SHORT COMMUNICATION
Langerhans Cell Histiocytosis Caused by Adalimumab for Crohn’s Disease: A Case Report
Mariko KOCHI and Tetsuya HIGUCHI
Department of Dermatology, Toho University Sakura Medical Center, 564-1 Shimoshizu, Sakura, Chiba 285-8741, Japan. E-mail: mariko.kochi@med.toho-u.ac.jp
Citation: Acta Derm Venereol 2023; 103: adv10285. DOI https://doi.org/10.2340/actadv.v103.10285.
Copyright: © Published by Medical Journals Sweden, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: Jun 7, 2023; Published: Jun 30, 2023
INTRODUCTION
Langerhans cell histiocytosis (LCH) is a disease that causes diverse clinical symptoms due to the monoclonal proliferation of atypical histiocyte-like cells that infiltrate the skin, bones, liver, spleen, and central nervous system. Paradoxical reactions that occur during treatment with biological agents are defined as the appearance or exacerbation of a pathological condition. Tumor necrosis factor-alpha (TNFα) inhibitors lead to skin manifestations such as psoriasiform rash and palmoplantar pustulosis. This study reports a patient with LCH that was induced by adalimumab, a fully human monoclonal antibody against TNFα, administered to treat Crohn’s disease.
CASE REPORT
A 32-year-old man diagnosed with Crohn’s disease via ileocolonoscopy (Montreal classification A2L3B1) was administered adalimumab (40 mg/week) and azathioprine (100 mg/day) for 4 years, during which he experienced no skin disease. However, 2 months prior to his presentation, red nodules appeared on the patient’s chest, abdomen, and thighs. He was referred to our department with a diagnosis of granuloma annulare. Physical examination revealed red nodules up to approximately 5 mm diameter on the patient’s chest, abdomen, and limbs. The patient’s gastrointestinal symptoms were controlled. Topical steroids and phototherapy were initiated, and the adalimumab was continued. The rash temporarily resolved, then gradually worsened to multiple aggregates up to approximately 10 mm diameter on the patient’s chest, abdomen, and limbs (Fig. 1a). The patient’s Crohn’s disease remained in remission. A skin biopsy of a red nodule on the left side of the patient’s chest revealed histiocyte-like cells with markedly enlarged and irregularly shaped nuclei infiltrating the dermis (Fig. 2a, b). Most histiocyte-like cells were positive for CD1a (Fig. 2c, d) and some cells were positive for S-100 protein. Therefore, the patient was diagnosed with LCH.
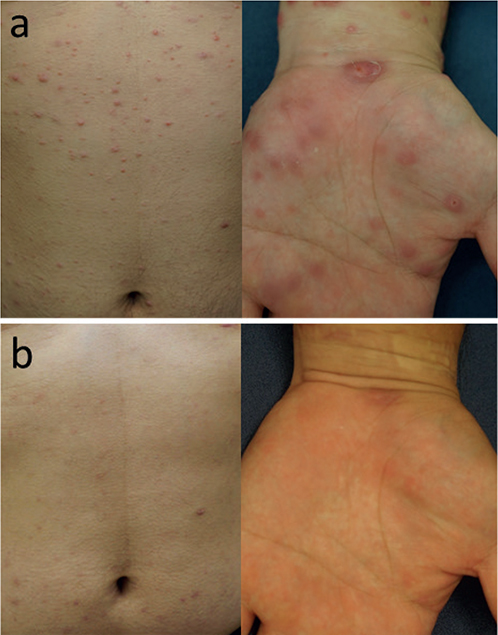
Fig. 1. Clinical photographs. (a) Red nodules up to approximately 10 mm diameter on the abdomen and left hand. (b) The nodules spontaneously resolved approximately 6 months after discontinuation of adalimumab.
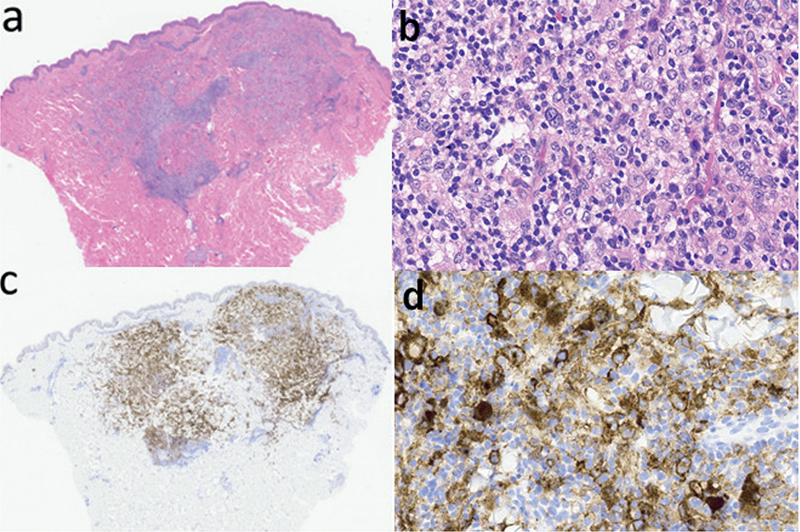
Fig. 2. Histopathology. Histiocyte-like cells with markedly enlarged and irregularly shaped nuclei infiltrated into the dermis (haematoxylin–eosin, original magnification (a) ×20; (b) ×400. Immuno-histologically, most histiocyte-like cells were positive for CD1a ((c) ×20; (d) ×400).
Computed tomography of the chest and abdomen was not suggestive of LCH in other organs, including the lungs and bones. Seven months after the initial examination, adalimumab was switched to vedolizumab (anti-α4 β7 integrin antibody) for the treatment of Crohn’s disease, and the rash spontaneously resolved approximately 6 months thereafter (Fig. 1b). The patient’s Crohn’s disease was subsequently controlled with vedolizumab and azathioprine therapy, with no relapse of the rash for over 1 year. The patient’s C-reactive protein level remained within the normal range.
DISCUSSION
LCH is a disease in which atypical histiocyte-like cells similar to Langerhans cells proliferate monoclonally and infiltrate the skin, bones, liver, spleen, and central nervous system, causing diverse clinical symptoms (1). Although LCH may occur in people of all ages, its incidence is 1 in 200,000 children and 1 in 500,000 adults (2). LCH is an inflammatory myeloid tumor with features of both tumors and inflammation. LCH is classified into the single-system single-site (SS), single-system multi-site (SM), and multi-system multi-site (MM) types based on the distribution of the affected lesions. LCH includes various conditions, ranging from those that spontaneously resolve without treatment to those that rapidly progress and are fatal. The treatment varies depending on the disease type. The SS type, which spontaneously resolves in some patients, is treated via resection of the lesions and with topical and locally-injected steroids. The SM and MM types are mainly treated via chemotherapy (3). Previous studies have reported patients with LCH localized to the skin, whose symptoms improved after oral thalidomide (4, 5). Thalidomide inhibits TNFα, which plays an important role in the differentiation of Langerhans cells from myeloid progenitors (5).
However, TNFα inhibitors, which are used to treat psoriasis, are associated with skin manifestations, including psoriasiform rash and palmoplantar pustulosis. This phenomenon is a paradoxical reaction. Increased production of interferon-alpha in plasmacytoid dendritic cells, which is inhibited by TNFα, results in a cytokine imbalance, initiating inflammation by T helper 1 cells (6). Although there are no reports of LCH induced by TNFα inhibitors, the aggravation of eosinophilic granuloma of the lung (a type of LCH) 3 months after the start of treatment with infliximab for ulcerative colitis has been reported (7).
An association between LCH and inflammatory bowel disease has been reported. Multisystemic LCH involving the colonic mucosa may be misdiagnosed as Crohn’s disease (8, 9). A case series of patients with LCH and Crohn’s disease has been reported (10). Therefore, LCH and Crohn’s disease must be diagnosed carefully using the patient’s histology and clinical course.
In this case, LCH was localized to the skin and occurred exclusively during adalimumab therapy administered to treat Crohn’s disease. The rash worsened during adalimumab therapy and resolved after adalimumab was discontinued. Therefore, it is assumed that adalimumab therapy induced LCH in this patient. While thalidomide, which inhibits TNFα, is used for the treatment of LCH, another TNFα inhibitor paradoxically induced LCH in this patient. Although the skin manifestations of this patient were not psoriasiform rash or palmoplantar pustulosis, which are known to be caused by the paradoxical reaction to TNFα inhibitors, these skin manifestations are noteworthy.
REFERENCES
- Windebank K, Nanduri V. Langerhans cell histiocytosis. Arch Dis Child 2009; 94: 904–908.
- Allen CE, Merad M, McClain KL. Langerhans-cell histiocytosis. N Engl J Med 2018; 379: 856–868.
- Kobayashi M, Tojo A. Langerhans cell histiocytosis in adults: advances in pathophysiology and treatment. Cancer Science 2018; 109: 3707–3713.
- Shahidi-Dadras M, Saeedi M, Shakoei S, Ayatollahi A. Langerhans cell histiocytosis: an uncommon presentation, successfully treated by thalidomide. Indian J Dermatol Venereol Leprol 2011; 77: 587–590.
- McClain KL, Kozinetz CA. A phase II trial using thalidomide for Langerhans cell histiocytosis. Pediatr Blood Cancer 2007; 48: 44–49.
- Seneschal J, Milpied B, Vergier B, Lepreux S, Schaeverbeke T, Taïeb A. Cytokine imbalance with increased production of interferon-alpha in psoriasiform eruptions associated with antitumour necrosis factor-alpha treatments. Br J Dermatol 2009; 161: 1081–1088.
- Rodriguez HN, García I, Alba A, Igea F. Infliximab-induced reactivated Langerhan’s cell hstiocytosis in a patient with ulcerative colitis. Inflamm Bowel Dis 2009; 15: 1286–1287.
- Podjasek JO, Loftus CG, Smyrk TC, Wieland CN. Adult-onset systemic Langerhans cell histiocytosis mimicking inflammatory bowel disease: the value of skin biopsy and review of cases of Langerhans cell histiocytosis with cutaneous involvement seen at the Mayo Clinic. Int J Dermatol 2014; 53: 305–311.
- Therrien A, El Haffaf Z, Wartelle-Bladou C, Côté-Daigneault J, Nguyen BN. Langerhans cell histiocytosis presenting as Crohn’s disease: a case report. Int J Colorectal Dis 2018; 33: 1501–1504.
- Kvedaraite E, Lourda M, Han H, Tesi B, Mitchell J, Ideström M et al. Patients with both Langerhans cell histiocytosis and Crohn’s disease highlight a common role of interleukin-23. Acta Paediatr 2021; 110: 1315–1321.