ORIGINAL RESEARCH ARTICLE
National trends of surgery for benign prostatic hyperplasia in Finland
Alisa Salmivalli, M.D.a,b,c , Peter J. Boström, M.D., Ph.D.c
, Peter J. Boström, M.D., Ph.D.c , Pertti Nurminen, M.D., Ph.D.c
, Pertti Nurminen, M.D., Ph.D.c , Pekka Kinnala, M.D., Ph.D.c
, Pekka Kinnala, M.D., Ph.D.c , Ville Kytö, M.D., Ph.D.d,e
, Ville Kytö, M.D., Ph.D.d,e and Otto Ettala, M.D., Ph.D.c
and Otto Ettala, M.D., Ph.D.c
aDoctoral Programme in Clinical Research, University of Turku, Turku, Finland; bDepartment of Urology, Satasairaala Central Hospital, Wellbeing Services County of Satakunta, Pori, Finland; cDepartment of Urology, Turku University and Turku University Hospital, Turku, Finland; dHeart Center, Turku University Hospital and University of Turku, Turku, Finland; eResearch Services, Wellbeing Services County of Southwest Finland, Turku, Finland
ABSTRACT
Purpose: To investigate national trends of surgical treatment for benign prostatic obstruction (BPO).
Methods: The Care Register for Healthcare in Finland was used to investigate the annual numbers and types of surgical procedures, operation incidence and duration of hospital stay between 2004 and 2018 in Finland. Procedures were classified using the Nordic Medico-Statistical Committee Classification of Surgical Procedures coding. Trends in incidence were analyzed with two-sided Cochran-Armitage test. Trends in duration of hospital stay and patient age were analyzed with linear regression.
Results: Transurethral resection of the prostate (TURP) was the most common operation type during the study period, covering over 70% of operations for BPO. Simultaneous with the implementation of photoselective vaporization of the prostate (PVP), the incidence of TURP, minimally invasive surgical therapies, transurethral vaporization of the prostate (TUVP) and open prostatectomies decreased (p < 0.05). The mean operation incidence rate in the population between 2004 and 2018 was 263 per 100,000. The duration of hospital stay shortened (p < 0.05), and the average age of operated patients increased by 2 years (p < 0.0001).
Conclusion: The implementation of PVP did not challenge the dominating position of TURP in Finland, but it has probably influenced the overall use of other surgical therapies, excluding transurethral incision of the prostate. The results might suggest that the conservative treatment is accentuated, patient selection is more thorough, and surgical intervention might be placed at a later stage of BPO.
KEYWORDS: Benign prostatic obstruction; national trends; transurethral resection of the prostate; photoselective vaporization of the prostate; incidence
Citation: Scandinavian Journal of Urology 2024, VOL. 59, 70–75. https://doi.org/10.2340/sju.v59.32425.
Copyright: © 2024 The Author(s). Published by MJS Publishing on behalf of Acta Chirurgica Scandinavica. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material, with the condition of proper attribution to the original work.
Received: 28 November 2023; Accepted: 21 March 2024; Published: 22 April 2024
CONTACT Alisa Salmivalli aaksal@utu.fi Department of Urology, Turku University Hospital, P.O. Box 52, FIN-20521 Turku, Finland.
Supplemental data for this article can be accessed online at https://doi.org/10.2340/sju.v59.32425
Competing interests and funding: The authors declare that there are no conflicts of interest.
This work was supported by Paavo Nurmi foundation, State Research Funding, Finnish Foundation for Cardiovascular Research and Turku University Hospital Foundation.
Introduction
Lower urinary tract symptoms (LUTS) remain a common burden to aging males. Despite the release of α1-blocker and a 5α-reductase inhibitor combination drugs, surgical procedures are still often necessary for LUTS resulting from benign prostatic obstruction (BPO) [1]. While transurethral resection of the prostate (TURP) remains the gold standard of surgical treatment, several other transurethral ablative techniques are commonly in use [2]. Among these techniques are transurethral vaporization of the prostate (TUVP) and photoselective vaporization of the prostate (PVP) for men with prostate size 30–80 ml, transurethral incision of the prostate (TUIP) for men with prostate size <30 ml, and open prostatectomy for men with prostate volume over 80 ml [2]. Transurethral microwave thermotherapy (TUMT) and transurethral needle ablation (TUNA) have also been alternative treatment options for men with prostate volume 30–80 ml [1]. Open prostatectomy, the oldest surgical treatment for BPO, has maintained its place due to its effectiveness and durability in use with patients having large prostates, but it is becoming less common [2, 3]. The role of other surgical therapies for the treatment of BPO in Finland has been unclear – especially after the adaptation of PVP, which has been demonstrated to be safer when operating at-risk patients [2, 4, 5]. TUIP is recommended for relieving LUTS in patients with moderate-to-severe LUTS in smaller prostates without a middle lobe [2]. TUVP has been used as an alternative for monopolar TURP, and it seems to have a favorable peri-operative profile but inferior mid-term efficacy [2]. TUMT has been indicated as a relatively safe treatment option that can be performed as an outpatient procedure [6]. TUNA is one of the less invasive procedures that can improve BPO symptoms, but it does not achieve the same level of efficacy as TURP [7]. It is unclear if various surgical therapies are needed, especially when the nature of many minimally invasive modalities is still experimental due to a lack of evidence of their efficacy [1, 8]. Moreover, PVP offers shorter catheterization times, perioperative safety and functional results similar to TURP [2, 9]. The present study aimed to describe possible changes in usage rates of various surgical procedures for BPO in Finland, considering the introduction and adaptation of PVP.
Materials and methods
The Care Register for Healthcare in Finland was used to obtain the numbers of elective BPO surgical procedures performed annually between 2004 and 2018 in Finland. Procedures were classified using the Nordic Medico-Statistical Committee Classification of Surgical Procedures coding as TURP (KED22), Open (KED00, KED10), PVP (KED52), TUIP (KED33), TUMT (KED72), TUNA (KED62), TUVP (KED76) and Other (KED96 and KED98). The first operation for each patient per study year was included. If multiple operational codes were available during the same treatment period, only the most significant of operations was included, and the classification was concluded in consensus of the authors (classification from the least to most significant: Other, TUVP, TUMT, TUNA, TUIP, TURP, Laser, Open). Patients with urologic malignancy or neoplasm and under 40 years of age were excluded. Procedures administered as an emergency operation were also excluded. Detailed exclusions of ICD10 codes are available in Table S1. Age groups were categorized as 40–49, 50–59, 60–69, 70–79, 80–89 and >90 years. Postsurgical length of stay was at least 1 day, meaning length of stay was 1 day in same-day discharge and in outpatient procedures.
This study was based on a nationwide administrative database of the Finnish Institute for Health and Welfare [10]. The data of annual surgical procedures and hospital admissions were obtained from the National Institute for Health and Welfare of Finland (permission no: THL/2245/5.05.00/2019). Annual population data were obtained from Statistics Finland (TK-53-484-20).
The primary objective was to determine national trends of surgical procedures for the treatment of BPO. The secondary objective was to determine operation incidence in the population and postsurgical length of stay. Year and age-specific mean operation incidence was calculated by dividing the number of age-group operations by same-aged population while assuming that the entire male population of Finland was at risk during that period. The overall mean operation incidence was calculated by dividing the number of all operations by the male population of Finland aged 40 years or older during the study period. The relative proportion of certain operation types was calculated by dividing the number of the specific operation by the number of overall operations during the same period. Trends in incidence were analyzed with two-sided Cochran-Armitage test. Trends in duration of hospital stay and patient age were analyzed with linear regression. Statistical significance was inferred at P-value < 0.05. SAS ver 9.4 was used for analyses.
Results
A total of 64,117 operations were performed between 2004 and 2018 in Finland. After exclusions based on previously descriped criteria, 52,761 patients were included in the study population. The baseline features of study population are available in Table 1. During the study period, 39,333 TURP, 6,220 PVP, 4,499 TUIP, 1,204 open prostatectomy, 742 TUVP, 580 TUMT, 65 TUNA and 118 other partial excision of prostate procedures were performed. TURP was the most common operation type for all age groups. During the study period, the relative proportion of TURP decreased from 80% to 72%, while the proportion of PVP increased from 0.1% to 16%, reaching its peak at 18% in 2013. The relative proportion of TUNA decreased from 0.8% to 0.2%, TUVP from 3.6% to 0.5%, TUMT from 2.7% to 0.6%, open prostatectomies from 3.3% to 2.0% and other partial excisions from 0.2% to 0.0%. The relative proportion of TUIP procedures decreased from 9.7% in 2004 to 7.4% in 2007 and 2008. Thereafter, the proportion of TUIP reascended to 8.8% in 2018. The trend of annual procedure numbers is presented in Figure 1.
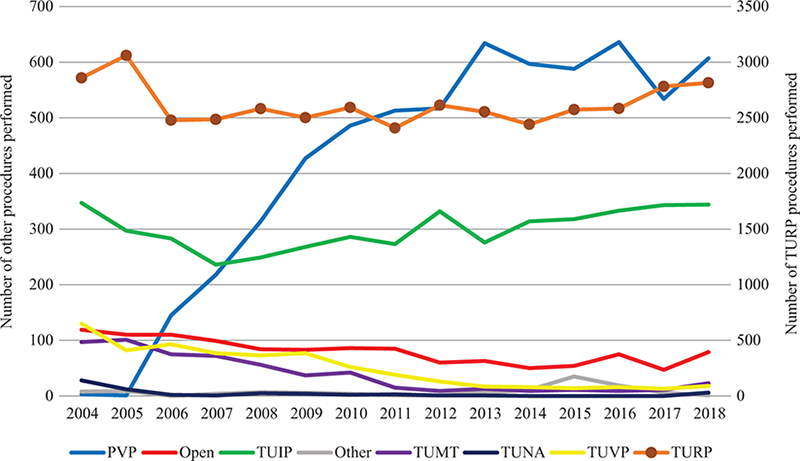
Figure 1. Surgical procedures for benign prostatic obstruction by year.
The primary Y axis on the left-hand side acts as the scale for PVP, Open, TUIP, Other, TUMT, TUNA and TUVP. The secondary Y axis on the right-hand side acts as the scale for TURP.
The mean operation incidence rate in the population between 2004 and 2018 was 263 per 100,000 (standard deviation [SD] 12.2). The overall operation incidence rate did not change significantly during the study period (trend p = 0.5044). There was a significant decrease (trend p < 0.05) in trend of incidence in TURP, Open, TUVP, TUMT, TUNA and Other operations, while the incidence of PVP increased significantly (trend p < 0.0001). Operation incidence decreased significantly also in all other age groups than the age group of men 40–49 and >90 years. The operation incidence between 2004 and 2018 was highest for the age groups of men 70–79 (737 per 100,000) and 80–89 years old (739 per 100,000) and lowest for the age group of men 40–49 (11 per 100,000). The Trend p values of incidence are available in Table S2. The annual operation incidence rate per 100,000 by age-groups is presented in Figure 2.
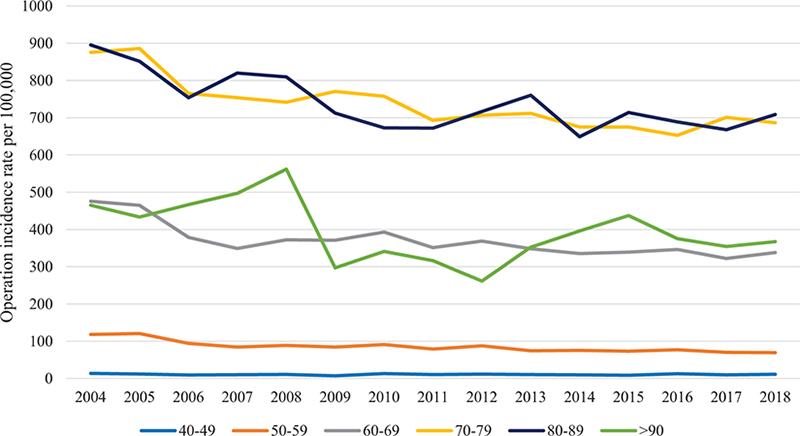
Figure 2. Annual operation incidence rate per 100,000.
The postsurgical length of stay shortened during the study period for all procedure types and all age groups (p < 0.05). The hospital stay was longest for patients that underwent open prostatectomy (mean 8.1 days, SD 3.0), and shortest for those that underwent TUMT (mean 1.1 days, SD 0.2). The mean hospital stay after TURP was 4.0 days (SD 2.1) and after PVP 2.3 days (SD 1.5). In the age group of >90 years, the mean hospital stay was 7.0 days (SD 3.2) in 2004, which decreased to 3.2 days (SD 1.6) in 2018. The shortest hospital stays were for the age group 40–49 years old, and the mean duration decreased from 3.6 days (SD 1.7) in 2004 to 2.4 days (SD 1.1) in 2018. The trend of mean duration of hospital stay for procedures with N > 1,000 and for all age groups is presented in Figure 3. The p values and parameter estimates of postsurgical length of stay are available in Table S3.
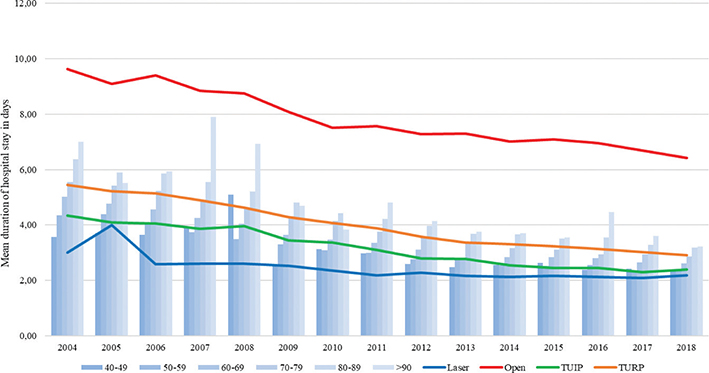
Figure 3. Mean duration of hospital stay in days.
The mean age of all operated patients increased from 69.6 (SD 9.1) to 71.8 (SD 8.5) years during the study period (p < 0.0001). The mean age increased significantly in all other operation types than TUVP. The mean age of patients that underwent PVP was 70.6 (SD 8.6), open prostatectomy 72.6 (SD 7.3), TUIP 67.5 (SD 11.0), TURP 70.9 (SD 8.5), TUVP 72.4 (SD 8.5) and other partial excision of the prostate 71.8 (SD 9.0). The mean age of patients was oldest in the TUMT group (mean age 75.3, SD 8.9) and youngest in the TUNA group (mean age 64.4, SD 11.1). The p values and parameter estimates of mean age are available in Table S4.
Discussion
In this population-based study of 52,761 patients, we aimed to examine the changes in usage rates of various surgical procedures for BPO in Finland. During the study period (2004–2018), TURP was by far the most common operation type for BPO in Finland. Simultaneous with the adaptation of PVP, the relative proportion of TURP decreased by 7.3%, and the proportion of minimally invasive surgical therapies, TUVP and open prostatectomies also decreased, while the relative proportion of TUIP procedures remained the same. The incidence of surgical treatment for BPO did not alter significantly, the duration of hospital stay shortened and the average age of operated patients rose by 2 years.
During the study period, we observed that the initial enthusiasm of PVP waned and the operation levels stabilized. The first-generation (80-W) PVP was launched in Finland in 2006 and was found to be a safe technique with excellent hemostatic properties, but the extent of tissue removal was considered insufficient [11]. In its launch year, there were 145 PVP operations in Finland, and the number increased steadily thereafter until 2013. During this period of increased PVP procedures, the second generation, 120-W high-performance system, was launched in 2007 and the third generation, 180-W XPS laser system, in 2010. The second-generation PVP provided better intraoperative and early postoperative outcomes but more storage bladder symptoms in comparison to TURP [12, 13]. The 180-W XPS laser, which represents the current standard for PVP, offers shorter operation times, with prostate volume reduction and functional results comparable to TURP [2, 9]. However, initial reports of higher reoperation rates and poorer reductions in prostate volume [12, 14–16] probably stalled the excitement around PVP. The increasing trend of operation numbers halted in 2013 and stayed at approximately 600 operations per year thereafter.
Similar, but much steeper, trends concerning TURP and PVP were reported in two different studies in Australia, as well as in France. In Australia, Patel and Bariol reported that the number of TURP procedures declined from 96% to 73% while PVP treatment increased from 3.4% to 20% between 2008 and 2014, after which there was a slight decline of PVP procedures over the next 3 years [17]. Morton et al. reported that TURP remained the most commonly performed procedure, although its rate declined from 76% to 61%, while the use of PVP increased between 2000 and 2018 in Australia [18]. The authors also reported that the use of open prostatectomies was originally low and declined further, while TUIP remained relatively stable [18], which concurs with the current study. Peyronnet et al. described, in their research letter, that while the overall number of BPO surgical procedures in France remained stable, the share of PVP dramatically increased from 0.2% to 23%, while there was a 34% reduction in the number of TURP and open prostatectomies during the study period 2005–2014 [19]. Similar trends have also been reported in the US and Canada [20–22]. In the current study, the 7.3% decrease in the relative proportion of TURP is moderate compared to the rates reported in Australia, France, the US and Canada. Still, TURP remained the most commonly performed procedure for BPO in these studies, as in the current study [17–22].
The proportion of minimally invasive therapies and TUVP was low at the outset of the current study but continued to decrease during the study period, probably partially due to PVP adaptation. Another reason for this decrease might be due to the evolution of BPO treatment options. Even though TUMT is a true outpatient procedure, as also seen in the current study, its practical considerations are thin, and the latter also applies to TUNA [1]. Both techniques were considered in the 2013 European Association of Urology guidelines but are absent from the current guidelines [1, 2]. However, a more recent high-energy TUMT might serve as an outpatient alternative for treatment of large glands, but further studies are still necessary [23]. TUVP, on its own, is also a disappearing technique due to its inferior efficacy [2], but it might have a purpose of use in hemostasis after TURP.
In the current study, the mean operation incidence rate in the population between 2004 and 2018 was 263 operations for BPO per 100,000 men. This is remarkably higher than the incidence reported in Australia during almost the same period but lower than that reported in the US. In Australia, the operation incidence was rising, from 106 to 147 per 100,000 between 2000 and 2018 [18]. Meanwhile a declining incidence trend was reported in the US: Malaeb et al. found that the total rate of operations for BPO peaked in 2005 at 1,078 per 100,000 and declined by 15.4% in 2008 [22]. While the number of overall operations increased from 3,591 to 3,893 operations per year in the current study, the operation incidence did not alter significantly. This might have been caused by demographic changes: the number of men over 40 years old in Finland grew by 150,000 during the study period, and decreasing operation incidence trend was visible in the most growing age-groups of men (50–59, 60–69, 70–79 and 80–89 years old), but not in the age-groups of men 40–49 or over 90 years old. The major differences in reported incidence in earlier studies is at least partly explained by the datasets used. While Morton et al. used a dataset that comprised mostly of benign prostatic hyperplasia–related surgeries in Australia, it did not include public in-hospital data and therefore reflected only the private usage of these procedures, similar to the Medicare dataset of Malaeb et al.’s study in the US [18, 22]. A major difference between the aforementioned and the current study is the use of a truly nationwide dataset of previously validated mandatory-by-law register [24]. If the incidence of LUTS in Finland is presumed to be 15 per 1,000 men, as reported in the Triumph Project [25], 18% of patients with LUTS received surgical treatment. This rate is slightly lower than that reported in Korea (21%) [26].
During the study period, we observed a shortening of postsurgical length of hospital stay for all procedure types and all age groups. Still, in our opinion, the mean hospital stay was surprisingly long after TURP (4.0 days) and open prostatectomy (8.0 days) when compared to PVP (2.3 days). TUMT was the only true outpatient procedure, as previously mentioned (1.1 days). The mean difference in length of hospital stay between TURP and PVP was similar to that reported by Thangasamy et al. [27], but hospital stay after TURP was longer than that reported in Treharne et al.’s meta-analysis (2.87–3.43) [28]. At the same time (2000–2008), in the US, most TURP procedures required a postsurgical hospital stay, but there was a gradual increase in outpatient TURP procedures, and over 60% of PVP procedures were administered as an outpatient operation [22]. Shortening the postsurgical length of hospital stay brings economic advantage and is possibly a partial reason for the initial enthusiasm around PVP [27]. However, further cost effectiveness analysis should also take possible complications and especially reoperation rate into consideration [4]. All in all, same-day discharge after surgical treatment for BPO is probably becoming increasingly popular for selected patients, considering the publication of further studies of the safety of such an approach [29]. The mean age of all operated patients increased by 2 years to 71.8 at the end of the study period. The mean age rose for all procedures, except for the TUVP group. Similar to the current study, the highest BPO procedure numbers have been seen for age group 70–75 in other studies [21, 22], but interestingly, the operation incidence was almost identical for age groups 70–79 and 80–89 years in the current study.
There are strengths and limitations to the current study. The main focus of this retrospective study was to analyze national trends in surgery for benign prostatic hyperplasia, and the use of a nationwide, previously validated, mandatory-by-law register is a major strength of this study [24]. A general limitation is the lack of detailed patient data, and due to the nature of the Nordic Medico-Statistical Committee Classification of Surgical Procedures coding, we were unable to differentiate bipolar and monopolar TURP and categorize the three generations of PVP. Also, we are aware of new arising techniques, such as minimally invasive simple prostatectomy, aquablation, prostatic artery embolization, convective water vapor energy ablation and prostatic urethral lift [2]; but since these were not performed in Finland during the study period, we did not discuss these in the current study.
In conclusion, the implementation of PVP did not challenge the dominating position of TURP in Finland, but it has probably influenced the overall use of other surgical therapies, excluding transurethral incision of the prostate. The overall number of surgical procedures for BPO is rising, while patients are getting older and postsurgical length of stay is shortening. The results of this study might suggest that the conservative treatment is accentuated, patient selection is more thorough, and surgical intervention might be placed at a later stage of BPO.
Acknowledgments
Mr. Mikael Högerman is acknowledged for technical assistance.
Data availability statement
The data that support the findings of this study were obtained from the National Institute for Health and Welfare of Finland (permission no: THL/2245/5.05.00/2019). Restrictions apply to the availability of these data, which were used under license for this study. Data are available from the National Institute for Health and Welfare and Statistics Finland for those fulfilling the legal requirements for data access.
References
- [1] Oelke M, Bachmann A, Descazeaud A, et al. EAU guidelines on the treatment and follow-up of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol. 2013;64:118–140. https://doi.org/10.1016/j.eururo.2013.03.004
- [2] Cornu JN, Gacci HHM, Herrmann TRW, et al. EAU guidelines on non-neurogenic male lower urinary tract symptoms (LUTS), incl. Benign Prostatic Obstruction (BPO). European Association of Urology. EAU Guidelines Office, Arnhem, the Netherlands; 2023.
- [3] Gilfrich C, Leicht H, Fahlenbrach C, et al. Morbidity and mortality after surgery for lower urinary tract symptoms: a study of 95 577 cases from a nationwide German health insurance database. Prostate Cancer Prostatic Dis. 2016;19:406–411. https://doi.org/10.1038/pcan.2016.33
- [4] Salmivalli A, Ettala O, Nurminen P, et al. Short- and long-term risks of photoselective laser vaporization of the prostate: a population-based comparison with transurethral resection of the prostate. Ann Med. 2023;55:1287–1294. https://doi.org/10.1080/07853890.2023.2192046
- [5] Salmivalli A, Ettala O, Boström PJ, et al. Mortality after surgery for benign prostate hyperplasia: a nationwide cohort study. World J Urol. 2022;40:1785–1791. href="https://doi.org/10.1007/s00345-022-03999-0
- [6] Hoffman RM, Monga M, Elliot SP, et al. Microwave thermotherapy for benign prostatic hyperplasia. Cochrane Database Syst Rev. 2007; 4.
- [7] Bouza C, López T, Magro A, et al. Systematic review and meta-analysis of Transurethral Needle Ablation in symptomatic benign prostatic hyperplasia. BMC Urol. 2006;6:1–17. https://doi.org/10.1186/1471-2490-6-14
- [8] Christidis D, McGrath S, Perera M, et al. Minimally invasive surgical therapies for benign prostatic hypertrophy: the rise in minimally invasive surgical therapies. Prostate Int. 2017;5:41–46. https://doi.org/10.1016/j.prnil.2017.01.007
- [9] Brunken C, Seitz C, Woo HH. A systematic review of experience of 180-W XPS GreenLight laser vaporisation of the prostate in 1640 men. BJU Int. 2015;116:531–537. https://doi.org/10.1111/bju.12955
- [10] Kauppila JH, Helminen O, Kytö V, et al. Short-term outcomes following minimally invasive and open esophagectomy: a population-based study from Finland and Sweden. Ann Surg Oncol. 2018;25:326–332. https://doi.org/10.1245/s10434-017-6212-9
- [11] Te AE, Malloy TR, Stein BS, et al. Impact of prostate-specific antigen level and prostate volume as predictors of efficacy in photoselective vaporization prostatectomy: analysis and results of an ongoing prospective multicentre study at 3 years. BJU Int. 2006;97:1229–1233. https://doi.org/10.1111/j.1464-410X.2006.06197.x
- [12] Al-Ansari A, Younes N, Sampige VP, et al. GreenLight HPS 120-W laser vaporization versus transurethral resection of the prostate for treatment of benign prostatic hyperplasia: a randomized clinical trial with midterm follow-up. Eur Urol. 2010;58:349–355. https://doi.org/10.1016/j.eururo.2010.05.026
- [13] Zang YC, Deng XX, Yang DR, et al. Photoselective vaporization of the prostate with GreenLight 120-W laser versus transurethral resection of the prostate for benign prostatic hyperplasia: a systematic review with meta-analysis of randomized controlled trials. Lasers Med Sci. 2016;31:235–240. https://doi.org/10.1007/s10103-015-1843-1
- [14] Bachmann A, Schürch L, Ruszat R, et al. Photoselective vaporization (PVP) versus transurethral resection of the prostate (TURP): a prospective bi-centre study of perioperative morbidity and early functional outcome. Eur Urol. 2005;48:965–972. https://doi.org/10.1016/j.eururo.2005.07.001
- [15] Hermanns T, Gross O, Kranzbühler B, et al. Ablative efficiency of 532-nm laser vaporization compared to transurethral resection of the prostate: results from a prospective three-dimensional ultrasound volumetry study. World J Urol. 2014;32:1267–1274. https://doi.org/10.1007/s00345-013-1203-3
- [16] Teng J, Zhang D, Li Y, et al. Photoselective vaporization with the green light laser vs transurethral resection of the prostate for treating benign prostate hyperplasia: a systematic review and meta-analysis. BJU Int. 2013;111:312–323. https://doi.org/10.1111/j.1464-410X.2012.11395.x
- [17] Patel RM, Bariol S. National trends in surgical therapy for benign prostatic hyperplasia in Australia. ANZ J Surg. 2019;89:345–349. https://doi.org/10.1111/ans.15016
- [18] Morton A, Williams M, Perera M, et al. Management of benign prostatic hyperplasia in the 21st century: temporal trends in Australian population-based data. BJU Int. 2020;126:18–26. https://doi.org/10.1111/bju.15098
- [19] Peyronnet B, Cornu J-N, Rouprët M, et al. Trends in the use of the green light laser in the surgical management of benign prostatic obstruction in France over the past 10 years. Eur Urol. 2015;67:1193–1197. https://doi.org/10.1016/j.eururo.2015.01.003
- [20] Schroeck FR, Hollingsworth JM, Kaufman SR, et al. Population based trends in the surgical treatment of benign prostatic hyperplasia. J Urol. 2012;188:1837–1841. https://doi.org/10.1016/j.juro.2012.07.049
- [21] LaBossiere JR, Wallis CJD, Herschorn S, et al. Surgical management of benign prostatic obstruction: 20-year population-level trends. Can Urol Assoc J. 2020;14:552–557. https://doi.org/10.5489/cuaj.6224
- [22] Malaeb BS, Yu X, McBean AM, et al. National trends in surgical therapy for benign prostatic hyperplasia in the United States (2000–2008). Urology. 2012;79:1111–1117. https://doi.org/10.1016/j.urology.2011.11.084
- [23] Stenmark F, Brudin L, Kjölhede H, et al. Treatment with CoreTherm in 570 patients with prostate volumes of 80–366 ml: an evaluation of short- and long-term retreatment risk. Scand J Urol. 2022;56:336–341. https://doi.org/10.1080/21681805.2022.2108139
- [24] Sund R. Quality of the Finnish Hospital Discharge Register: a systematic review. Scand J Public Health. 2012;40:505–515. https://doi.org/10.1177/1403494812456637
- [25] Verhamme KMC, Dieleman JP, Bleumink GS, et al. Incidence and prevalence of lower urinarytract symptoms suggestive of benign prostatic hyperplasia in Primary CareöTheTriumph Project. Eur Urol. 2002;42:323–328. https://doi.org/10.1016/S0302-2838(02)00354-8
- [26] Lee YJ, Lee JW, Park J, et al. Nationwide incidence and treatment pattern of benign prostatic hyperplasia in Korea. Investig Clin Urol. 2016;57:424–430.
- [27] Thangasamy IA, Chalasani V, Bachmann A, et al. Photoselective vaporisation of the prostate using 80-W and 120-W laser versus transurethral resection of the prostate for benign prostatic hyperplasia: a systematic review with meta-analysis from 2002 to 2012. Eur Urol. 2012;62:315–323. https://doi.org/10.1016/j.eururo.2012.04.051
- [28] Treharne C, Crowe L, Booth D, et al. Economic value of the transurethral resection in saline system for treatment of benign prostatic hyperplasia in England and wales: systematic review, meta-analysis, and cost–consequence model. Eur Urol Focus. 2018;4:270–279. https://doi.org/10.1016/j.euf.2016.03.002
- [29] Garden EB, Ravivarapu KT, Levy M, et al. The utilization and safety of same-day discharge after transurethral benign prostatic hyperplasia surgery: a case-control, matched analysis of a national cohort. Urology. 2022;165:59–66. ttps://doi.org/10.1016/j.urology.2022.01.037