbaric oxygen therapy (HBOT) can improve LRTI-related problems. The aim of this study was to assess changes in overall urinary and bowel function and in specific symptoms like increased frequency, leakage, bleeding and pain.
Methods: This single center prospective study included consecutive patients receiving HBOT for pelvic LRTI from august 2019 to March 2022. HBOT implied 30 treatments in a hyperbaric chamber, 1/d, 5 days /week, breathing 100% O2 for 90 min. at 2.4 atmospheres pressure. Patients answered the EPIC urinary and bowel questionnaire at baseline (BL), end of HBOT and at 6 months follow up. Lower EPIC sum scores (0-100) indicate more symptoms. Total scores <80 were taken to indicate clinical significant urinary or bowel problems. Five urinary and 6 bowel items were selected to assess single symptoms.
Results: Of 72 men and 61 women, 103 had urinary and 115 bowel total scores <80. EPIC sum scores improved significantly from BL to end of HBOT and 6 months (table). 6-months improvement-rates for individuals with the respective urinary symptoms were: Leakage 49.3% (n=37of 75), hematuria 74.3% (26/35), pain 55.4% (31/56), nocturia 50.5% (54/107), frequency 61.0% (61/100). Improved bowel symptom scores were observed in: Leakage 55.7% (34/61), diarrhea 37.4% (43/115), bleeding 55.6% (50/90), pain at defecation 51.7% (47/91), frequency of defecation 44.4% (32/72), abdominal pain 51.4% (38/74).
Conclusions: Six months after HBOT, symptoms of urinary and bowel LRTI were reduced. The most responsive urinary symptoms were hematuria, frequency and pain, and for bowel symptoms bleeding and leakage. These findings support the use of HBOT in pelvic radiation injuries.
*Nominee for best abstract in the field of urologic cancer
AS-8.090
Robotic pyeloplasty for ureteropelvic junction obstruction – experiences from Haukeland University Hospital
Lien M1, Hjelle K2,3, Almås B2, Æsøy M2,3, Ulvik Ø2,3
1University of Bergen, Faculty of Medicine, Bergen, Norway, 2Haukeland University Hospital, Helse-Bergen HF, Department of Urology, Bergen, Norway, 3University of Bergen, Faculty of Medicine, Department of Medicine, Bergen, Norway
Background: Ureteropelvic junction obstruction (UPJO) is described by a narrowing of the ureteral lumen below the renal pelvis. At Haukeland University Hospital, robotic pyeloplasty (RP) for UPJO has been performed since 2014. The aim of the study was to evaluate the results of the treatment.
Methods: Retrospective review was performed of patients undergoing RP between 2014 and 2022. Outcomes of interest included symptom relief, complication rates and renographic findings at follow-up.
Results: In total, 95 RP procedures were performed in 54 women and 41 men, with a mean age of 40 years (range: 10 – 78). Flank pain was the most frequent symptom (n = 81, 85%) followed by infection (n = 33, 35%). More than one cause indicating surgery was present in 34% of patients. Urodynamic relevant obstruction on renography was detected in 62 patients (65%) preoperatively. Anderson-Hynes pyeloplasty was performed in all patients, except for one patient who underwent lysis of adhesions around PUJ, only. Crossing vessels causing UPJO was the most frequent cause of obstruction and identified in 61 patients (64%). Mean operative time was 123 minutes (range 60 – 270 min) and varied widely between surgeons. Two patients experienced peroperative complications, one with a tear in the renal pelvis and another with a minor renal hematoma. At 3 months follow-up, 91% of the patients had symptom relief and no obstruction on renography was registered in 65%. To note, there was no significant association between improvement in symptoms after surgery and relief of obstruction on renography at follow-up, p = 0.57.
Conclusions: RP is a safe procedure with high success rate in terms of symptom relief and low peroperative complication rate. There was no association between renography finding and relief in symptoms at follow-up. Success after surgery should therefore depend on symptom relief rather than renography findings.
AS-8.091
A cohort study of renography following robot-assisted pyeloplasty for ureteropelvic junction obstruction in adults – what is the optimal use of the renography?
Alghezi A1, Hess S2, Zamani R1, Scheufen S1, Merrild J1, Madsen S1, Poulsen M1
1Hospital South West Jutland Esbjerg, urological department, Esbjerg, Denmark, 2Hospital South West Jutland Esbjerg, radiological department, Esbjerg, Denmark
Background: The use of renography for evaluation of pyeloplasty for PUJ obstruction in adults varies within the literature. In this study, we aim to describe the drainage and functional outcome by the renography with the goal of determining the optimal use of the renography, when performing pyeloplasty.
Methods: Between 2019 and 2022, we assessed the drainage and functional outcomes according to (TcMAG3) diuretic renography’s from our consecutive cohort. 70 adults underwent a RA dismembered Anderson-Hynes pyeloplasty. Following the surgery, stents were left in place for 4 weeks. The patients had a renography prior to surgery and at 3, 6, 12 months during follow up. For the analyses, relative uptake by split renal function, time to peak height activity (Tmax), and residual activity at 20 minutes were measured.
Results: A total of 70 op were performed as all patients were eligible for the study. A total of 62 patients (88.6%) were pain free at three months follow up after pyeloplasty. This did not change during the remaining follow up period. Mean split renal function of the affected kidney was 43% prior to surgery, and 44%, 45%, 43% after 3, 6, and 12 months of follow up, respectively. Mean Tmax of the affected kidney was 10 min prior to surgery, and 7.7 min, 7.8 min, 7.4 min after 3, 6, and 12 months of follow up. Mean residual activity at 20 minutes of the affected kidney was 64% prior to surgery, and 45%, 44%, 41% after 3, 6, and 12 months of follow up. While no change was observed for split renal function, significant changes (P<0.05) were observed for Tmax and residual function following the surgery. After 3 months following the surgery, the renographies were stable and no further significant change was observed with longer follow up.
Conclusions: The drainage and functional outcome following a RA dismembered Anderson-Hynes pyeloplasty may optimally be described by a renography prior to and 3 months following the surgery. Further renography’s do not appear to be beneficial or provide further information.
SESSION IX - ORAL PRESENTATIONS – NURSES SESSION
AS-9.092
Nurse-led consultations – experiences and perspectives from the department of Urology at Haukeland University Hospital
Landro H M, Mohn J, Storebø T
Haukeland University Hospital, Urology, Bergen, Norway
Background: Nursing shortage is a reality. At the same time, our role as nurses at an outpatient clinic and the way we embrace nurse-led consultations have changed during the last decade. Expanded scope of nursing practice could result in enhanced feelings of professionalism. Flexibility, priority and preparations among the nurses are central issues to secure good clinical practice for our patients. Clinical nurse specialists seek to embrace a person-centered approach in the consultations. We assumed that the number of nurse-led consultations had increased in our outpatient clinic during the last decade. We wanted to investigate whether this was real or just an assumption, and how the different range of services and procedures were distributed.
Methods: Retrospective survey from 2013-2023 with numbers of nurse-led consultations and distribution of clinical procedures at an outpatient clinic at a University Hospital in Norway.
Results: The results are pending and will be presented at the congress.
Conclusions: The conclusions are pending and will be presented at the congress.
AS-9.093*
Project plan to produce video material for children on urodynamics
Bastrup Larsen H1, Andersen M1, Brun P1, Vilms Skou Pedersen M1, Junker T1,2
1Odense University Hospital, Urology, Odense, Denmark, 2Odense University Hospital, Research and Innovation Unit of Radiology, Odense, Denmark
Background: It is not unusual for children to have lower urinary tract dysfunction. If the initial examination is insufficient to initiate appropriate treatment, urodynamics (UD) can be indicated. UD is made with a catheter installed in the bladder and rectum, and EMG electrodes around the anus. A relaxed child is paramount to the outcome of the UD. At our institution, we recently had a 9-year-old boy scheduled for UD. Despite educational efforts, he was terrified, tried to escape, and did not hear the nurse’s explanation. The fear of the unknown was prominent and dominant. In addition, the child and parents lacked knowledge about the examination, despite the oral and written information given. Based on several similar episodes, the idea arose to make a short video about UD. The purpose of this project is to produce video material for the preparation of children who are to undergo UD.
Methods: Parents of children aged 4-10 have been interviewed about the idea. Experience-based knowledge from parents, nurses and doctors will be collected and used as a basis for content in the video. Equipment used for UD will be filmed and produced from the child’s perspective.
Results: Initially interviewed parents, nurses, and doctors welcomed the idea of producing a video on UD and will contribute with ideas on content and production. Children will be cast as actors, and a teddy bear with a suprapubic catheter will be used. The video will be produced as a demo, after which funding will be applied to produce the final product. It is the intention to have the video released on several platforms.
Conclusions: Adding video material to the patient information, intends is to secure a better patient experience on UD. A better patient experience can lead to a more relaxed child, the foundation of successful examination.
*Winner of best abstract in the Nurses scientific session
AS-9.094
Treatment of urethral recurrence following radical cystectomy and orthotopic neobladder
Plathan M L1, Löffeler S2, Haug E S2
1Sykehuset i Vestfold, Urology, Tønsberg, Norway, 2Sykehuset i Vestfold, Tønsberg, Tønsberg, Norway
Background: Urethral recurrence of urothelial cancer in patients with orthotopic neobladder (ONB) is challenging, as radical treatment requires urethrectomy and conversion to ileal conduit. Successful treatment with BCG has been reported, sparing the patient for major surgery, preserving voiding functions and quality of life. We present a case report and describe a revised method for BCG delivery to the urethra.
Methods: A patient with bladder tumor was operated with TUR-B and diagnosed with bladder cancer pTa + CiS, radiologic stage cT2. After multidisciplinary assessment, he was offered radical cystectomy with ONB December 2019 resulting in pT1 N0 and negative margins. The patient was satisfied with his ONB with a capacity of 5 dl and nighttime continence. Hematuria during follow up (FU) revealed urethral recurrence of a pTa low-grade April 2022. Laser coagulation was performed, but additional biopsies showed presence of CiS. Urethrectomy with conversion to an ileal conduit was considered, but in consultation with the patient it was decided to try BCG-treatment according to a protocol using a modified Foley catheter for irrigation of the urethra applying BCG through a perforation below the balloon.
Results: Treatment was performed as an outpatient procedure starting May 2022. The irrigation was performed with an initial bolus with distal obstruction of the lumen followed by slow continuous flow managed by pump for intravenous infusion. The patient has completed all induction and maintenance treatments, so far 12, with good tolerance. At cystoscopy check-up in March 2023 there was no sign of recurrence. The patient will continue treatment with BCG for a minimum of one year.
Conclusions: Local BCG treatment may save a well-functioning ONB with urethral recurrence. Longtime data is lacking, and thorough FU is mandatory.
AS-9.095
Intracavitary BCG Instillation in Upper urinary Tract Urothelial Carcinoma
Plathan M L, Haug E S
Sykehuset i Vestfold, Urology, Tønsberg, Norway
Background: High-grade urothelial cancer (UTC) in the upper urinary tract (UTUC) is a serious condition that according to guidelines demands Nephro-ureterctomy (NU) in most cases. In patients with singel kidney or bilateral disease, nephron sparing alternatives are wanted. There is vast experience of bladder instillation of BCG and there is guidelines for adjuvant chemoinstillation in the bladder for UTUC. Data on efficacy and methods for intracavitar BCG (IC-BCG) treatment in the upper tract is though lacking. We will present our experience with BCG treatment for UTUC and different methods for IC-BCG instillation.
Methods: Patients treated with IC-BCG for UTUC were identified in our local registry and medical record assessed. Depending on the accessibility of the upper tract, protocols both for instillation by intraluminal urethral stents and by nephrostomy tubes were used. Position of stents and the nephrostomy was thoroughly checked before each treatment. When instilling BCG through stents we made a small incision in the upper end of the stoma bag to access the end of the stent and to avoid spilling of BCG. When instilling by nephrostomy we attached the three-way faucet for instillation. The patient voided at the end of the procedure. The infusion was given by bolus 5ml every 10th minute for one hour.
Results: We have performed 4 treatments of IC-BCG in 3 patients. Two treatments were distributed by stents through the ileal conduit and two by nephrostomies – in one patient bilateral. The patients kept stents and nephrostomies between each weekly instillation. Allocated time for each instillation was 2 hours. The patients underwent from 10 to 12 IC-BCG in the outpatient clinic. In one patient it was stopped due to recurring urinary infections. Complaints were mostly related to stents and nephrostomy.
Conclusions: IC-BCG is feasible, well tolerated, but a resource-intensive alternative to NU and dialysis and requires interdisciplinary coordination.
AS-9.096
My Care Plan cancer via 1177
Hägglund A
Regionalt cancercentrum Stockholm Gotland, Stockholm, Sweden
Background: One of the ten missions RCC is working on is knowledge management. To support cancer care employees and patients so that every meeting is based on the best possible knowledge. To achieve that, RCC offers various supports and tools, based on research. Within knowledge management, there are a number of knowledge supports, such as National Care Programs, Boa Image Frameized Care Processes (SVF), the Regime Library, registers, patient summaries (IPÖ) and My Care Plan (MVP).
Methods: My Care Plan contains patient information that has been developed and managed by national working groups. The information contained in My Care Plan is both diagnosis-adapted and general. Through the various functions available with messages, contact, assessment forms or activity plans, you can make it individualized for the patient and work more person-centered and get the patient more involved in their care.
Results: In My Care Plan there is nationally quality-assured information where the patient receives information about what should happen during and after treatment and self-care advice. There is also information about the patient’s cancer drugs – taken from the Regime Library. The Regime Library contains detailed recommendations on how to use cancer medicines.
Conclusions: My Care Plan is the patient’s plan. It is a support for creating participation, security and understanding for the patient and relatives.
AS-9.097
G8 and Mini-COG testing for geriatric screening of older prior to inclusion in clinical trials in general and SPCG-19 in particular
Langsrud K S, Löffeler S
Sykehuset i Vestfold, Urology, Tønsberg, Norway
Background: SPCG-19 is a randomized, open label, multicenter, parallel group treatment, phase 3, two-arm study to measure the effect on overall survival and quality of life of immediate curative therapy compared to standard conservative treatment in older male participants aged > 75 years with non-metastatic, high-risk prostate cancer. Geriatric screening of patients is performed by study nurses prior to inclusion in the study.
Methods: Patients eligible for the study have to be 75 years or older. In accordance with urological and oncological guidelines patients are screened by G8 miniCOG tests, which are fast and simple screening tests to map patients’ general health and cognitive status. The test takes less than five minutes.
Results: Since we started to include patients in November 2022, we have tested eight patients. They all scored ≥14 points at G8 and all patients passed the miniCOG test (minimum 3/5 points). Test results of the miniCOG test were clearly influenced by the surroundings with stress leading to more stress which compromised patients’ focus on the task. Unneccessary stress may thus lead to less reliable results in miniCOG testing. Most patient were familiar with the miniCOG test from previous exposure.
Conclusions: G8 and miniCOG testing are meaningful tests in elderly patients for determining general health and cognitive function. Both tests can be easily performed by study nurses. Both tests help to identify frail patients which are unfit to receive standard treatment and/ or to participate in a clinical trial. Patients who fail either or both tests need further geriatric work-up.
AS-9.099, AS-11.124
The burden of urinary tract infections in Scandinavia – findings from a cross-sectional, population-based survey
Andersen F B1, Scheffel G2, Nedland B3, Jacobsen L4
1Coloplast Danmark A/S, Humlebæk, Denmark, 2Coloplast Sweden A/B, Kungsbacka, Sweden, 3Coloplast Norway A/S, Oslo, Norway, 4Coloplast, Humlebæk, Denmark
Background: Urinary tract infections (UTIs) are common complication in users of clean intermittent catheterization (CIC) and constitute a major concern. The objective was to explore the burden of UTIs in Scandinavia (Denmark, Norway and Sweden), including the mental burden of worrying about UTIs.
Methods: In March-April 2022, an online survey was distributed among CIC users and comprised questions on UTI incidence, symptoms, bladder emptying technique, residual urine, blood in urine and the disease-specific quality of life questionnaire, Qualiveen-30.
Results: A total of 1009 CIC users responded to the survey, and the male/female ratio was 49%/25% (26% unknown). There were 665 respondents from Denmark, 184 from Norway and 160 from Sweden. 38% used CIC due to neurogenic issues, 49% due to non-neurogenic issues with 80% of the CIC users suffering from urinary retention, 29% from urinary incontinence and 17% from bowel issues. Within the last year, 57% of the CIC users had experienced at least one UTI requiring antibiotic treatment and annual UTI level was estimated to 1.78 (95% CI = 1.53-2.07). Of the population experiencing UTIs, 47% had 3 or more UTIs, 11% had been hospitalised due to UTIs, of which 16% were hospitalised 3 times or more in a year. Among the CIC users experiencing UTIs 85% had antibiotics prescribed by a doctor and 17% had antibiotics available from home-stock. The leading cause of worry when performing CIC concerned getting a UTI (61%), followed by inserting bacteria into the urethra (57%) and not emptying the bladder completely (43%).
Conclusions: This cross-sectional population-based survey show that CIC users in Scandinavia experience high level of UTIs. This is also reflected in a substantial patient and healthcare burden due to high rates of hospitalisations and antibiotic treatment. High mental impact was observed among CIC users concerning worries about UTIs, bacteria in urethra and not emptying the bladder completely.
AS-9.125
Evidence-Based Method for Collecting a Urine Sample - A Quasi-Experimental Study of Nursing Staff’s Adherence to Guidelines
Knutsen R N, Jensen B T
Aarhus University Hospital, Department of Urology, Aarhus, Denmark
Background: A bladder catheter is a frequently used treatment in clinical practice. The presence of a bladder catheter is associated with the development of a catheter-associated urinary tract infection (CAUTI), where collection of a urine sample for microbiological examination is essential in relation to early and correct treatment of the infection. EAU guideline from 2021 recommend that in patients with symptoms of a CAUTI, where the bladder catheter has not been placed within the last 7 days, the bladder catheter should be changed prior to collecting a urine sample. Despite these precise recommendations, the practice of collecting a urine sample from patients with symptoms of a CAUTI seems unchanged.
Methods: A quasi-experimental study was designed at Department of Urology at Aarhus University Hospital. to explore current adherence to guideline regarding correct urine sampling in patients with symptoms of CAUTI. Adherence to evidence-based practice was measured before and after a focused teaching intervention with the overall aim to inform, educate and improve adherence to guideline in clinical practice. A descriptive tool to monitor the course of care was developed for the purpose to collect data before and after the intervention. Fishers Exact Test was used to test proportions for statistically significant differences.
Results: A total of 38 nurses participated in the screening for adherence before the intervention and 22 after. Data collected before the intervention showed that knowledge about CAUTI and correct sampling of urine was deficient and adherence to guidelines was considered low. Likewise, the adherence to current guidelines was significantly improved after the intervention.
Conclusions: A short and well-planned teaching intervention can increase nursing staff’s knowledge and adherence to an evidence-based practice and secure a correct collection of a urine sample from a bladder catheter in patients with symptoms of a CAUTI.
SESSION X - POSTER PRESENTATIONS – MISCELLANEOUS
AS-10.100
Positive consequences regarding hospital staff resources, caused by a shift from sedation/general anesthesia to local anesthesia during intravesical treatment with botulinum Toxin A (Botox) for overactive bladder (OAB). A total game-changer
Schou J
Herlev/Gentofte Hospital, Department of Urology, Copenhagen, Denmark
Table 1. Presenting staff use during 6 treatments/1 day.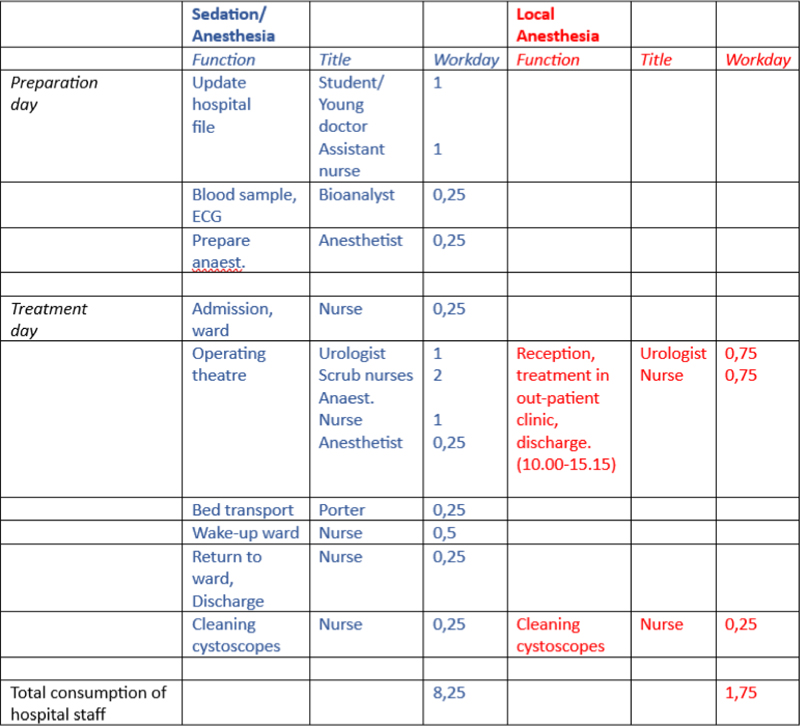
Background: The aim was to determine the consequences regarding hospital staff resources, during a shift from sedation/general anesthesia to local anesthesia during intravesical treatment with Botulinum Toxin A (Botox) for overactive bladder (OAB).
Methods: A vast majority of patients (>93%) prefer Botox treatment in local anesthesia in an outpatient setting, and consequently we changed our mind-set, and offer Botox-naïve patients this modality as a first line treatment. We treat 850-900 patients/year, and maximally 80 of these are under admission. We performed 6 treatments/day at the OR, and the same number is treated in the out-patient clinic.
Results:
Conclusions: As the table shows, there is a tremendous decrease in the demand for staff resources with the new concept. A demand for 6 treatments/day falling from 8,25 to 1,75 workdays speaks for itself. The gain/year is in loose terms: 800 treatments/6 per treatment day is 133 days. Each day saves 6,5 workdays. Saving/year: 865 workdays. In DK we work approximately 200 days/year, meaning a saving of over 4 work years/year.
AS-10.101
The use of intradetrusor injection with botulinum toxin A (BTX) in adults is increasing at Haukeland University Hospital (HUH)
Myskja M, Beisland C, Gudbrandsdottir G, Bergesen A, Roth I, Hjelle K M
Haukeland University Hospital, Department of Urology, Bergen, Norway
Background: When conservative treatment options have failed, intradetrusor injections of BTX has been used to treat neurogenic (NB) and non-neurogenic (N-NB) overactive bladder. We aimed to evaluate our practice patterns at HUH over the two last decades, as the number of patients and treatments seemed to have increased.
Methods: Retrospective registration of patients receiving BTX from 2001-2020 identified 161 adult patients. Data were retrieved from the medical records as part of a clinical audit.
Results: Median age was 53 years (IQR 33-66) and 61 % were females. Treatment indication was NB in 84 patients (52%) and N-NB in 77 (48%). 89% were treated in local anaesthesia, the remainders under sedation or general anaesthesia. For NB patients, initial doses of <200 IU, 200 IU and 300 IU were given to 36 (43%), 29 (34%) and 19 (23%) patients, respectively. The initial dose among N-NB was overall lower with 79% receiving 100 IU and 21% >100 IU initially. During follow-up (FU) the BTX dose was increased in 47%. Overall cystometry was performed pre-BTX in 89%, but only in 26% during FU (mostly in the NB-group). Comparison of cystometry pre-BTX and at FU a showed a significant reduction in maximum detrusor pressure during filling; from 55 cmH2O to 26 cm H2O and an increased cystometric capacity; from 312 to 380 ml (paired T-test, p<0,05 for both). 45% are still on BTX treatment at HUH, 21% have been referred elsewhere and 34% are terminated (mostly due to urinary diversion or lack of indication/effect). FU-time for patients still in treatment (n=73) was median 6 years (IQR 4-9, range 1-19). The number of new BTX patients are increasing. There were 22, 41 and 98 new patients in 2003-08, 2009-14 and 2015-20, respectively. The overall number of annual BTX sessions more than doubled from 63 in 2016 to 140 in 2020.
Conclusions: Intradetrusor BTX is a safe and effective. There is overall an increasing number of patients receiving BTX treatment. This expansion is especially visible for N-NB patients.
AS-10.102
Induction of bacterial cystitis in female rabbits by uropathogenic Escherichia coli and the differences between the bladder dome and trigone
Rizk D1, Rizk D1, Rizk D1,2,3
1College of Medicine and Medical Sciences, Arabian Gulf University, Anatomy, Microbiology, Physiology, Manama, Bahrain, 2College of Medicine and Medical Sciences, Arabian Gulf University, Obstetrics and Gynaecology, Manama, Bahrain, 3Vita-Salute San Raffaele University, IRCCS San Raffaele Hospital, Urogynecology Unit, Department of Obstetrics and Gynecology, Milan, Italy
Background: Studies showed that infections located within the bladder trigone may be associated with higher risk of recurrence of urinary tract infections (UTI) in women than those affecting rest of the bladder. Our objective was to describe an animal model of bacterial cystitis and investigate whether histological effects are different between the trigone and dome.
Methods: Female New Zeeland white rabbits (age 4-6 months, weight 2-2.5 kg) were used; 13 study- 8 controls (n=21). Cystitis was induced by transurethral inoculation of uropathogenic E coli (UPEC) into the urinary bladder (n=13). Urine samples were collected by catheterization and cultured for bacterial growth after 12 and 24 hours then every 48 hours. Infection was defined as ≥1x10 5 UPEC colony-forming unit/ml in the first two urine samples. Bladder dome and trigonal specimens were examined by light and scanning electron microscopy eight days post-infection.
Results: Sustained increase in bacterial count, urethral bleeding and rabbit weakness confirmed bladder colonization in 10/13 study group (77%). Infection was not demonstrated in two animals and was spontaneously cleared in the third after 48 hours. No controls developed infection. The dome showed inflammatory changes including epithelial thinning or loss, inflammatory cell infiltration of the connective tissue and congested blood vessels in infected rabbits (n=10) compared to controls. There was a more pronounced trigonal inflammatory response in the ten animals particularly complete loss of epithelium, inflammatory cells infiltration across all layers and considerable congestion with peri-muscular hemorrhage.
Conclusions: Structural and ultra-structural inflammatory changes occurred throughout all urinary bladder layers in study compared to control rabbits confirming utility of this animal model to study UTI. The findings were more marked in the trigone than in the dome suggesting a possible role of trigone in recurrent UTI with potential clinical applications.
AS-10.103
Can We Consider ‘Endometriosis’ as Side Effect of Intravesical BCG? -A Case Report of Extremely Rare Occurence in a Male
Sarkar P k1, Koslowski M2, Jones M1, Ahmed I1, Papadopoulos G1, Streeter E1
1Kent and Canterbury Hospital, Urology, Canterbury,Kent, United Kingdom, 2Kent and Canterbury Hospital, Histopathology, Canterbury,Kent, United Kingdom
Background: Endometriosis which denotes the abnormal growth of tissue resembling endometrium in ectopic sites,has largely been studied in women of reproductive age and is an extreme rare phenomenon in men with a total of 16 cases previously reported in the literature . The present case describes finding of Bladder Endometriosis in a 66-year-old man with history of Intravesical BCG induction on a background of Bladder cancer.
Methods: A 66-year gentleman was initially referred with visible haematuria and lower urinary tract symptoms. His past medical history includes Hypertension, Chronic plaque Psoriasis, Panproctocolectomy and ileo-jejunal pouch formation for Ulcerative Colitis, AF. He was put on Finasteride 2 weeks before referral. Transurethral resection of bladder tumour seen on flexible cystoscopy confirmed G3pTa papillary urothelial carcinoma with clear upper renal tract on imaging. Early relook bladder biopsy showed benign histology followed by 6 cycle of induction intravesical BCG treatment.
Results: Post -BCG Rigid Cystoscopy--3 mm small lesion close to left Ureteric orifice and interestingly ,Bladder biopsy described feature of Endometrium (both endometrial gland and stroma) which was confirmed with Immunostains - stroma positive for CD 10 and ER, Glands positive for CK7 and ER and no Transitional epithelium seen. There are very few cases of this in the literature at all and most seem to relate to high levels of oestrogen secondary to prolonged hormone therapy for prostate cancer, liver disease or high body mass index. But our patient was very slim and neither have Liver Cirrhosis nor Prostate cancer. Although he was treated with steroid hormones around 20 years ago prior to having major bowel resection, these would have been of the inflammatory type rather than the sex steroid type, therefore should have no influence.
Conclusions: In summary, endometriosis is an extremely rare lesion in men. Awareness of this entity is crucial for general pathologists to avoid wrong diagnosis and unnecessary management.
AS-10.104
Entrapped Penile Ring Removal with Metal Cutting Diamond Disk
Stork B, Eltahawy E
University of Michigan, Department of Urology, Ann Arbor, Michigan, United States of America
Background: Penile rings are commercially available in a wide range of different shapes, sizes, and materials. Entrapped rings compromise venous outflow, decrease arterial inflow, and, if not removed in a timely manner, can result in ischemia of penile tissue. Rings made of metal can be particularly challenging to remove.
Methods: A 72-year-old man with history of erectile dysfunction presented to the emergency room 6 hours after placing a 0.7 cm thick steel ring at the base of his penis. Emergency room physicians made multiple attempts to remove the ring without success. The patient was taken to the operative room, administered a general anaesthetic, and a penile block was performed. A Foley catheter was placed, and a thin malleable retractor was positioned between the metal ring and the penis. Sterile water was continuously run onto the operative field. An air powered drill with an attached Stryker Metal Cutting Diamond Disk (25.4 mm x 0.8 mm reference number 5120-130-250) was used to cut the ring into two pieces. The ring was then safely removed.
Results: Total time from ring placement to removal was 17 hours. Operating room time was 112 minutes. Five metal cutting diamond disks were used during the case.
Conclusions: Entrapment of the penis by a metal ring presents a challenging clinical problem for emergency room physicians and urologists alike. Intraoperative ring removal with the aid of metal cutting diamond disks and drill can be a safe and effective surgical option when other less invasive treatment options fail.

Figure 1. Cutting of Entrapped Penile Ring with Metal Cutting Diamond Disk.
AS-10.105
Clinical presentation and treatment for urachal cancer – a nationwide retrospective study from Norway
Akhtar S N1, Haug E2, Carlsen B3, Aarsæther E J4, Karlsvik A-K5, Kjøbli E5, Hannestad I6, Müller S6, Brennhovd B7, Dimmen M8, Beisland C1,9, Gudbrandsdottir G1,9
1Department of Urology, Haukeland University Hospital, Bergen, Norway, 2Department of Urology, Vestfold Hospital, Tønsberg, Norway, 3Department of Pathology, Vestfold Hospital, Tønsberg, Norway, 4Department of Urology, University Hospital of North Norway, Tromsø, Norway, 5Department of Urology, St. Olavs University Hospital, Trondheim, Norway, 6Department of Urology, Akershus University Hospital, Lørenskog, Norway, 7Department of Urology, Oslo University Hospital, Oslo, Norway, 8Department of Urology, Bodø Hospital, Bodø, Norway, 9Department of Clinical Medicine, University of Bergen, Bergen, Norway
Background: Urachal carcinoma is a rare type of cancer in the bladder which makes it difficult to study in a prospective setting. International guidelines’ recommendation are based on small single centre studies, and carry a low level of evidence. The aim of this study is to explore the clinical presentation and to evaluate indications for different treatment strategies used for urachal cancer.
Methods: In Norway, advanced bladder cancer surgery is centralized to seven centres. Patients were retrieved from five centers. One center had no eligible patients and the final center has yet to retrieve data. The cohort consist of 38 patients. Patient characteristics, surgery-, and histopathological related variables, as well as data on complications and treatment after surgery were obtained. During the period 1997-2021, a total of 48 patients has been reported to the cancer registry of Norway. The study is approved by the Ethics Committee in Western Norway.
Results: Of the patients 21 (55%) were male. Median age at surgery was 64 (IQR 53-75). Seven patients (18%) were incidentally diagnosed. The remaining 31 had symptoms, the most common being macroscopic haematuria (n=25 (66 %)). Four (11 %) had dysuria and two (5%) presented with abdominal pain. 8 patients had two symptoms, 4 with UTI and 4 with pollakisuria. Median tumour size was 3.5 cm (IQR 2.5-5.0 cm). Most patients underwent bladder resection (n=20, 53%), while 16 (42%) had cystectomy and two TUR-BT. 34 had surgical free margins. Median follow up was 47 months (IQR 25-108 months). The mean tumour size for the cystectomy group was 4.9 cm compared to 3.3 cm for the bladder resection group (p<0.01). Patients treated with bladder resection showed a significant better survival (p=0.048) compared to those treated with cystectomy.
Conclusions: Most patients were symptomatic at time of diagnosis. Treatment seems to be based on size of tumour, which might explain the survival difference seen between the cystectomy group and the bladder resection group.
AS-10.106
Non-inferiority, randomized, open-label clinical trial on the effectiveness of transurethral microwave thermotherapy compared to prostatic artery embolisation in reducing severe lower urinary tract symptoms in men with benign prostatic hyperplasia
Kristensen-Alvarez A1, Fode M2, Stroomberg H V1, Røder A1
1Rigshospitalet, Urological Research Unit, Copenhagen, Denmark, 2Copenhagen University Hospital - Herlev and Gentofte Hospital, Department of Urology, Copenhagen, Denmark
Background: The objective of this clinical trial is to assess if prostatic artery embolization (PAE) is non-inferior to transurethral microwave thermotherapy (TUMT) in reducing lower urinary tract symptoms (LUTS) secondary to benign prostatic hyperplasia (BPH). The primary aim is to compare LUTS 6 months after TUMT and PAE, measured by the International Prostate Symptom Score (IPSS). Both treatments have previously been shown to reduce LUTS with a similar post-procedure outcome in mean IPSS. However, the previous studies differed in baseline characteristics thus it is currently unknown if they perform equally well. Secondary objectives include comparison of patient reported and functional outcomes at short- and long-term follow-up.
Methods: This study is designed as a multi-centre, non-inferiority, open label randomised clinical trial. Patients will be randomised with a 1:1 allocation ratio between treatments using the randomisation module in REDCap. The primary outcome is expected to be evaluated by a 95% confidence interval against the predefined threshold of +3 points in IPSS for inferiority. Assuming a difference in mean IPSS after treatment of 1 point with an SD of 5 and a non-inferiority margin set at the border for a clinically non-meaningful difference of 3 points, the calculated sample size was 100 patients per arm. To compensate for 10% drop-out the study will include 220 patients. An interim analysis will be performed for every 50 cases.
Results: TUMT and PAE are minimally invasive procedures performed in an outpatient setting that have been shown to reduce LUTS in a similar magnitude. To date there are no randomised clinical trials comparing PAE to TUMT, which is problematic as the most prominent problem with minimally invasive BPH treatment is the lack of proper selection of candidates for a specific procedure.
Conclusions: We expect non-inferiority of PAE to TUMT. With analysis of the secondary outcomes, we aspire to contribute to a better understanding of patient selection for either treatment.
AS-10.107
Predictors of surgical treatment in male patients with non-neurogenic lower urinary tract symptoms (LUTS)
Hopland-Nechita F V1,2, Andersen J R3, Beisland C2,4
1Førde Central Hospital, Surgical Department, Førde, Norway, 2University of Bergen, Department of Clinical Medicine, Bergen, Norway, 3Western Norway University of Applied Sciences, Førde, Norway, 4Haukeland University Hospital, Department of Urology, Bergen, Norway
Background: To investigate clinical and biochemical predictors of future need for surgical treatment in male LUTS patients
Methods: This is a prospective cohort study following strict inclusion and exclusion criteria. The international prostatic symptom score (IPSS) and IPSS “bother question” (IPSS-BQ) were collected at baseline, together with data on prostate volume (PV), uroflowmetry, PSA, post-voiding residual (PVR) urine and comorbidities. Comorbidities were quantified using the Charlson Index and the ASA score. The IPSS total score (IPSS-TS) and both subscores (Voiding symptoms (IPSS-VS) and storage symptoms (IPSS-ST) were recorded. The follow-up and the surgical indication were both set according to standard of care by EAU guidelines. All surgical procedures were done using bipolar TUR-P from Olympus Medical. For analyses the patients were divided into two groups (Group 1: underwent later surgery; Group 2: medical treatments or no treatment). T-test was used to test differences between the groups. Logistic regression models were used to identify independent predictors of need for future surgery
Results: We included 63 eligible patients of which 22 underwent surgery during follow-up. The median follow up was 42 months (IQR 30-50). There were statistically significant differences between the two groups at baseline with p=0.003, p=0.002 and p=0.001 for IPSS-TS, IPSS-VS and IPSS-BQ, respectively. The IPSS-ST was not significantly different (p=0.14). Also Qmax (p=0.007) and PVR (p=0.02) showed significant differences between the groups at baseline. For age, ASA-score, Charlson index, PSA and PV, there were no statistical differences. In logistic regression analyses IPSS-BQ (OR 3.78 (95% CI, 1.51 – 9.49) p=0.005); IPSS-VS (OR 2.17 (95% CI, 1.04 – 4.52), p=0.039) and Qmax (OR 0.88 (95% CI, 0.77 – 0.99), p=0.038) remained independent predictors of surgical treatment.
Conclusions: At baseline, the IPSS-VS subscale, IPSS-BQ and Qmax were predictors for future need for surgical treatment
AS-10.108
Cognitive coaxial transperineal prostate biopsy without antibiotic prophylaxis is safe
Honoré A1, Moen C A1, Juliebø-Jones P1,2, Chaudhry A A1, Rawal R1, Sandøy A1, Reisæter L A R3, Gravdal K4, Beisland C1,2
1Haukeland University Hospital, Urology, Bergen, Norway, 2University of Bergen, Department of Clinical Medicine, Bergen, Norway, 3Haukeland University Hospital, Radiology, Bergen, Norway, 4Haukeland University Hospital, Pathology, Bergen, Norway
Background: Increasing rates of urosepsis following transrectal prostate biopsy (TRBx) in our department warranted a change. Transperineal prostate biopsy (TPBx) is associated with fewer complications and is the recommended biopsy procedure in the current EAU guidelines. We aimed to reduce complications by introducing a coaxial TPBx technique that allows for both cognitive fusion targeted biopsy as well as standard biopsies.
Methods: Patients biopsied between January 1st, 2018 and May 31st, 2022 at our department were included. For patients included in active surveillance, biopsies before and after this period were also included. The TRBx- and TPBx groups were compared regarding complications and antibiotic use. Pearson’s Chi-squared test was used to examine differences between groups. The study is approved by the regional ethics committee in Western Norway, and all patients have consented.
Results: 1,915 patients were included with 2,116 separate biopsy sessions, 1,027 of which were TPBx. All (100%) TRBx patients received antibiotics, but only 2.4% of TPBx (p<0.001). In total, 5.0% of TRBx patients were admitted to hospital, while only 0.3% following TPBx (p<0.001). There were no cases of urosepsis in the TPBx group.
Conclusions: Coaxial TPBx can safely be performed without antibiotic prophylaxis.
AS-10.109
Unilateral pelvic lymph node dissection may be feasible in selected men with clinically node negative prostate cancer undergoing radical prostatectomy
Aas K1,2, Axcrona K1,3, Lilleaasen G4, Mygland V1, Hammarström C5, Myklebust T Å6,7, Müller S1
1Akershus University Hospital, Department of Urology, Lørenskog, Norway, 2University of Oslo / Institute of Clinical Medicine, Oslo, Norway, 3Oslo University Hospital Radiumhospitalet / Institute for Cancer Research, Department of Molecular Oncology, Oslo, Norway, 4Akershus University Hospital, Department of Urology, Oslo, Norway, 5Akershus University Hospital, Department of Pathology, Lørenskog, Norway, 6Cancer Registry of Norway, Oslo, Norway, 7Møre and Romsdal Hospital Trust, Department of Research and Innovation, Ålesund, Norway
Background: The aim of this study was to describe pathological lymph node (pN1) detection, persistent PSA and secondary cancer treatments in men with clinically node negative (cN0) prostate cancer (PCa) undergoing unilateral vs bilateral pelvic lymph node dissection (PLND) at the time of robot-assisted radical prostatectomy (RALP).
Methods: Retrospective study of men who underwent RALP and PLND at Akershus University Hospital in 2022. All patients had cN0 disease on pelvic MR and were stratified according to unilateral or bilateral PLND. Persistent PSA was defined as PSA ³0.1 after six weeks. Secondary PCa treatments included hormonal treatment and/or radiotherapy. Follow-up was until March 2023. The independent T test compared continuous variables and the χ2 test compared categorical variables. A p-value of < 0.05 was considered significant.
Results: In 72 evaluable patients, 14 (19%) and 58 (81%) men underwent unilateral and bilateral PLND, respectively. Lower iPSA and Briganti scores were observed in the unilateral PLND group, but no differences in pathological T-category or surgical margins. Median six vs 14 nodes were removed in uni- vs bilateral PLND. Overall, 14% had pN1 disease, 13% persistent PSA and 15% underwent secondary PCa treatments, with no differences observed among the PLND groups. One patient in the unilateral group had persistent PSA and bone metastasis were detected on postoperative PET-scan.
Conclusions: No differences in pN1 detection or short-term oncological outcomes were observed for unilateral vs bilateral PLND in a small sample of men with cN0 PCa undergoing RALP. Unilateral PLND may be feasible in selected men.
AS-10.110
Genetic risk score predicting cholesterol as a prostate cancer prognostic factor
Boele S1, Murtola T1, Siltari A1, Raittinen P2, Tammela T2, Auvinen A2, Talala K2, Taari K2, Schleutker J2
1Tampere University, Faculty of Medicine and Health Technology, Tampere, Finland, 2Tampere University, Tampere, Finland
Background: Prostate cancer progression and treatment resistance are known to be influenced by intracellular cholesterol metabolism. However, the degree to which serum cholesterol and lipoprotein levels are associated with prostate cancer outcomes remains unclear. The objective of the study was to estimate whether SNPs predicting serum cholesterol and lipoproteins also predict mortality among a cohort of men with prostate cancer. Mendelian randomization theory states that germline SNP distribution is unaffected by confounding variables such as diet and lifestyle factors.
Methods: Using data collected by the Finnish Randomized Study of Prostate Cancer Screening, our study cohort consisted of 3,241 men diagnosed with prostate cancer between 1996-2015. Patient blood samples were genotyped by the PRACTICAL consortium and a genome browser was utilized for selecting 85 SNPs in lipid metabolism-associated genes. A regional laboratory database provided information on serum cholesterol and lipoprotein levels. Linear regression and lasso regression were utilized to create scores predicting serum cholesterol, LDL, HDL and triglyceride levels by SNP genotype. Then, a multivariable-adjusted Cox regression was used to evaluate the risk of prostate cancer death and overall mortality by level of the SNP risk score.
Results: SNP score predicting total cholesterol stratified prostate cancer patients both for disease-specific (HR 1.27, 95% CI 0.49-3.28 for highest tertile vs. lowest) and overall survival (HR 1.43, 95% CI 0.94-2.20, p for trend 0.077), albeit statistical significance was not reached. Similar survival differences were observed for SNP scores predicting triglyceride levels, but not for scores predicting LDL or HDL levels.
Conclusions: SNPs predicting serum cholesterol and triglycerides are likely prognostic factors for the survival of prostate cancer patients. This implies that serum cholesterol and lipoproteins are also of importance in prostate cancer progression.
AS-10.111
Impact on Prostatype® P-score on treatment and long-term outcomes
Röbeck P1, Berglund E2, Dragomir A3, Dahlman P4, Häggman M1, Ladjevardi S1
1Akademiska sjukhuset Uppsala, Urology, Uppsala, Sweden, 2Prostatype Genomics, Solna, Sweden, 3Akademiska sjukhuset Uppsala, Department of Pathology, Uppsala, Sweden, 4Akademiska sjukhuset Uppsala, Department of Surgical Sciences, Uppsala, Sweden
Background: Better risk stratification of prostate cancer (PCa) will encourage acceptance of active surveillance (AS), help to reduce overtreatment, and alleviate some of the concerns about screening for PCa. New tissue genomic classifiers are likely to become widely used and increasingly valuable in clinical practice, in part because their reproducibility provides assurance relative to the variations in expertise among pathologists in assigning Gleason grade and among radiologists in performing and interpreting MRIs. The decision for observation or definitive therapy is so important, and so laden with potential effects on quality of life, that physicians and patients will continue to seek genomic classifiers to assist them in making better medical decisions. The established risk factors at the time of diagnosis are clinical stage, circulating prostate-specific antigen (PSA) levels, and the Gleason grade and extent of cancer in a biopsy specimen. These prognostic factors are sufficient for general risk stratification but have limited utility for predicting the long-term risk of metastases and death, especially among men with low- or intermediate-risk cancers.
Methods: Prostatype® test can predict the risk of dying from PCa within 10 years. The test combines results from mRNA analysis of 3 stem-cell genes together with the clinical parameters PSA, Gleason grade and tumor stage.
In this study, 500 patients, mainly clinically low- and intermediate-risk, were analyzed with the Prostatype® test. The long-term risk for prostate cancer mortality was investigated (up to 30 years of follow-up).
Results: This study demonstrate that higher P-score is strongly associated with worse long-term outcomes (prostate cancer specific mortality), supporting the clinical utility of the Prostatype® test.
Conclusions: The results suggest that the Prostatype® test provides information on the risk for the meaningful long-term outcomes of prostate cancer specific mortality.
AS-10.112
Ki67 and prostate specific antigen are prognostic in metastatic hormone naïve prostate cancer and may be predictive for efficacy of adjuvant docetaxel
Spyratou V1, Freyhult E2, Bergh A3, Thellenberg-Karlsson C4, Wikström P3, Welén K1,5, Josefsson A1,6,7
1Department of Urology, Institute of Clinical Sciences, University of Gothenburg, Gothenburg, Sweden, Gothenburg, Sweden, 2Department of Cell and Molecular Biology, National Bioinformatics Infrastructure Sweden, Science for Life Laboratory, Uppsala University, Uppsala, Sweden, Uppsala, Sweden, 3Department of Medical Biosciences, Pathology, Umeå University, Umeå, Sweden, Umeå, Sweden, 4Department of Radiation Sciences, Oncology, Umeå University, Umeå, Sweden, Umeå, Sweden, 5Sahlgrenska Center for Cancer Research, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden, Gothenburg, Sweden, 6Department of Surgical and Perioperative Sciences, Urology and Orthopedics, Umeå University, Umeå, Sweden, Umeå, Sweden, 7Wallenberg Centre for Molecular Medicine, Umeå University, Umeå, Sweden, Umeå, Sweden
Background: For metastatic hormone naïve prostate cancer patients, androgen deprivation therapy (ADT) is the standard therapy, together with adjuvant addition of docetaxel or androgen targeting drugs, but markers for patient selection are lacking. The purpose of the present study was to investigate if Ki67 and prostate specific antigen (PSA) immunoreactive scores can identify patients who benefit from ADT alone and those who need additional therapy.
Methods: Prostate biopsies from 92 patients with metastatic hormone naïve PC were immunohistochemically evaluated for PSA and KI67. Gene expression analysis was performed with Clarion D microarrays to identify phenotypic profile associated with the immunohistochemistry scores.
Results: Cox regression analysis after adjustment for age, ISUP, and serum PSA value demonstrated that KI67 labeling index was positively, and PSA immunoreactive score negatively associated with progression-free and overall survival. Patients with a high Ki67/PSA ratio significantly benefitted from docetaxel treatment added to ADT, while no benefit was seen for those with a low Ki67/PSA ratio. Accordingly, mRNA expression data analysis showed an association between high Ki67/PSA ratio, cell-cycle regulation, and DNA damage repair.
Conclusions: PSA and Ki67 immunoreactive scores are prognostic in the metastatic hormone sensitive setting. Their combined evaluation can distinguish patients with metastatic prostate cancer who benefit from early addition of docetaxel as adjuvant therapy to ADT. Since the number of patients treated with docetaxel was small, further studies are warranted to establish these results.
SESSION XI - POSTER PRESENTATIONS – MISCELLANEOUS
AS-11.113
Late effects impact on Quality of Life after treatment for bladder cancer (CONQUER)
Milling R V1, Nielsen N K1, Graugaard-Jensen C1, Christensen P2, Pappot H3, Bjerggaard Jensen J1
1Aarhus University Hospital, Department of Urology, Aarhus, Denmark, 2Aarhus University Hospital, Department of Surgery, Aarhus, Denmark, 3University Hospital of Copenhagen, Department of Oncology, Rigshospitalet, Copenhagen, Denmark
Background: Treatment of bladder cancer (BC) spans from conservative treatment with transurethral resection and instillation therapy to major surgery, radiotherapy, systemic oncological treatment, and variations thereof. Each treatment has a risk of complications and impact on Quality of Life (QoL). This risk has been inconsistently described, and the impact on QoL in some of the treatment groups has only been studied to a limited extend. The aim of this study is to investigate risk factors for impairment on QoL among patients with BC.
Methods: This is a prospective follow-up questionnaire study. All adult patients referred for examination because of haematuria in the Central Denmark Region during the year of 2022 was invited to participate. Invitations were sent along with the invitation to examination. The study group will fill out the questionnaire 6 times within a 5-year period; at baseline and at 4, 8, 12, 24, and 60 months after baseline. The questionnaires are validated and standardized QoL surveys as well as validated symptom-based questionnaires covering urological, gastrointestinal, and sexual function. Information about tumour, treatment, and late effects is obtained by accessing the patients’ electronic records.
Results: During 2022, 2486 patients were referred for suspicion of BC. 1991 patients met the inclusion criteria. 433 patients responded, making the response rate 22.2 %. Among all patients seen in the clinic, 15 % were diagnosed with BC. Among the responders, 12 % were diagnosed with BC. Responders versus non-responders were similar in age, ASA classification, smoking-status, and gender distribution. Additionally, the groups are similar regarding tumour stage and treatment. Additional results are pending.
Conclusions: Analyses of QoL data at baseline and 4-month follow-up for BC patients versus non BC patients will be presented at NUF 2023.
AS-11.114
Symptoms, side effects and immediate functional outcome following transurethral surgery of bladder tumours
Deacon N N1, Nielsen N K1, Jensen J B1,2
1Aarhus University Hospital, Department of Urology, Aarhus, Denmark, 2Aarhus University, Department of Clinical Medicine, Aarhus, Denmark
Background: The standard procedure for diagnosis and treatment of tumour tissue in the urinary bladder is transurethral resection of bladder tumour (TURBT). Despite that, research in patient-reported outcome (PRO) following transurethral surgery is limited. Assessment of the impact of TURBT on PRO will be useful when comparing newer treatment options such as En Bloc resection (EBR) or laser ablation (LA) with the conventional method. This project aims to elucidate the immediate symptom burden and quality of life (QoL) following TURBT. Furthermore, we aim at setting a standard of reference for future modalities in non-muscle invasive bladder cancer (NMIBC) treatment.
Methods: Patients undergoing bladder cancer related transurethral procedures at Aarhus University Hospital (AUH) complete a symptom-based questionnaire (ICIQ-M/F-LUTS), a QoL questionnaire (EQ-5D-3L) and a newly created post-transurethral operation side effects questionnaire (PROTO) at day 1 and day 14 post-operatively. The questionnaires will be used to compare PRO between the following 4 groups: patients with primary NMIBC undergoing EBR(1) or conventional TURBT(2), patients with recurrent NMIBC undergoing LA(3), and patients undergoing flexible cystoscopy without finding of tumour tissue(4).
Results: Patient inclusion is in progress and running from November 2022 to April 2023. As of mid-March, a total of 185 TURBT-like procedures (cTURBT, re-TURBT, cystoscopy with biopsy, EBR) have been performed at AUH. 119 of these were asked to participate with a participation rate of 79%. The remaining 66 patients were not asked due to logistical challenges or exclusion criteria. The LA and cystoscopy patients have been included on selected days in the outpatient clinic, and 36 have agreed to participate. Results are pending and will be presented at NUF Congress 2023.
Conclusions: The ambition is to provide knowledge to ensure improved patient information regarding the course of bladder surgery, thereby facilitating better patient-centred care.
AS-11.115
Thromboembolic Events in Patients Undergoing Neoadjuvant Chemotherapy and Radical Cystectomy for Muscle Invasive Bladder Cancer: A Study of Renal Impairment in Relation to Potential Thromboprophylaxis
Rydell H1, Ericson A1, Eriksson V1, Johansson M1,2, Svensson J3, Banday V1, Sherif A1
1Umeå university, Department of Surgical and Perioperative Sciences, Urology and Andrology, Umeå, Sweden, 2Länssjukhuset Sundsvall/Härnösand, Urology, Sundsvall, Sweden, 3Umeå university, Department of Statistics, Umeå School of Business, Economics and Statistics (USBE), Umeå, Sweden
Background: Recent studies on patients with muscle-invasive bladder cancer (MIBC) undergoing neoadjuvant chemotherapy (NAC) have shown an association between NAC and thromboembolic events (TEE) prior to radical cystectomy (RC). Recent studies suggest that central venous access catheters (CVAs) may induce TEEs, and low-molecular-weight heparin (LMWH) has been mentioned as possible prophylaxis. However, other studies have shown a high incidence of decreased renal function in these patients. The purpose of this study was to determine the portion of MIBC patients with NAC-induced TEEs who had decreased preoperative renal function for whom LMWH potentially would not be beneficial as prophylaxis.
Methods: We identified 459 cystectomized MIBC patients from two Swedish medical centers from 2009 to 2021. The inclusion criterion of cT2-T4aN0M0 resulted in 220 eligible patients, who were further divided into NAC-administered (n=187) and NAC-eligible (n=33), the tentative control group. Values of renal function before, during, and after each NAC cycle were retrospectively collected from individual medical records.
Results: Amongst the NAC-administered patients with TEE (n=29), 41% (95% CI 23.5–61.1%) of patients had decreased renal function.
Conclusions: A substantial portion of NAC-administered patients who developed TEEs had reduced renal function and would have been less likely to have benefited from renal clearance-dependent LMWH prophylaxis.
AS-11.116
A Retrospective Analysis of the De Ritis Ratio in Muscle Invasive Bladder Cancer, with Focus on Tumor Response and Long-Term Survival in Patients Receiving Neoadjuvant Chemotherapy and in Chemo Naïve Cystectomy Patients
Eriksson V1, Holmkvist O1, Huge Y2, Johansson M1,3, Alamdari F4, Svensson J5, Aljabery F2, Sherif A1
1Umeå university, Department of Surgical and Perioperative Sciences, Urology and Andrology, Umeå, Sweden, 2Linköping university, Department of Clinical and Experimental Medicine, Division of Urology, Linköping, Sweden, 3Länssjukhuset Sundsvall/Härnösand, Urology, Sundsvall, Sweden, 4Västmanland Hospital, Department of Urology, Västerås, Sweden, 5Umeå university, Department of Statistics, Umeå School of Business, Economics and Statistics (USBE), Umeå, Sweden
Background: A high pre-treatment De Ritis ratio, the aspartate transaminase/alanine aminotransferase ratio, has been suggested to be of prognostic value for mortality in muscle invasive bladder cancer (MIBC). Our purpose was to evaluate if a high ratio was associated with mortality and downstaging.
Methods: A total of 347 Swedish patients clinically staged T2-T4aN0M0, with administered neoadjuvant chemotherapy (NAC) or eligible for NAC and undergoing radical cystectomy (RC) 2009–2021, were retrospectively evaluated with a low ratio < 1.3 vs. high ratio > 1.3, by Log Rank test, Cox regression and Mann–Whitney U-test (MWU), SPSS 27.
Results: Patients with a high ratio had a decrease of up to 3 years in disease-free survival (DFS), cancer-specific survival (CSS) and overall survival (OS) (p=0.009, p=0.004 and p=0.009) and 5 years for CSS and OS (p=0.019 and p=0.046). A high ratio was associated with increased risk of mortality, highest for DFS (HR, 1.909; 95% CI, 1.265–2.880; p=0.002). No significant relationship between downstaging and a high ratio was detected (p = 0.564 MWU).
Conclusions: A high pre-treatment De Ritis ratio is, on a population level, associated with increased mortality post-RC in endpoints DFS, CSS and OS. Associations decrease over time and require further investigations to determine how strong the associations are as meaningful prognostic markers for long-term mortality in MIBC. The ratio is not suitable for downstaging-prediction.
AS-11.117
Mitochondrial DNA mutations in urine as a biomarker for urinary bladder cancer
Schwenke B L L1, Arstad C1, Müller S1, Ekstrøm P O2
1Akershus University Hospital, Urological department, Nordbyhagen, Norway, 2Oslo University Hospital - Det Norske Radiumhospitalet; Institute for cancer research, Department of tumor biology, Oslo, Norway
Background: Urinary bladder cancer is the 10th most common cancer disease globally. In most non-muscle-invasive bladder cancers both primary diagnosis and subsequent follow up for multiple years include cystoscopies, CT scans and urine cytology. In total this constitutes an invasive and cost intensive program. Mitochondria are the metabolic and energetic power hub of the cells, with their own circular DNA. Cancer cells regularly have mitochondrial dysfunctions with detectable mitochondrial DNA mutations. The hypothesis of this study is that mitochondrial DNA mutations in exfoliated urinary urothelium cells in the urine can be used as a biomarker for bladder cancer. This marker could potentially be a tool in primary diagnosis and follow-up of non-muscle invasive bladder cancer.
Methods: The preliminary results of this pilot study consists of mutation analysis of mitochondrial DNA, in cells isolated from urinary samples before surgery, tissue biopsies from the tumor and endoscopic normal tissue retrieved during the transurethral resection. For further analysis urine will be sampled during the first year of follow up. Extracted and amplified mitochondrial DNA in mutational hot spots were analyzed for mutations by the method of cycling temperature capillary electrophoresis. Twenty-three patients with urinary bladder cancer were included in this pilot study, twenty-one of these with primary cancer.
Results: All patients had transitional cell carcinoma, four of these had variant histology. Mitochondrial DNA mutations both in the urinary sample and in tumor tissue were found in six patients. Mitochondrial DNA mutations in tumor tissue only were identified in an additional ten patients.
Conclusions: Mitochondrial DNA mutations could represent a biomarker for urinary bladder cancer. This biomarker should potentially reduce discomfort and cost in primary diagnosis and follow-up of bladder cancer patients. Further analysis of the urine after tumor resection are planned.
AS-11.118
Intracavitar BCG instillation for Upper urinary Tract Urothelial Carcinoma
Knobloch C F1, Plathan M L1, Carlsen B2, Haug E S1
1Vestfold Hospital Trust, Urological, Tønsberg, Norway, 2Vestfold Hospital trust, Pathology, Tønsberg, Norway
Background: High-grade urothelial cancer (UTC) in the upper urinary tract (UTUC) is a serious condition that according to guidelines demands Nephro-ureterctomy (NU) in most cases. In patients with single kidney or bilateral disease, nephron-sparing alternatives are wanted. BCG has proven to reduce recurrence and to some extent progression of UTC, but evidence is based on Non-Muscle Invasive Bladder Cancer. Although there is guidelines for adjuvant instillation in the bladder for UTUC, data on efficacy and methods for intracavitar BCG (IC-BCG) treatment in the upper tract is lacking. We will present our experience IC-BCG treatment for UTUC and different methods for IC-BCG instillation.
Methods: Patients treated with IC-BCG for UTUC 2016-2021 were identified in our local registry and medical record assessed. All patients were treated for Carcinoma in Situ and surveillance included urine cytology. Depending on the accessibility of the upper tract, protocols both for deposal by intraluminal urethral stents and by nephrostomy tubes were used.
Results: Three patients and four treatments were identified; two treatments were given before, and two after radical cystectomy (RC). Follow-up from last treatment range from one to two years. The patients received from 10 to 12 IC-BCG. In one patient, it was stopped due to recurring urinary infections. Two treatments were distributed by stents through ileal conduit and two by nephrostomies - one bilateral.UTUC recurrence has occurred in two patients. One patient treated unilateral 2016, was retreated 2020, and is progression free at FU. One patient underwent RC and orthotopic neobladder after treatment due to bladder recurrence and one patient has died from UTUC.
Conclusions: IC-BCG is a feasible but resource-intensive alternative to NU and dialysis in informed patients. Eligible patients may often have pan-UTC, and if prolonging IC-BCG up to 3 years can improve RFS is not known.
AS-11.119
Urinary diversions (UD) for benign conditions- retrospective study of a 10-year cohort at Haukeland University Hospital (HUH)
Haugland J N1, Bergesen A K1, Roth I1, Hjelle K M1,2, Beisland C1,2, Gudbrandsdottir G1,2
1Haukeland University Hospital, Urology, Bergen, Norway, 2University of Bergen, Clinical Medicine, Bergen, Norway
Background: The number of patients requiring a urinary diversion (UD) for benign indication at our institution seems to have increased over the last decade. Thus, we aimed to evaluate practice patterns and surgical treatment options for UD with or without cystectomies for benign conditions at our tertiary referral center.
Methods: All patients who underwent a UD due to benign conditions at HUH from 2013 to 2022 are included. Data on 72 consecutive patients were retrieved from the medical records regarding patient characteristics, symptoms, indications and type of diversion. The study period was divided into early and later period (2013-2017 vs.2018-2022).
Results: Median age at surgery was 61 (IQR 42-71) years. Male to female ratio was 1:1. Diversion was offered as last resort due to painful bladder in 11, neurogenic bladder in 25 (i.e. Multiple sclerosis, spinal cord injury, spina bifida), sequela from radiotherapy in 25 or due to other causes in 16 patients. Urinary incontinence was a dominating symptom in 58 % of the cases, pain in 39%, and overactive bladder in 17%. Three or more symptoms were reported by 60% of the patients. Fistulas were reported in 17%. Forty eight patients needed a catheter before UD (transurethral 30%, suprapubic 38%, CIC 21% and nephrostomy 11%). Seven patients had more than one catheter.The majority of the UD was ileal conduit (90%) and the remainder a continent reservoir (Lundiana pouch). Synchronous cystectomy was performed in 34, and deferred cystectomy in two patients. Eighteen patients had concomitant procedures (i.e. colostomy (n=14)). An increased number of UD was performed in the late vs. the early period (p<0.001). Likewise, more patients had a UD due late-effects of radiotherapy in the later period (p<0.001).
Conclusions: During the study period, we performed more UD for benign conditions. Our impression is that more patients require UD because of urological complications after radiotherapy. The latter will need further attention.
AS-11.120
Robotic assisted Y-V plasty for bladder neck sclerosis – a case report
Roaldsen M, Aarsæther E
University Hospital of North Norway, Department of Urology, Tromsø, Norway
Background: Bladder neck sclerosis following transurethral resection of the prostate is a well-known complication with a reported incidence of 1-12%. Retrograde endoscopic treatment strategies are usually first choice, but may not always succeed. Patients considered resistant to transurethral management of bladder neck sclerosis may be offered an Y-V plasty of the bladder neck. Robotic assisted Y-V plasty was previoulsy reported by Granieri et al with excellent results. Our first experience with robot assisted Y-V plasty is presented as a case report.
Methods: The patient is a 66-year-old male who was admitted to his local hospital in 2020 with acute urinary retention, sepsis and hydronephrosis. Ultrasound revealed a 34 mL sized prostate. Uroflowmetry showed a maximum flow rate of 15 ml/s and a post void residual volume of 73 ml. He was later referred to transurethral resection of the prostate, which was completed the same year. A year later the patient was diagnosed with bladder neck sclerosis, which was subsequently treated with a transurethral incision. The bladder neck sclerosis recurred three months later. The patient then underwent another unsuccessful attempt at transurethral incision before he was referred to our clinic for a second opinion. Preoperative assessment with urethrography and urethroscopy demonstrated a narrow, 1,5 mm lumen with a length of 2 cm.
Results: The patient underwent robotic assisted Y-V plasty with a transperitoneal approach. Operative time was 80 minutes and length of stay was 2 days. A cystography was performed before catheter removal after 16 days. Uroflowmetry after surgery demonstrated a maximum flow rate of 26 ml/s and a post void residual volume of 33 ml. Urethrography and cystoscopy after three months revealed satisfactory results.
Conclusions: Robotic assisted Y-V plasty may be a feasible alternative to patients with bladder neck sclerosis resistant to transurethral incision.
AS-11.121
Severe complication in a patient with artificial urinary sphincter following treatment for prostate cancer – a case report
Nilsen O J
Oslo University Hospital, Department of Urology, Oslo, Norway
Background: Stress urinary incontinence (SUI) is a well-known sequela after treatment for prostate cancer. A common treatment for patients with debilitating SUI is implantation of an artificial urinary sphincter (AUS). It is shown that patients with a history of radiotherapy have a higher risk of complications after prostatectomy and after implantation of an AUS. We present a case report illustrating the possibility of severe complications in these patients.
Methods: Presentation of a case report.
Results: At the age of 72, the patient was operated with robot assisted radical prostatectomy (RARP) for a pT2c, Gleason 8 tumour. Due to positive margins and lymph nodes, he also received adjuvant radiotherapy. 19 months after RARP, in 2017, he was offered an AUS due to bothersome leakage of up to 500 grams per day. Preoperative cystometry showed reduced bladder capacity of 220 ml and terminal detrusor overactivity. After implant, he still had some leakage and was treated with mirabegron. In 2019 a TUR-B was done due to PUNLMP. He has also had several transurethral endoscopic treatments of calcifications in the bladder neck and anastomosis.
He had another TUR-B December 2022. In February 2023 he was admitted with sepsis of unknown origin. After a few days, local symptoms was showing in the scrotum, he reported pneumaturia and a CT scan showed abscess around the AUS and possibly rectovesical fistula. He was transferred to our department and operated the same day. Infection and faecal content were found around all parts of the AUS. The AUS was removed extraperitoneally and laparoscopic sigmoidostomy was done in the same session. He is recovering, but still not fit for major surgery (e.g., ileal conduit).
Conclusions: Patients treated with both radiotherapy and surgery for prostate cancer have increased risk of complications after implantation of an AUS. Patients should be informed accordingly and physicians should suspect infection of the implant in patients presenting with infections.
AS-11.122
Penile plication surgery a single surgeon series
Hopland-Nechita F V1,2, Hustveit F1, Dalin M1, Borkhus T1, Øverland G B1
1Førde Central Hospital, Surgical Department, Førde, Norway, 2University of Bergen, Department of Clinical Medicine, Bergen, Norway
Background: Tunical shortening procedures are the first treatment option for Peyronie’s disease with adequate penile length and absence of complex deformities (hourglass or hinge). Penile plication techniques are among the most used in this category. The aim of this study is to present the single surgeon experience with penile plication over the last 5 years.
Methods: The study is the retrospective analysis of the patients treated during 2018 to 2022. All patients were primary operated with penile plication. We excluded reoperations. From the medical records (search criteria was ICD code - KGH20) data was collected regarding age, comorbidities, angle of curvature, technique of plication, operative time, complications, and failures. Pictures data (pre- and post-surgery) were reviewed whenever available.
Results: In total 71 patients were identified. The most used technique was “16-dot” technique. Medium angle of curvature 46.5 degrees dorsally and 30 degrees laterally. 12 patients had curvature in more than one axis. Mean operative time was 36,4 min. Seven patients had failure of plication (four treated with re-do plication and three with grafting). Four patients presented with wound dehiscence which required secondary suture. Technical modifications were implemented to improve the results after visits to referral hospital and discussions with more experience surgeons.
Conclusions: Penile plication is a relatively simple surgical technique but requires attention to details for optimal results. Short visits to referral hospitals are strongly recommended to refine the technique.
AS-11.123
Urethroplasty for Bulbar Urethral Strictures: Results from a Low-Volume Center
Pasovic L1, Løvvik A1, Müller S1,2
1Akershus University Hospital, Department of Urology, Lørenskog, Norway, 2University of Oslo, Faculty of Medicine, Oslo, Norway
Background: We present the six-year results of urethroplasty for bulbar urethral strictures using either a buccal mucosal graft (BMG) or primary end-to-end anastomosis (PA) from a low-volume center.
Methods: Urethroplasty for bulbar urethral stricture was performed in 29 patients in the period 2016-2022. Retrograde urethrography established the diagnosis. Median patient age was 36 years (range 17-78 years). Patients were subjected to either BMG or PA according to surgeon’s preference. A foley catheter was placed for two weeks postoperatively with antibiotic prophylaxis, upon which retrograde urethrography was performed to exclude anastomosis leakage. Follow-up was scheduled at 3 and 12 months and included flowmetry and residual volume investigations.
Results: A total of 23 patients (79 %) received a BMG, while six patients (21 %) received a PA. A majority (59 %) were previously treated with internal urethrotomy. Median stricture length determined by retrograde urethrography was 12 mm (range 2-30 mm). The etiology was idiopathic in 79 %, followed by perineal trauma in 17 %. Voiding qMax determined by flowmetry improved from a preoperative mean of 7,1 ± 3,2 mL/s to a postoperative mean of 25,0 ± 9,4 mL/s (P < 0.0001). Residual volume improved from a preoperative mean of 102 ± 101 mL to a postoperative mean of 45 ± 32 mL (P = 0.052). Postoperative contrast leakage was observed in one patient (3.4 %) and subsided spontaneously. Three patients (10,3 %) experienced minor postoperative complications. Recurrence was noted in four patients (13,8 %; 8 % in the BMG group and 33 % in the PA group, respectively).
Conclusions: The results show significant improvement in postoperative flowmetry. Complication and recurrence rates are comparable to that reported from high-volume centers, suggesting that urethroplasty can be considered safe and effective also in a low-volume center.