ORIGINAL REPORT
Factors Influencing Major Life-Changing Decisions in Patients with Psoriasis: A Cross-sectional Study
Manuel SÁNCHEZ-DÍAZ1, Pablo DÍAZ-CALVILLO1, Alberto SOTO-MORENO1, Alejandro MOLINA-LEYVA1 and Salvador ARIAS-SANTIAGO1–3
1Dermatology Unit, Instituto de Investigación Biosanitaria IBS Granada, 2Psoriasis Clinic, Hospital Universitario Virgen de las Nieves, and 3Dermatology Department, School of Medicine, University of Granada, Granada, Spain
Psoriasis is a chronic inflammatory disease associated with significant impairment in quality of life. Although quality of life in patients with psoriasis has been widely studied, there is little evidence regarding the impact of psoriasis on major life-changing decisions (MLCD). The aims of this study are to describe the impact of psoriasis on MLCD and to explore the potential clinical factors associated with MLCD. This cross-sectional study included 113 patients with psoriasis, regardless of disease severity, duration, or current treatment. The impact of the disease on different MLCD, including those related to professional career, decision of having children, choice of clothing, and leisure activities, was explored using Likert scales. Mean age was 51 years old and female to male ratio was 1.08 (54/50). The mean Psoriasis Area Severity Index was 3.75, and 30% (35/113) of the patients had psoriatic arthropathy. The most affected MLCD were career choice (median (interquartile range) score 3 (2–4)), social relationships (2 (1–3)), choice of clothing (2 (1–3)), job performance, absenteeism, and choice of holiday destination (1 (0–2)). Female sex, early age of onset and psoriatic arthropathy were associated with a greater impact of the disease on MLCD (p < 0.05). The results showed that a range of MLCD are affected in patients with psoriasis, such as career choice, job performance, absenteeism, or choice of clothing. Female sex, psoriatic arthritis and early age of onset are factors associated with a greater impact on MLCD. In order to limit the long-term negative effects of psoriasis on patients, special attention should be paid to detection of psoriatic arthritis, and to patients with early disease onset.
Key words: psoriasis; quality of life; life-changing decisions.
SIGNIFICANCE
Psoriasis is a chronic skin disease associated with quality-of-life impairment. This study assessed the impact of psoriasis on vital decisions regarding decisive subjects in patients’ lives (termed “major life-changing decisions”). The results show that that psoriasis frequently influences career choice, social relationships, choice of clothing, and job performance. Moreover, female patients, those with an early age of onset of psoriasis and psoriatic arthropathy are more likely to have a greater negative impact of the disease. Special attention should be paid to these groups of patients in order to limit the long-term negative effects of psoriasis.
Citation: Acta Derm Venereol 2023; 103: adv11640. DOI https://doi.org/10.2340/actadv.v103.11640.
Copyright: © Published by Medical Journals Sweden, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: Jun 26, 2023; Published: Oct 10, 2023
Corr: Alejandro Molina Leyva, Dermatology Department, Hospital Universitario Virgen de las Nieves, Avenida de las Fuerzas Armadas 2, ES-18014 Granada, Spain. E-mail: alejandromolinaleyva@gmail.com
Competing interests and funding: The authors have no conflicts of interest to declare.
INTRODUCTION
Psoriasis is a common chronic inflammatory skin and multisystemic disease (1), which may involve joints and could be associated with a variety of comorbidities (2), such as psoriatic arthritis (2), metabolic syndrome and obesity (3), cardiovascular disease (4), and psychological disorders (5, 6). Moreover, psoriasis is related to impairment in the quality of life of both patients and their cohabitants (7, 8).
As previously described by Bhatti et al. (9), chronic disease may have an impact, not only on current quality of life, but also in the long-term on critical life decisions, such as the decision to have children, get divorced, choice of job or place to live. These critical life decisions are therefore named “major life-changing decisions” (MLCD). In Bhatti’s study (9), MLCD are described for both dermatological and non-dermatological disorders.
In this regard, psoriasis, as the standard model of chronic skin disease, may not only have an impact in terms of quality of life, but also by affecting the MLCD of patients throughout their lives.
To date, some published articles refer to the concept of MLCD (10), and also to a proposal of a validated scale to explore MLCD (11), the Major Life Changing Decision Profile, which is translated and validated in Polish (12). However, there are no research studies evaluating how patients with psoriasis are affected in terms of MLCD, nor which clinical and sociodemographic factors are associated with a greater or lesser impact of the disease over the patients’ lifetime in terms of MLCD.
Therefore, the aims of the current study were: to describe the impact of psoriasis on MLCD in a cohort of patients with psoriasis; and to explore the socio-demographic and clinical factors associated with a greater impact on MLCD, so as to identify potential ways of reducing the cumulative negative impact of the disease on patients’ lives.
MATERIALS AND METHODS
Study design
A cross-sectional study was performed including patients with psoriasis regardless of disease severity, disease duration and current treatments. Patients were asked about the impact the disease had had on their life-changing decisions. Socio-demographic, clinical and treatment variables were also collected.
Patients
Patients included in the study were seen at the Dermatology Department (Psoriasis Clinic) of the Virgen de las Nieves University Hospital, Granada, Spain. Patients were asked to participate in a conversation in which they were questioned about the impact of the disease on the decisions made throughout their lives. Patients were recruited between August 2022 and January 2023. Sequential sampling was performed. This study has been approved by the Institutional Review Board of the Virgen de las Nieves University Hospital (Study ID 0671-N-22).
Inclusion criteria
Inclusion criteria were: patients with a clinical diagnosis of psoriasis, regardless of the severity of the disease and the treatment followed; age 18 years or older; and informed consent to be included in the study.
Exclusion criteria
Exclusion criteria were: patient’s refusal to participate in the study; patients or controls who had any other major disease that may have impacted their life decisions.
Ethics
The current study was approved by the Research Ethics Committee of Virgen de las Nieves University Hospital (Study ID 0671-N-22) and is performed in accordance with the principles of the Declaration of Helsinki.
Variables of interest
Main variables. The main variables included those related to the impact of psoriasis on MLCD. These variables were measured by the patient following a 4-point Likert scale (13) which ranged from “0: No impact at all” to “4: Significant impact”. The MLCD considered were some of those originally described by Bhatti et al. (9), and were as follows:
- MLCD related to job: career choice, job performance, job promotion opportunities, absenteeism days, salary, decision to take early retirement.
- MLCD related to education: educational performance, level of education achieved.
- MLCD related to personal relationships: family relationships, social relationships, choice of partner, sexual impairment.
- MLCD related to paternity/maternity: decision to have children, number of children.
- Other MLCD: choice of place to live, choice of house, choice to live abroad, choice of clothing, choice of holiday destination, sport practiced, tobacco consumption, drug consumption.
Other variables. Socio-demographic, biometric and clinical variables, including age, sex, and disease severity measured as Psoriasis Area Severity Index (PASI) (14) and Body Surface Affected (BSA) (15), comorbidities, such as psoriatic arthritis, identified using Classification for Psoriatic Arthritis (CASPAR) criteria (16), current treatments for psoriasis, occupation and educational level were recorded via questionnaires and clinical examination.
Statistical analysis
Descriptive statistics were used to evaluate the characteristics of the sample. The Shapiro–Wilk test was used to assess the normality of the variables. Continuous variables are expressed as mean and standard deviation (SD). Likert scale scores are expressed as median and interquartile range (IQR). Qualitative variables are expressed as relative and absolute frequency distributions. The kappa index was used to explore the concordance between observations. The χ2 test or Fisher’s exact test, as appropriate, were used to compare nominal variables, and the Student’s t-test or Wilcoxon-Mann-Whitney test were used to compare nominal and continuous data. To explore possible associated factors, simple linear regression was used for continuous variables. The β coefficient and SD were used to predict the log odds of the dependent variable. Statistical significance was considered if p-values were less than 0.05. Statistical analyses were performed using JMP version 14.1.0 (SAS Institute, Cary, NC, USA).
RESULTS
Socio-demographic and clinical features of the sample
A total of 134 patients were initially asked to participate in the study. Of these, a final total of 113 (84.2%, 113/134) patients were included. Mean age of the patients was 51.8 years (SD 13.78) and female to male ratio was 1.08 (54:50). Most patients had a long duration of disease (mean disease duration 23.33 years, SD 16.51), were actively working (56.7%, 64/113) and had university or professional studies (55.7%, 63/113).
Regarding clinical variables, the mean BSA was 5.56% (SD 12.7) and the mean PASI was 3.75 (SD 9.78). Most patients (79.64%, 90/113) were on biologic treatment. A third of patients had psoriatic arthropathy (30.9%, 35/113). Detailed information is shown in Table I.
Subjective evaluation of disease severity and impact of the disease on lifetime decisions
Patients and dermatologists were asked to assess the severity of the disease and its impact on life decisions. As shown in Table I, patients perceived a higher severity and scored higher for the impact of the disease on life decisions compared with dermatologists, showing poor concordance (kappa index < 0.20).
Impact of psoriasis on major life-changing decisions
A variety of MLCD were explored (Table II). It was found that the MLCD most affected by psoriatic disease were those associated with career choice (median (IQR) score 3 (2–4)), social relationships (2 (1–3)), and choice of clothing (2 (1.3)). Other affected domains of MLCD were job performance, absenteeism days, choice of holiday destination, sexual activity, and family relationships (1 (0–2) for all of them). The percentage of patients having a moderate or severe impact of disease on most affected MLCD is shown in Fig. 1.
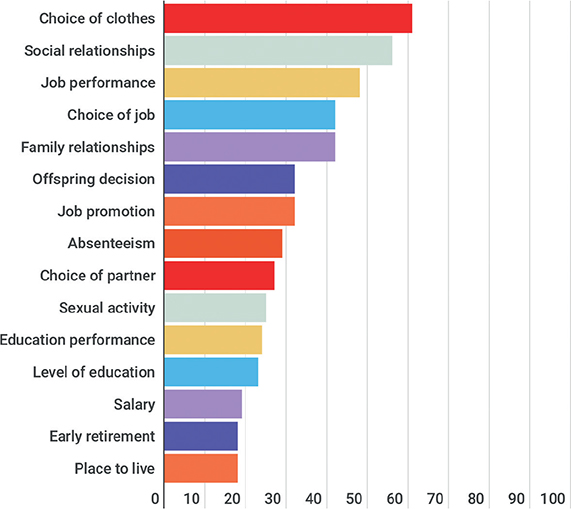
Fig. 1. Percentage of patients showing a moderate or high impact of psoriasis on different major life-changing decisions (MLCD). Only the most affected MLCD are shown.
In contrast, psoriasis had less impact in terms of MLCD on salary, decision to take early retirement, educational performance and level of education achieved, choice of partner (median (IQR) score 0 (0–1)), choice of a place to live and choice of house characteristics (0 (0–0)).
Socio-demographic and clinical factors associated with the most commonly affected major life-changing decisions
Univariate analyses were performed to explore the clinical and socio-demographic factors associated with MLCD in patients with psoriasis. The most affected MLCD were included in the analysis: career choice, job performance, absenteeism days, social relationships, choice of clothing and choice of holiday destination (Table III).
The most important factors associated with MLCD in patients with psoriasis were: female sex, which was associated with a greater impact of psoriasis on MLCD regarding social relationships, choice of clothing and holiday destination (p < 0.005). An early age of onset was associated with a greater impact on MLCD regarding absenteeism, social relationships, choice of clothing and holiday destination (p < 0.05), but showed a trend for all the MLCD explored. Psoriatic arthropathy was related to a greater impact on all MLCD explored except holiday destination. Finally, being unemployed showed similar results to psoriatic arthropathy.
Notably, the subjective impression of the dermatologist about the intrusiveness of the disease throughout the patient’s life was not associated with most MLCD. Moreover, current disease severity measured by PASI and BSA was inconsistently associated with the different MLCD.
Socio-demographic and clinical factors associated with other major life-changing decisions
Univariate analyses were performed to explore the clinical and socio-demographic factors associated with MLCD in patients with psoriasis (Table IV). Salary, choice of a place to live, decision to have children and anxiolytic drugs taken were the MLCD explored.
The most important associated factors were: female sex, which was associated with a greater impact of psoriasis on lifetime salary, choice of place to live, and anxiolytic drugs taken (p < 0.05); younger age, which was associated with a higher impact on MLCD regarding the choice of a place to live and the decision to have children (p < 0.01); psoriatic arthropathy, which was associated with an impact on MLCD regarding salary, decision to have children and anxiolytic drugs taken (p < 0.01); and, finally, being unemployed was associated with all the MLCD explored.
As above, the subjective impression of the dermatologist about the intrusiveness of the disease over the patient’s lifetime was not associated with most MLCD. Moreover, current disease severity measured by PASI and BSA was inconsistently associated with the different MLCD.
DISCUSSION
Psoriasis is a chronic skin disease that seems to have a significant impact on patients’ MLCD. The most affected MLCD are career choice, job performance, absenteeism days and choice of clothing. Moreover, some specific clinical factors seem to be associated with a greater impact of the disease in terms of MLCD.
In this regard, the identification of factors associated with increased MLCD is crucial for limiting the long-term negative effects of psoriasis on patients’ lives. In the current study, among others, 3 specific factors have been found: female sex, joint involvement, and early onset of the disease.
Furthermore, as in quality of life (17), and life-changing decision studies (18), female patients seem to experience a greater impact of the disease in terms of life decisions and are more prone to development of psychological distress. The cause of this association is unclear. On the one hand, sex differences have been found in emotion regulation mechanisms in patients with psoriasis (19). On the other hand, there are probably cultural and social reasons, typical of modern society, the detailed analysis of which is beyond the scope of this study.
Moreover, psoriatic arthropathy appears to play an important role in changing the life decisions of patients with psoriasis. The current study has shown the significant impact of this comorbidity in terms of career choice, job performance, days of absenteeism, social relationships, salary and choice of place to live. Physical limitations caused by joint pain and functional impotence are probably responsible for these findings, and future studies including MLCD specifically related to the physical domain would be of great interest. Despite the lack of specific studies addressing lifetime decisions, quality of life studies also highlight the importance of psoriatic arthritis in terms of quality of life impairment (20). Therefore, it seems that early and effective treatment for joint involvement is crucial to limit the lifetime impact of psoriasis.
Finally, early age of onset of the disease has been linked to a greater burden in terms of absenteeism, social relationships, choice of clothing and holiday destination, as well as choice of place to live. In this regard, previous studies have addressed the importance of the onset of chronic skin diseases during paediatric or adolescent ages (21): chronic skin diseases put paediatric patients at risk of strained family relationships, poor self-image, psychiatric comorbidities, stigmatization, and eventual suicidal behaviour. Therefore, early diagnosis and proper treatment are key to avoiding the dysfunction accumulated throughout the lives of these patients.
Regarding disease severity, the current study showed inconsistent results regarding its relationship with MLCD and mean PASI values were not remarkably high. However, this could be biased, since most patients were currently undergoing advanced psoriasis treatments. Moreover, despite having well-controlled psoriasis at the current time, many patients may have experienced MLCD influenced by their previously very severe psoriasis over many years.
It should be noted that the dermatologist’s subjective assessment does not seem to correlate with the real impact of psoriasis over the patients’ lifetime. Thus, it seems necessary to perform a specific evaluation, asking patients about the impact of the disease over time. These findings are similar to those observed for disease severity and disease symptomatology (22), with patients and dermatologists showing different opinions.
In addition, Bhatti et al. (9), who described the concept of MLCD, have created a questionnaire, the Major Life Changing Decision Profile (MLCDP) (11) based on their initial qualitative study. The MLCDP may be added as a further measure of disease severity or disease impact in future studies on skin disorders, and it would be of great interest to perform this routinely on patients with psoriasis who are visiting the dermatologist, to inform clinical decision making.
The main limitations of the current study are its cross-sectional nature, which makes it impossible to assess causality, the probable overrepresentation of patients with more severe disease, and the limited sample size, which could have led to limited detection of statistical differences.
In conclusion, some MLCD seem to be more significantly affected in patients with psoriasis, such as career choice, job performance, absenteeism days or choice of clothing. The detection of factors associated with greater impact on MLCD, such as female sex, psoriatic arthritis, or early age of onset, is crucial for limiting the long-term negative effects of the disease on patients. The future development of validated tools to assess MLCD in patients with psoriasis, as well as the study of MLCD in patients’ cohabitants, would be of great interest in order to include this measure as a disease characteristic in future studies.
REFERENCES
- Langley RGB, Krueger GG, Griffiths CEM. Psoriasis: epidemiology, clinical features, and quality of life. Ann Rheum Dis 2005; 64: 18–25.
- Oliveira M de FSP de, Rocha B de O, Duarte GV. Psoriasis: classical and emerging comorbidities. An Bras Dermatol 2015; 90: 9–20.
- Jensen P, Skov L. Psoriasis and obesity. Dermatology 2016; 232: 633–639.
- Gao N, Kong M, Li X, Zhu X, Wei D, Ni M, et al. The association between psoriasis and risk of cardiovascular disease: a mendelian randomization analysis. Front Immunol 2022; 13: 918224.
- Aguayo-Carreras P, Ruiz-Carrascosa JC, Molina-Leyva A. Type D personality is associated with poor quality of life, social performance, and psychological impairment in patients with moderate to severe psoriasis: a cross-sectional study of 130 patients. Indian J Dermatol Venereol Leprol 2020; 86: 375–381.
- Lim DS, Bewley A, Oon HH. Psychological profile of patients with psoriasis. Ann Acad Med Singapore 2018; 47: 516–522.
- Randa H, Todberg T, Skov L, Larsen LS, Zachariae R. Health-related quality of life in children and adolescents with psoriasis: a systematic review and meta-analysis. Acta Derm Venereol 2017; 97: 555–563.
- Martínez-García E, Arias-Santiago S, Valenzuela-Salas I, Garrido-Colmenero C, García-Mellado V, Buendía-Eisman A. Quality of life in persons living with psoriasis patients. J Am Acad Dermatol 2014; 71: 302–307.
- Bhatti ZU, Finlay AY, Bolton CE, George L, Halcox JP, Jones SM, et al. Chronic disease influences over 40 major life-changing decisions (MLCDs): a qualitative study in dermatology and general medicine. J Eur Acad Dermatol Venereol 2014; 28: 1344–1355.
- Warren RB, Kleyn CE, Gulliver WP. Cumulative life course impairment in psoriasis: patient perception of disease-related impairment throughout the life course. Br J Dermatol 2011; 164: 1–14.
- Bhatti ZU, Salek SS, Bolton CE, George L, Halcox JP, Jones SM, et al. The development and validation of the major life changing decision profile (MLCDP). Health Qual Life Outcomes 2013; 11: 78.
- Wójcik E, Reszke R, Krajewski PK, Matusiak Ł, Madziarska K, Ali FM, et al. Major life changing decision profile: creation of the Polish language version. Dermatol Ther 2021; 34: e14568.
- Jebb AT, Ng V, Tay L. A review of key likert scale development advances: 1995–2019. Front Psychol 2021; 12: 637547.
- Golbari NM, van der Walt JM, Blauvelt A, Ryan C, van de Kerkhof P, Kimball AB. Psoriasis severity: commonly used clinical thresholds may not adequately convey patient impact. J Eur Acad Dermatol Venereol 2021; 35: 417–421.
- Ogdie A, Shin DB, Love TJ, Gelfand JM. Body surface area affected by psoriasis and the risk for psoriatic arthritis: a prospective population-based cohort study. Rheumatology (Oxford) 2022; 61: 1877–1884.
- Taylor W, Gladman D, Helliwell P, Marchesoni A, Mease P, Mielants H. Classification criteria for psoriatic arthritis: development of new criteria from a large international study. Arthritis Rheum 2006; 54: 2665–2673.
- Mabuchi T, Yamaoka H, Kojima T, Ikoma N, Akasaka E, Ozawa A. Psoriasis affects patient’s quality of life more seriously in female than in male in Japan. Tokai J Exp Clin Med 2012; 37: 84–88.
- von Stülpnagel CC, Augustin M, Düpmann L, da Silva N, Sommer R. Mapping risk factors for cumulative life course impairment in patients with chronic skin diseases – a systematic review. J Eur Acad Dermatol Venereol 2021; 35: 2166–2184.
- Ciuluvica C, Fulcheri M, Amerio P. Expressive suppression and negative affect, pathways of emotional dysregulation in psoriasis patients. Front Psychol 2019; 10: 1907.
- Moraes FA, da Silva MRR, Dos Santos JBR, Acurcio FA, Almeida AM, Kakehasi AM, et al. Health-related quality of life in psoriatic arthritis: findings and implications. Value Heal Reg issues 2021; 26: 135–141.
- Kelly KA, Balogh EA, Kaplan SG, Feldman SR. Skin disease in children: effects on quality of life, stigmatization, bullying, and suicide risk in pediatric acne, atopic dermatitis, and psoriasis patients. Child (Basel) 2021; 8: 1057.
- Griffiths CEM, Augustin M, Naldi L, Romiti R, Guevara-Sangines E, Howe T, et al. Patient-dermatologist agreement in psoriasis severity, symptoms and satisfaction: results from a real-world multinational survey. J Eur Acad Dermatol Venereol 2018; 32: 1523–1529.