SHORT COMMUNICATION
Epidermodysplasia Verruciformis in Fitzpatrick Skin Type VI: New Dermoscopic Findings
Rie YOTSU1–3, Chiaki MURASE4, Ryo FUKAURA4, Bamba VAGAMON5,6 and Masaaki KAWASE7
1Tulane School of Public Health and Tropical Medicine, New Orleans, LA, USA, 2Department of Dermatology, National Center for Global Health and Medicine, Tokyo, 3School of Tropical Medicine and Global Health, Nagasaki University, Nagasaki, 4Department of Dermatology, Nagoya University Graduate School of Medicine, Nagoya, Japan, 5Department of Dermatology, Université Alssane Ouattara de Bouaké, Bouaké, Ivory Coast, Côte d’Ivoire, 6Raoul Follereau Institute, Adzopé, Côte d’Ivoire and 7Department of Dermatology, The Jikei University School of Medicine, Katushika Medical Center, Tokyo, Japan. E-mail: ryotsu@tulane.edu
Citation: Acta Derm Venereol 2023; 103: adv10437. DOI: https://doi.org/10.2340/actadv.v103.10437.
Copyright: © Published by Medical Journals Sweden, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: Aug 22, 2023; Published: Sep 27, 2023
INTRODUCTION
Typical epidermodysplasia verruciformis (EV) is a rare genetic cutaneous disorder inherited in an autosomal recessive pattern, characterized by persistent infection with certain types of beta-human papillomavirus (HPV) (1). Clinical features include warty papules and plaques over almost the entire body. Treatment is largely symptomatic, and may include cryotherapy, regular curettage, and surgery. EV is frequently associated with mutations in EVER1/EVER2, genes that are involved in cell-mediated immunity against HPV (2). We report here 2 cases of EV in a pair of siblings from Côte d’Ivoire, in whom dermoscopic features were identified that could be specific to EV and aid diagnosis.
CASE REPORTS
A 20-year-old woman presented with widespread skin lesions. Isolated lesions had appeared in early childhood, and spread extensively during subsequent years. Examination revealed diffuse, polymorphous, hypopigmented, keratotic macules and papules with pseudo-Koebnerization (Fig. 1a–c). Her 19-year-old brother, who was also present, had had similar lesions since childhood, albeit less severe (Fig. 1d, e). The lesions were distributed around the head, torso, axillae, and groin. Their medical histories were otherwise unremarkable. Neither sibling tested positive for HIV. They were initially treated with topical retinoids, before discontinuation due to financial constraints.

Fig. 1. Clinical images of the patients. Photographs of the older sister showing the presence of diffuse, polymorphous, hypopigmented, verrucous macules and papules with pseudo-Koebnerization on her (a) face and chest (b) back and (c) hands. (d, e) Photograph of the younger brother with similar, but less severe, lesions on his (d) forehead and (e) chest. Written consent from the patients is given.
Dermoscopic features of the abdominal lesions from both siblings revealed fairly well-demarcated, asymmetrical, flat whitish spots on dark skin (Fig. 2). Growth of hypopigmented white body hair from and around certain lesions was observed.
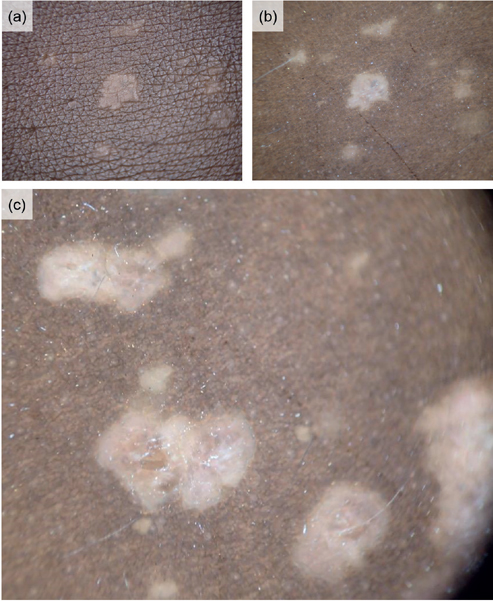
Fig. 2. Higher magnification and dermoscopy images of the lesions. Fairly well-demarcated, asymmetrical, whitish flat spots on dark skin (skin type VI). White body hair occasionally grew from the centre of some lesions and the surrounding skin. (a) Skin surface: (b) dermoscopic image showing a white hair; (c) dermoscopic image of a different area of skin showing multiple white hairs, indicating their reproducibility (magnification x10.)
Skin biopsies were taken, which revealed hyperkeratosis and parakeratosis in the upper epidermis, with enlarged keratinocytes containing abundant blue-grey cytoplasm, enlarged nuclei with pale chromatin, and 1 or more nucleoli (Fig. 3a, c). Immunohistochemistry using anti-HPV monoclonal antibodies (K1H8; Dako Products, Agilent Technologies, Inc., Santa Clara, CA, USA) demonstrated the presence of HPV (Fig. 3b, d). Precipitins, which were brownish gold, were observed in the nuclei of spinous and granular cells. These findings were characteristic of EV.

Fig. 3. Histopathological and immunohistochemical findings associated with epidermodysplasia verruciformis. (a) Older sister haematoxylin-eosin stain ×40; (b) older sister immunohistochemical stain ×40; (c) younger brother haematoxylin-eosin stain ×40; (d) younger brother immunohistochemical stain ×40. (anti-HPV monoclonal antibodies K1H8; Dako Products, Agilent Technologies, Inc., Santa Clara, CA, USA).
It was then attempted to detect genetic predispositions and perform HPV typing; however, as the sample was limited and further samping was difficult to obtain due to the patients living in an extremely rural area, it was opted to perform typing only for HPV-5/-8, which are the types specific to EV. Neither HPV-5/-8 nor typical variants for EV in EVER1/EVER2 in the host gDNA were identified.
Informed consent and ethical approval were gained, and all research was undertaken according to the principles of the Declaration of Helsinki.
DISCUSSION
Typical skin lesions of EV include generalized polymorphic skin lesions, including hypopigmented to hyper-pigmented papules, macules, and plaques. The lesions are asymptomatic, but can cause cosmetic concerns among affected individuals; indeed, the current patients consulted us due to cosmetic concerns. Sun protection was recommended to reduce the risk of developing skin cancer, but, unfortunately, proved difficult, as the patients were farmers with no alternative livelihood. Patients with EV, especially HPV-5/-8, are prone to developing non-melanoma skin cancers, particularly squamous cell carcinomas (3, 4); therefore, they require closer attention and follow-up.
The prevalence of HIV infection among Ivorian adults aged 15–49 years is estimated at 2.4% (5). It was originally suspected that the current patients had acquired EV, a subtype associated with immunosuppressed states but not necessarily inherited (6). However, the patients were HIV-negative. HIV testing is crucial when EV is suspected, particularly in high-prevalence areas and high-risk individuals, in order to rule out a diagnosis of acquired EV.
As EV is such a rare condition, few reports have described its dermoscopic findings in any great detail (Table I) (7–10). Interestingly, the country of origin and patient demographics of these existing reports vary considerably, and have managed to include multiple skin types (7–10). The reports share similar findings, such as a description of an erythematous base (“erythematous”, or “hypopigmented to erythematous”), and dotted vessels (the “red dots” mentioned by Sachdeva et al. (10) presumably refer to dotted vessels). Dotted vessels are classic dermoscopic findings of HPV-related warts, and hence this finding is reasonably expected in EV (11). The finding of white scales is also to be expected, as EV causes hyperkeratosis and eventual shedding of the outer keratin layer (12).
| Country of origin | Patient | Fitzpatrick skin typea | Dermoscopic features | Reference |
| Ecuador | 1. 37-year-old male 2. 15-year-old female |
1. IV 2. II |
1. One lesion with a seborrhoeic keratosis-like appearance (asymmetrical pigmented lesion, comedo-like openings, milia-like cysts, light-brown/erythematous scaly surface) One lesion with a Bowen’s disease-like appearance (keratinized centre, erythematous border, atypical vessels) 2. One lesion with white scales, erythematous base One lesions with a compound melanocytic naevus-like appearance (globular pattern) |
Segura et al., 2006 (7) |
| China | 53-year-old male | III | White scales Erythematous base Dotted/linear irregular vessels |
Wang & Sun, 2019 (8) |
| India | 1. Adolescent male 2. 20s male |
Both V | 1. Unfocused dotted vessels, hypopigmented to erythematous base 2. Hypopigmented to erythematous base (both patients) |
Afra et al., 2019 (9) |
| India | 24-year-old female | V | White scales Red dots Hypopigmented to erythematous base Brown/black areas mixed with hypopigmented areas |
Sachdeva et al., 2022 (10) |
| Cote d’Ivoire | 1. 20s female 2. 20s male |
Both VI | Both patients: Hypopigmented macules, dark base, hypopigmented white vellus hair | Current case |
| aEstimated from clinical photographs. | ||||
Segura et al. (7) reported 2 patients of differing ages and skin types, who were both diagnosed with EV histologically. Interestingly, their dermoscopic features had the greatest variety; certain lesions from the patients were dermoscopically consistent with seborrhoeic keratoses, Bowen’s disease, and melanocytic naevi. The presence of Bowen’s disease in the case of the 37-year-old man serves as a reminder that EV has the potential to undergo malignant change easily, even in relatively young patients. The differing dermoscopic characteristics between the 2 patients reported by Segura et al. (7) could also be explained by the different Fitzpatrick skin types held by each individual.
In comparison, the current cases demonstrate contrasting findings to the previously reported cases. The current patients presented with white lesions on a dark base, as opposed to an erythematous base. One explanation could be that erythematous inflammation is very difficult to observe dermoscopically in Fitzpatrick type VI skin, compared with even Fitzpatrick type V skin, as shown in the 2 papers from India (9, 10). Furthermore, scaling was not a prominent feature in the current cases.
One interesting finding that other cases did not report was the presence of hypopigmented vellus hair growth from the lesional skin, which was not present in healthy areas of the skin, in both patients. Persistent HPV infection has been suggested to interfere with melanogenesis, which would account for this particular finding as well as the hypopigmentation mentioned in the other reports (13).
Dermoscopic findings for patients with EV in Fitzpatrick skin type VI have not been reported previously. We observed that lesions associated with EV in people with Fitzpatrick skin type VI appear white on dark skin (“whites on colour”), as opposed to a hypopigmented/erythematous base as is usually reported. Furthermore, we have identified a potential novel characteristic feature of EV, at least in people of similar skin types, in the growth of hypopigmented vellus hairs from lesional skin. This is significant, as the presence of this feature could help greatly in differentiating EV from other conditions in people of Fitzpatrick type VI skin, who are likely to have atypical features of EV as described above.
REFERENCES
- Bernard H, Burk R, Chen Z, van Doorslaer K, zur Hausen H, de Villiers E. Classification of papillomaviruses (PVs) based on 189 PV types and proposal of taxonomic amendments. Virology 2010; 401: 70–79.
- Ramoz N, Rueda L, Bouadjar B, Montoya L, Orth G, Favre M. Mutations in two adjacent novel genes are associated with epidermodysplasia verruciformis. Nat Genet 2002; 32: 579–581.
- Orth G, Jablonska S, Jarzabek-Chorzelska M, Obalek S, Rzesa G, Favre M, et al. Characteristics of the lesions and risk of malignant conversion associated with the type of human papillomavirus involved in epidermodysplasia verruciformis. Cancer Res 1979; 39: 1074–1082.
- Kawase M. Genetics of epidermodysplasia verruciformis. Current genetics in dermatology (Oiso N, editor). IntechOpen 2013: 121–132.
- UNAIDS. Country factsheets, Côte d’Ivoire, 2021. UNAIDS. [Accessed 2022 Dec 16]. Available from: https://www.unaids.org/en/regionscountries/countries/ctedivoire.
- Moore S, Rady P, Tyring S. Acquired epidermodysplasia verruciformis: clinical presentation and treatment update. Int J Dermatol 2022; 61: 1325–1335.
- Segura S, Carrera C, Ferrando J, Mascaró J Jr, Palou J, Malvehy J et al. Dermoscopy in epidermodysplasia verruciformis. Dermatol Surg 2006; 32: 103–106.
- Wang X, Sun J. Dermoscpic and reflectance confocal microscopic features of epidermodysplasia verruciformis. J Dermatol 2019; 46: e272–e273.
- Afra T, Keshavamurthy V, Razmi M, Khader A, Hafi B. Novel dermoscopic features of pityriasis versicolor-like macules in epidermodysplasia verruciformis. Pediatr Dermatol 2020; 37: 230–232.
- Sachdeva M, Singh J, Sharma S, Dayal S. Congenital epidermodysplasia verruciformis in skin of color: new dermoscopic features. Indian Dermatol Online J 2022; 13: 500–501.
- Dong H, Shu D, Campbell T, Frühauf J, Soyer H, Hofmann-Wellenhof R. Dermatoscopy of genital warts. J Am Acad Dermatol 2011; 64: 859–864.
- Huang S, Wu J, Lewis D, Rady P, Tyring S. A novel approach to the classification of epidermodysplasia verruciformis. Int J Dermatol 2018; 57: 1344–1350.
- Afra T, Vinay K, Razmi T, Khader A, Hafi N. Novel dermoscopic features of pityriasis versicolor-like macules in epidermodysplasia verruciformis. Pediatr Dermatol 2020; 37: 230–232.