QUIZ SECTION
Sporadic Red Papules on the Face: A Quiz
Kexin YAN and Xiulian XU*
Institute of Dermatology, Chinese Academy of Medical Sciences and Peking Union Medical College, Nanjing, China. *E-mail: xxlqjl@sina.com
Citation: Acta Derm Venereol 2023; 103: adv11662. DOI: https://doi.org/10.2340/actadv.v103.11662.
Copyright: © Published by Medical Journals Sweden, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Published: May 22, 2023
A 35-year-old woman presented to our outpatient dermatology clinic with multiple red papules on her face for 1 month. She reported no specific reason for the onset. She had been diagnosed with acne in another clinic and used external medicines for acne, including fusidic acid and retinoic acid cream, without evident effect.
The patient was diagnosed with lupus miliaris disseminatus faciei at another hospital. She was treated with minocycline and compound glycyrrhizin tablets; however, the lesions improved and then recurred. Her lesions were characterized as multiple red papules the size of miliary grains on her face. The papules had a glossy surface, and no pus was observed (Fig. 1A). On physical examination, the patient reported no fever and chills, without lymph node enlargement. No abnormalities were found on routine laboratory examinations or thoracoabdominal computed tomography. According to the physical examination and medical history, the initial suspicion was that the diagnosis might include eruptive xanthoma, lupus miliaris disseminatus faciei, granuloma annulare, and sarcoidosis.

Fig. 1. Cutaneous Rosai-Dorfman disease in the cheek of a 35-year-old woman. (A) Before treatment, her lesions were characterized by multiple red papules the size of miliary grains on her face. The papules had a glossy surface and no pus was observed. (B) After 1 month of treatment, the facial skin of patient has dark-red patches, some papules after fading left pigmentation spots and a little desquamation. Permission from the patient is given to publish these photos.
Reflectance confocal microscopy showed that the epidermis was slightly thin, the basal layer had oedema, inflammatory cells migrated, the basal layer liquefaction had liquefactive degeneration, pigment, and inflammatory cells were infiltrated in the dermis, and tissue-like cells were observed. The skin lesions were biopsied, and pathological examination revealed excessive keratinization of the epidermis with the formation of local keratotic plugs. Diffuse tumour cells were seen in the shallow and deep dermis, with many histopathocytes, lymphocytes, and plasma cells scattered among them. Deep-staining areas of lymphocytes and light-staining areas of cytoplasm-rich histocytes were seen, some of which were foam-like histopathocytes, and phagocytosis was observed (Fig. 2A–B). No caseous necrotic foci were observed. Acid-fast staining was negative. Immunohistochemistry showed that S-100 and CD68 were positive, and CD1a was negative (Fig. 2C–D). The patient was prescribed prednisone acetate 15 mg once a day, methotrexate tablet 5 mg twice a week, and compound glycyrrhizin 50 mg 3 times a day. After 1 month of treatment, the skin lesions improved significantly (Fig. 1B).
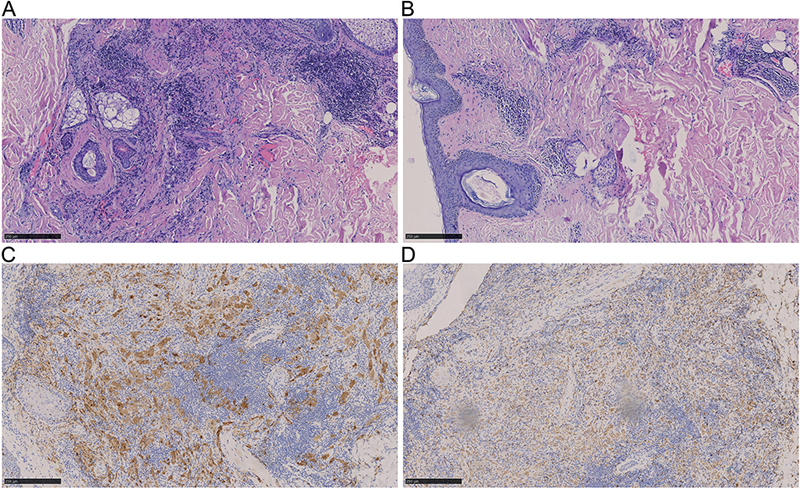
Fig. 2. Histological and immunological stains. (A–B) Epidermal hyperkeratosis with local formation of keratotic plugs, epithelial cell granuloma with lymphocyte and plasma cell infiltration around the appendages of the skin in the middle dermis, interstitial mucous degeneration, erythrocyte extravasation, no caseous necrotic lesions. Deep-staining areas of lymphocytes and light-staining areas of cytoplasm-rich histocytes were seen, some of which were foam-like histopathocytes, and phagocytosis was observed (haematoxylin-eosin staining, magnification× 25 and ×100). (C–D) S100 and CD68 are positive (immunological staining, magnification ×100).
What is your diagnosis? See next page for answer.
ANSWERS TO QUIZ
Sporadic Red Papules on the Face: A Commentary
Diagnosis: Cutaneous Rosai-Dorfman disease
Combined with immunohistochemistry, the cutaneous Rosai-Dorfman disease (cRDD) diagnosis was considered. RDD is a rare non-Langerhans cell histiocytosis known as sinus histiocytosis with massive lymphadenopathy (1). The most affected organs are the skin, subcutaneous tissues, and lymph nodes. The typical clinical symptoms of RDD are painless swollen lymph nodes in the neck associated with fever and night sweats. There are also patients with lesions in the bone, head and neck, kidney, adrenal gland, breast, salivary glands, orbit, nervous system, cardiovascular, respiratory system, bone marrow, liver, and other locations.
The classic histopathological features of RDD are the enlargement and multiplication of histocytes and the infiltration of lymphocytes and plasma cells. Histopathocytes show phagocytosis to lymphocytes and plasma cells and have a characteristic piercing effect. Immunohistochemistry shows that CD163 and S100 express in tissue cells, while CD1a is not expressed (2). cRDD manifests as hyperplasia of skin histocytes. The dermatological symptoms of cRDD are often isolated or fused nodules or patches on the head and neck that are yellowish, purplish, and sometimes tender (3).
Due to its non-specific clinical features, cRDD is often misdiagnosed as acne, eruptive xanthoma, cutaneous tuberculosis, cutaneous lymphoma, or Langerhans cell histiocytosis; therefore, pathology with immunohistochemistry is required (4). Histologically, RDD requires a differential diagnosis from Langerhans cell histiocytosis. RDD is negative for CD1a and shows more pronounced tissue cell puncture than Langerhans cell sarcoma and histiocytosarcoma. Infiltration of IgG4-positive cells can be seen on tissue slides of many patients with RDD, and it is similar to the clinical manifestations of hyper-IgG4 syndrome. The infiltration of IgG4-positive cells needs to be carefully evaluated, as there is more infiltration of IgG4-positive cells in hyper-IgG4 syndrome (5). At present, there are no clear guidelines for management of cRDD. The use of corticosteroids, sirolimus, thalidomide, radiotherapy, chemotherapy, targeted therapy, surgical excision, aminolaevulinic acid (ALA) photodynamic therapy, and other methods have been proposed (6, 7). We identified only 1 previous report of cRDD with clinical symptoms similar to eruptive xanthoma; the opinion was that patients could be observed and followed up because cRDD was a benign disease (8).
We reported a rare clinical manifestation of cRDD that resembled eruptive xanthoma. Misdiagnosis can lead to inappropriate treatment. Therefore, because cRDD can mimic the manifestations of other skin diseases, in addition to careful physical examination, comprehensive laboratory tests, imaging examinations, and pathological and immunohistochemical sections of the skin lesions are necessary. If there are lesions of RDD in other organs except for the skin, the treatment plan should be discussed with physicians from other disciplines. Compound glycyrrhizin is used to treat abnormal liver function, and it has also been used to treat skin diseases because of its anti-inflammatory, anti-allergy, and immune regulatory properties. It has a similar structure and effects to glucocorticoids, but has fewer adverse effects than glucocorticoids (9). The patient had been treated with compound glycyrrhizin after being misdiagnosed with lupus miliaris disseminatus faciei, which was briefly effective. Combined prednisone acetate, methotrexate, and compound glycyrrhizin had a significant therapeutic effect on this patient.
REFERENCES
- Rosai J, Dorfman RF. Sinus histiocytosis with massive lymphadenopathy. A newly recognized benign clinicopathological entity. Arch Pathol 1969; 87: 63–70.
- Goyal G, Ravindran A, Young JR, Shah MV, Bennani NN, Patnaik MM, et al. Clinicopathological features, treatment approaches, and outcomes in Rosai-Dorfman disease. Haematologica 2020; 105: 348–357.
- Fayne R, Rengifo SS, Gonzalez I, et al. Primary cutaneous Rosai-Dorfman disease; a case-based review of a diagnostically and therapeutically challenging rare variant. Ann Diagn Pathol 2020; 45: 151446.
- Gawdzik A, Ziarkiewicz-Wróblewska B, Chlebicka I, Jankowska-Konsur A, Szepietowski JC, Maj J. Cutaneous Rosai-Dorfman disease: a treatment challenge. Dermatol Ther (Heidelb) 2021; 11: 1443–1448.
- Emile JF, Abla O, Fraitag S, et al. Revised classification of histiocytoses and neoplasms of the macrophage-dendritic cell lineages. Blood 2016; 127: 2672–2681.
- Abla O, Jacobsen E, Picarsic J, et al. Consensus recommendations for the diagnosis and clinical management of Rosai-Dorfman-Destombes disease. Blood 2018; 131: 2877–2890.
- Sun L, Shi J, Su Z, Zhang M, Lu Y. Successful treatment of Rosai-Dorfman disease using ALA-PDT. Photodiagnosis Photodyn Ther 2018; 21: 128–129.
- El-Kamel MF, Selim MK, Gawad M. A new presentation of isolated cutaneous Rosai-Dorfman disease: eruptive xanthoma-like lesions. Indian J Dermatol Venereol Leprol 2020; 86: 158–161.
- Cao W, Xiao X, Zhang L, et al. Compound glycyrrhizin combined with antihistamines for chronic urticaria: a protocol for systematic review and meta analysis. Medicine (Baltimore). 2020; 99: e21624.