Systemic inflammatory response markers, including neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio and monocyte-to-lymphocyte ratio, are useful prognostic factors for various malignant tumours. The aim of this study was to investigate the clinical relevance of these markers in primary cutaneous angiosarcoma. Twenty-six patients were retrospectively divided into 2 groups according to pretreatment peripheral blood cell counts or systemic inflammatory response marker levels; overall survival and progression-free survival were compared. Univariate analysis found that high neutrophil count (> 3.1×109/l), high neutrophil-to-lymphocyte ratio (> 2.4), high platelet-to-lymphocyte ratio (> 175) and low lymphocyte count (≤ 1.3×109/l) were related to shorter overall survival, while high neutrophil and low lymphocyte groups had shorter progression-free survival. In multivariate analysis, high neutrophil count and high neutrophil-to- lymphocyte ratio (hazard ratio 7.44 and 5.04, 95% confidence interval 1.48–37.2 and 1.26–20.1, respectively) were identified as independent prognostic factors for poor overall survival. These results indicate that systemic inflammatory response markers serve as prognostic predictors in primary cutaneous angiosarcoma, as well as in other types of soft-tissue sarcoma.
Key words: cutaneous angiosarcoma; systemic inflammatory response; neutrophil, neutrophil-to-lymphocyte ratio; prognostic factor; overall survival.
Accepted Aug 17, 2021; Epub ahead of print Aug 18, 2021
Acta Derm Venereol 2021; 101: adv00527.
doi: 10.2340/00015555-3898
Corr: Yoshihide Asano and Takuya Miyagawa, Department of Dermatology, University of Tokyo Graduate School of Medicine, 7-3-1 Hongo, Bunkyo-ku, Tokyo, 113-8655, Japan. E-mail: yasano-tky@umin.ac.jp; miyagawat-der@h.u-tokyo.ac.jp
SIGNIFICANCE
Peripheral neutrophil, lymphocyte and platelet counts and their ratios are readily available, and are reported to be useful to predict the prognosis of patients with various malignant tumours. In patients with primary cutaneous angiosarcoma, pretreatment high neutrophil count and high neutrophil-to-lymphocyte ratio are independently associated with shorter lifespan. Since the prognosis of cutaneous angiosarcoma is very poor, and aggressive treatments of patients with low life expectancy can sometimes reduce their quality of life, prognostic prediction may help us choose the best therapeutic options for patients with primary cutaneous angiosarcoma.
INTRODUCTION
Cutaneous angiosarcoma (cAS) is a rare, aggressive soft-tissue sarcoma. The prognosis of cAS is unfavourable due to its high propensity for local recurrence and distant metastasis, with 5-year overall survival (OS) reported to be 33.5% (1). Prognostic prediction of cAS patients, therefore, helps in selection of the best therapeutic options, in which quality of life is considered a more valuable goal than life expectancy. At present, the neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR) and monocyte-to-lymphocyte ratio (MLR) serve as markers of systemic inflammatory response (SIR), and are useful as prognostic factors in many types of cancer (2–5). Owing to their availability in clinical settings, an increasing number of studies on SIR markers has been reported. Several investigations in soft-tissue sarcoma have identified high NLR and PLR as independent factors for poor prognosis (6–9). For angiosarcoma, a few studies have been performed to date. Suzuki et al. (10) reported that high PLR was associated with shorter distant metastasis-free survival in 17 Japanese patients with angiosarcoma of the face and scalp. Wang et al. (11) found that high NLR and high serum lactate dehydrogenase (LDH) were independent factors for poor prognosis for primary angiosarcoma, including visceral subtypes. Thus, among SIR markers, high NLR and PLR seem to be potential predictive factors for poor prognosis in angiosarcoma. On the other hand, it is generally accepted that the subtype of angiosarcoma affects its prognosis (12, 13), suggesting that there is a need for further studies on the clinical significance of SIR markers in patients with cAS. The aim of the current study was to examine the relationship of pretreatment peripheral blood cell counts, NLR, PLR, MLR and biochemical examination values, with prognosis of cAS.
MATERIALS AND METHODS
Study design and population
This study was performed according to the principles of the Declaration of Helsinki and was approved by the ethics committee of the University of Tokyo Graduate School of Medicine (approval number 695). Written informed consent was obtained from all patients. Patients who were histologically diagnosed with primary cAS and underwent treatment at the University of Tokyo Hospital between 1 April 2005 and 31 March 2018, were enrolled and reviewed retrospectively. Their baseline clinical status, pretreatment blood test values, presence of metastasis evaluated radiologically, types of treatment, and date of last follow-up were investigated. NLR, PLR and MLR were calculated as follows: NLR=absolute neutrophil count (×109/l)/absolute lymphocyte count (×109/l); PLR= absolute platelet count (×109/l)/absolute lymphocyte count (×109/l); MLR=absolute monocyte count (×109/l)/absolute lymphocyte count (×109/l).
Statistical analysis
OS was defined as the time interval between the date of diagnosis and death, and, when death could not be confirmed, it was defined as the time until the final confirmation of survival. Progression-free survival (PFS) was defined as the length of time from the start of treatment to disease progression or death. Optimal cut-off values for blood cell counts, NLR, PLR, MLR, and serum chemical biomarkers, such as LDH and alkaline phosphatase (ALP) levels, were calculated by receiver operating curve (ROC) analysis, and all the patients were divided into 2 groups according to cut-off values. The high NLR + MLR group was defined as patients with high NLR and high MLR. High NLR + PLR, and high PLR + MLR groups were also represented. The association of baseline clinical status and pretreatment haematological values with OS or PFS were analysed using Kaplan–Meier methods and compared using log-rank test. Cox-regression multivariate analyses were performed to take into consideration the effect of covariates previously reported to be prognostic factors: age, baseline tumour size, metastatic status, and history of surgical treatment (1, 14). To confirm the fit of the Cox-model, Wald test and likelihood ratio test were also performed. All statistical analyses were performed using JMP® Pro15.0.0 (SAS Institute Inc., Cary, NC, USA) and GraphPad Prism 8.3.1 statistical software package (GraphPad Software, Inc., San Diego, CA, USA). Statistical significance was defined as a p-value < 0.05.
RESULTS
Patient data at baseline
A total of 26 Japanese patients were enrolled in the study. Baseline patient data are summarised in Table I. Median age was 72 years (range 31–96 years), and median OS and PFS were 14.0 months (range 3–72 months) and 8.0 months (range 1–50 months), respectively. Survival curves for all the patients for OS and PFS are shown in Fig. 1. Seventeen patients (65%) were 70 years of age or over, 20 patients (77%) had large tumour size (≥ 5 cm), 19 patients (73%) had metastasis, and 5 patients (19%) had undergone surgical treatment.


Optimal cut-off values for blood test data
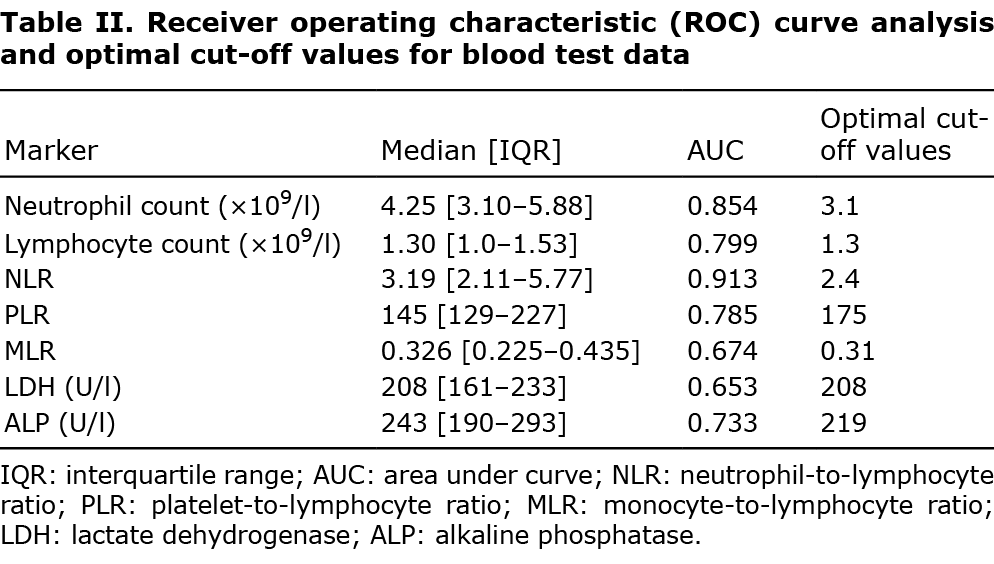
ROC curves for blood test data are shown in Fig. 2. The area under the curve (AUC) and optimal cut-off values were calculated by the ROC curves shown in Table II. All patients were divided into 2 groups according to the cut-off values.

Pretreatment high neutrophil count and neutrophil-to-lymphocyte ratio are associated with shorter overall survival in cutaneous angiosarcoma
In univariate analysis, OS was significantly shorter in the high neutrophil count group (median survival 13.0 vs 50.0 months, p = 0.0035), high NLR group (10.0 vs 50.0 months, p = 0.0025), high PLR group (9.0 vs 16.0 months, p = 0.014), and low lymphocyte count group (10.0 vs 24.0 months, p = 0.014) (Fig. 3). In multivariate analysis, high neutrophil count (hazard ratio (HR) 7.44, 95% confidence interval (95% CI) 1.48– 37.2, p = 0.015) and high NLR (HR 5.04, 95% CI 1.26–20.1, p = 0.022) proved to be independent factors for poor prognosis (Table III). Other markers, such as absolute platelet, monocyte, eosinophil and basophil counts, eosinophil-lymphocyte ratio, and haemoglobin level, were also evaluated; however, none of these were associated with OS (data not shown).


With regard to NLR, PLR and MLR, which have been reported to be associated with prognosis in various types of malignant tumours, including soft-tissue sarcoma, the study evaluated whether the combination of these markers shows more specific association with prognosis. However, as shown in Table III, the combinations of any 2 of high NLR, PLR and MLR were not relevant to poor prognosis.
In some reports, larger tumour size at baseline (≥ 5 cm) are reported to be associated with poor prognosis (1), and therefore the current study examined the relevance of pretreatment tumour size with peripheral neutrophil count and NLR. Although the median peripheral neutrophil count and NLR were elevated in the larger tumour size group, neither peripheral neutrophil count nor NLR at baseline was statistically relevant with regard to their tumour size (p = 0.371 and 0.335, respectively; Student’s t-test).
Pretreatment peripheral blood cell counts and systemic inflammatory response markers are not associated with progression-free survival in cutaneous angiosarcoma
Regarding PFS, the high neutrophil count group (6.0 vs 13.5 months, p = 0.047) and low lymphocyte count group (6.0 vs 10.0 months, p = 0.047) were associated with shorter PFS in univariate analysis. Multivariate analysis revealed that neither of these had significant correlation with PFS. NLR, PLR and MLR were not associated with PFS in univariate analysis (Table III).
Types of treatment were not statistically associated with overall survival, progression-free survival, neutrophil count or neutrophil-to-lymphocyte ratio
These results indicate that pretreatment neutrophil count and NLR are important for predicting the prognosis of patients with cAS. However, types of treatment can affect the survival time. Thus, the correlation between the type of treatment and OS, PFS, pretreatment neutrophil count and NLR were evaluated further. The OS, PFS, neutrophil count and NLR of patients in each treatment group are summarized in Table IV. As for OS and PFS, the combined intensive therapy group, namely the surgery + chemotherapy + radiotherapy group, appeared to have longer survival, although significant correlations were not observed in the log-rank test. In terms of pretreatment neutrophil count and NLR, no significant correlations with type of treatment were observed.

DISCUSSION
The current study revealed that pretreatment high absolute neutrophil count and NLR were independent factors for poor prognosis in primary cAS. This is consistent with the results of a study of angiosarcoma by Wang et al. (11). The report by Suzuki et al. (10), in which baseline peripheral absolute neutrophil count in the angiosarcoma patient group was higher than those in the healthy control group, also supports the current result. Serum LDH and ALP values, previously reported to be prognostic factors in angiosarcoma (11), were not associated with OS or PFS in the current patient population.
In general, inflammatory response is a hallmark of malignant neoplasm and is related to tumour initiation, promotion, and metastatic progression (6). As shown in SIR marker investigations, neutrophils, lymphocytes and platelets are closely associated with systemic inflammatory responses. For instance, neutrophilia can occur in cancer patients due to the hyperproliferation of myeloid cells in response to ectopically overproduced colony-stimulating factors (15–17). In some tumours, decreased populations of tumour-infiltrating lymphocytes (TILs) are linked to worse prognosis (17), and lymphopaenia is reported to be a simple predictive factor for poor OS in advanced sarcoma (18). In breast cancers, cytotoxic CD8+ lymphocytes are dominant in TILs and play an essential role in tumour-killing activity by interacting with tumour antigens and producing cytokines (19). On the other hand, during the process of tumour cell-induced platelet aggregation, activated platelets facilitate tumour survival, angiogenesis, and immunoevasion, thus promoting the metastatic propensity of tumours and related systemic inflammation (20). Although no obvious reason has been elucidated, peripheral blood cell counts, NLR, PLR and MLR can predict the prognosis of patients with malignant tumours.
In terms of TILs, several reports have referred to the association between TILs, peripheral blood cell counts and survival time. Martin et al. (21) reported that pretreatment leukocytosis was associated with a lower intraepithelial CD8+ TIL density and pretreatment leukocytosis predicted poor prognosis, including OS, in patients with anal squamous cell carcinoma. Similarly, Yoon et al. demonstrated a significant inverse correlation between pretreatment TIL levels and peripheral absolute neutrophil count in patients with oestrogen receptor-negative breast cancer and breast cancer showing high Ki-67 expression (22). Furthermore, Fujii et al. (23) showed that patients with cAS with higher numbers of CD8+ TILs in their primary tumours survived significantly longer than patients with lower values. Based on this evidence, we consider that there would be some correlation between pretreatment inflammatory cells infiltrating to the tumours, peripheral blood cell counts and the prognosis. Although the current study examined the association of the number and type of inflammatory cells infiltrating to the tumour with pretreatment blood cell counts in the patients, no statistically significant relevance was observed, possibly because the study group included a relatively small number of patients.
The current results also suggest that neutrophil count or NLR has significant influence on OS of patients with cAS, compared with PFS. Thus it is associated with the choice of first-line treatment strategy, because PFS is more relevant than OS to first-line therapy. Indeed, half of the patients in the current study group were over 75 years of age, and the decision on choice of first-line therapy depended on their co-existing diseases, baseline activity of daily living, cognitive function, and available social support. However, the number of patients in the current study group receiving subsequent lines of therapy was small (27%), and types of treatment were not statistically related to OS, PFS, neutrophil count or NLR, as shown in Table IV. These results may indicate that pretreatment neutrophil count or NLR at baseline could predict the prognosis of patients with cAS irrespective of the therapeutic strategy or response to treatment. Therefore, we assumed that neutrophil count or NLR reflects the intrinsic activity of the tumour cells, which may enable us to explain the difference between the contribution of neutrophil count or NLR to OS and the contribution to PFS.
Regarding some types of carcinomas, meta-analyses have demonstrated that, not only NLR, but PLR and MLR, are prognostic factors (24, 25). However, most investigations of angiosarcoma and other soft-tissue sarcomas conclude that NLR is the only marker for predicting prognosis (6–8, 11). Since the current study showed that absolute neutrophil count was also an independent prognostic factor, we consider that neutrophils are the most important and sensitive blood cells factor in the SIR to cAS. Given that 73% of the current study population had no metastatic disease at baseline, SIR seems to be triggered from the initial stage of cAS. Further studies are needed to clarify the relationship between neutrophils and the prognosis of cAS.
Limitations
This study has some limitations. First, the study was retrospective and includes a relatively small number of patients. Therefore, inherent biases are not fully excluded. Secondly, smoking causes neutrophilia and thus can be a confounding factor in this study, although smoking history was not evaluated because of the lack of data in the medical records. Thirdly, there are some differences between the studies in the cut-off values of NLR, PLR and MLR, and it is difficult to simply compare the current result with those of other studies. Although this is mainly because the cut-off values are determined by the ROC curves made from each study population, another possible reason is that ethnic differences exist in normal values of blood cell counts (26, 27). Therefore, standard cut-off values might be determined taking ethnic differences into account.
Conclusion
Pretreatment high absolute neutrophil counts and NLR were identified as independent factors for poor prognosis for cAS, which is consistent with other types of angiosarcoma and soft-tissue sarcoma investigations. Neutrophils appear to have an important role in the SIR associated with cAS, and further research is warranted to elucidate the relationship between them.
The authors have no conflicts of interest to declare.
REFERENCES
- Shin JY, Roh S-G, Lee N-H, Yang K-M. Predisposing factors for poor prognosis of angiosarcoma of the scalp and face: systematic review and meta-analysis. Head Neck 2017; 39: 380–386.
- Hu B, Yang X-R, Xu Y, Sun Y-F, Sun C, Guo W, et al. Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clin Cancer Res 2014; 20: 6212–6222.
- Geng Y, Shao Y, Zhu D, Zheng X, Zhou Q, Zhou W, et al. Systemic immune-inflammation index predicts prognosis of patients with esophageal squamous cell carcinoma: a propensity score-matched analysis. Sci Rep 2016; 6: 39482–39482.
- Hong X, Cui B, Wang M, Yang Z, Wang L, Xu Q. Systemic immune-inflammation index, based on platelet counts and neutrophil-lymphocyte ratio, is useful for predicting prognosis in small cell lung cancer. Tohoku J Exp Med 2015; 236: 297–304.
- Yang R, Chang Q, Meng X, Gao N, Wang W. Prognostic value of systemic immune-inflammation index in cancer: a meta-analysis. J Cancer 2018; 9: 3295–3302.
- Chan JY, Zhang Z, Chew W, Tan GF, Lim CL, Zhou L, et al. Biological significance and prognostic relevance of peripheral blood neutrophil-to-lymphocyte ratio in soft tissue sarcoma. Sci Rep 2018; 8: 11959.
- Cheng Y, Mo F, Pu L, Li Q, Ma X. Pretreatment inflammatory indexes as prognostic predictors of survival in patients suffering from synovial sarcoma. Front Oncol 2019; 9: 955–955.
- Mirili C, Paydaş S, Guney IB, Ogul A, Gokcay S, Buyuksimsek M, et al. Assessment of potential predictive value of peripheral blood inflammatory indexes in 26 cases with soft tissue sarcoma treated by pazopanib: a retrospective study. Cancer Manag Res 2019; 11: 3445–3453.
- Que Y, Qiu H, Li Y, Chen Y, Xiao W, Zhou Z, et al. Preoperative platelet-lymphocyte ratio is superior to neutrophil-lymphocyte ratio as a prognostic factor for soft-tissue sarcoma. BMC Cancer 2015; 15: 648.
- Suzuki G, Yamazaki H, Aibe N, Masui K, Sasaki N, Shimizu D, et al. Clinical usefulness of the platelet-to lymphocyte ratio in patients with angiosarcoma of the face and scalp. Int J Mol Sci 2017; 18: 2402.
- Wang M, Wu S, Tong A, Cui X, Ma X. The prognostic value of pretreatment inflammatory biomarkers in primary angiosarcoma. Cancer Manag Res 2019; 11: 7981–7989.
- Fayette J, Martin E, Piperno-Neumann S, Le Cesne A, Robert C, Bonvalot S, et al. Angiosarcomas, a heterogeneous group of sarcomas with specific behavior depending on primary site: a retrospective study of 161 cases. Ann Oncol 2007; 18: 2030–2036.
- Young RJ, Brown NJ, Reed MW, Hughes D, Woll PJ. Angiosarcoma. Lancet Oncol 2010; 11: 983–991.
- Lee KC, Chuang S-K, Philipone EM, Peters SM. Characteristics and prognosis of primary head and neck angiosarcomas: a surveillance, epidemiology, and end results program (seer) analysis of 1250 cases. Head Neck Pathol 2019; 13: 378–385.
- McGary CT, Miele ME, Welch DR. Highly metastatic 13762NF rat mammary adenocarcinoma cell clones stimulate bone marrow by secretion of granulocyte-macrophage colony-stimulating factor/interleukin-3 activity. Am J Pathol 1995; 147: 1668–1681.
- Li W, Zhang X, Chen Y, Xie Y, Liu J, Feng Q, et al. G-CSF is a key modulator of MDSC and could be a potential therapeutic target in colitis-associated colorectal cancers. Protein Cell 2016; 7: 130–140.
- Bowen RC, Little NAB, Harmer JR, Ma J, Mirabelli LG, Roller KD, et al. Neutrophil-to-lymphocyte ratio as prognostic indicator in gastrointestinal cancers: a systematic review and meta-analysis. Oncotarget 2017; 8: 32171–32189.
- Ray-Coquard I, Cropet C, Van Glabbeke M, Sebban C, Le Cesne A, Judson I, et al. Lymphopenia as a prognostic factor for overall survival in advanced carcinomas, sarcomas, and lymphomas. Cancer Res 2009; 69: 5383–5391.
- Wang K, Shen T, Siegal GP, Wei S. The CD4/CD8 ratio of tumor-infiltrating lymphocytes at the tumor-host interface has prognostic value in triple-negative breast cancer. Hum Pathol 2017; 69: 110–117.
- Yan M, Jurasz P. The role of platelets in the tumor microenvironment: from solid tumors to leukemia. Biochim Biophys Acta 2016; 1863: 392–400.
- Martin D, Rödel F, Winkelmann R, Balermpas P, Rödel C, Fokas E. Peripheral leukocytosis is inversely correlated with intratumoral CD8+ t-cell infiltration and associated with worse outcome after chemoradiotherapy in anal cancer. Front Immunol 2017; 8: 1225.
- Yoon CI, Park S, Cha YJ, Lee HS, Bae SJ, Cha C, et al. Associations between absolute neutrophil count and lymphocyte-predominant breast cancer. Breast 2020; 50: 141–148.
- Fujii H, Arakawa A, Utsumi D, Sumiyoshi S, Yamamoto Y, Kitoh A, et al. CD8+ tumor-infiltrating lymphocytes at primary sites as a possible prognostic factor of cutaneous angiosarcoma. Int J Cancer 2014; 134: 2393–2402.
- Sun Y, Zhang L. The clinical use of pretreatment NLR, PLR, and LMR in patients with esophageal squamous cell carcinoma: evidence from a meta-analysis. Cancer Manag Res 2018; 10: 6167–6179.
- Wang X, Su S, Guo Y. The clinical use of the platelet to lymphocyte ratio and lymphocyte to monocyte ratio as prognostic factors in renal cell carcinoma: a systematic review and meta-analysis. Oncotarget 2017; 8: 84506–84514.
- Azab B, Camacho-Rivera M, Taioli E. Average values and racial differences of neutrophil lymphocyte ratio among a nationally representative sample of United States subjects. PloS One 2014; 9: e112361–e112361.
- Bain BJ. Ethnic and sex differences in the total and differential white cell count and platelet count. J Clin Pathol 1996; 49: 664–666.