QUIZ SECTION
Multiple Red-brown Papules and Plaques on the Trunk and Extremities: A Quiz
Xiaoting SONG1–4, Daoning ZHANG1–4, Zuotao ZHAO1–4 and Aiping WANG1–4*
1Department of Dermatology and Venerology, Peking University First Hospital, Xishiku Avenue No. 8, Beijing 100034, China, 2Beijing Key Laboratory of Molecular Diagnosis on Dermatoses, 3National Clinical Research Center for Skin and Immune Diseases and 4NMPA Key Laboratory for Quality Control and Evaluation of Cosmetics, Beijing, China. *E-mail: wangap516@163.com
Citation: Acta Derm Venereol 2023; 103: adv12419. DOI https://doi.org/10.2340/actadv.v103.12419.
Copyright: © Published by Medical Journals Sweden, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Published: Sep 18, 2023
A 55-year-old man presented with a 2-month history of skin lesions on the trunk and extremities, with slight itching. He denied having fever, fatigue, night sweats, or weight loss. He had had hypertension and type 2 diabetes for many years, and denied any history of malignancy or exposure to chemicals. Physical examination revealed erythematous, firm, well-demarcated papules and plaques on his trunk and extremities (Fig. 1a), some of which were dome-shaped fleshy, umbilicated papules (Fig. 1b). A biopsy specimen was taken from his neck for pathological examination. Lesional skin histopathology revealed a dermal infiltrate of foamy histiocytes, Touton-type giant cells with a “wreath-like” arrangement of nuclei, and admixed lymphocytes (Fig. 2). No immunohistochemistry was performed.

Fig. 1. Clinical presentation. (a), Erythematous, firm, well-demarcated papules and plaques on the trunk. (b) Dome-shaped fleshy, umbilicated papules.
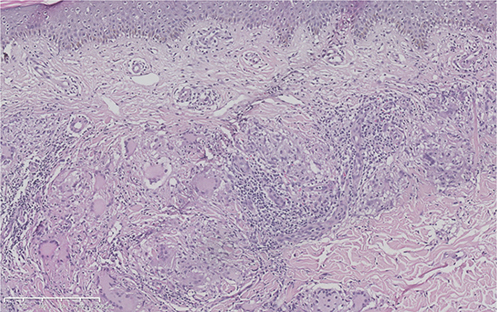
Fig. 2. Histopathological findings. A dermal infiltrate of foamy histiocytes, Touton-type giant cells, and admixed lymphocytes (haematoxylin-eosin, original magnification ×100).
What is your diagnosis?
- Granuloma annulare
- Eruptive xanthoma
- Xanthogranuloma
- Generalized eruptive histiocytoma
See next page for answer.
ANSWERS TO QUIZ
Multiple Red-brown Papules and Plaques on the Trunk and Extremities: A Commentary
Diagnosis: Xanthogranuloma
Xanthogranuloma (XG) is the most common form of non-Langerhans cell histiocytosis, with characteristic Touton-type giant cells in histopathology. In childhood, XG typically resolves spontaneously in most patients with an otherwise unremarkable course. Rare cases may have additional involvement of other systems, including the liver, spleen, central nervous system and eyes, resulting in organ-specific symptoms (1). Although an increased risk of developing juvenile myelomonocytic leukaemia has been proposed in patients with juvenile XG and neurofibromatosis type 1 (NF1), more recent study has not supported this association; hence it remains controversial (2, 3).
In adulthood, the most frequent presentation of XG is a solitary nodule, while in less common conditions it presents with more than 5 lesions and is termed multiple adult XG, and has an association with haematological malignancies. The skin lesions may develop during or after the haematological malignancy (4). As reported previously, the relevant haematological malignancies include myelodysplastic syndrome, B-cell acute lymphoblastic leukaemia, monoclonal gammopathy, follicular lymphoma, essential thrombocytosis, chronic lymphocytic leukaemia, large B-cell lymphoma, and adult T-cell lymphoma/leukaemia (4). The mechanism of the association of haematological malignancy and XG remains unknown. Larson et al. (5) speculated that excess gamma-globulins in these conditions may stimulate histiocytic proliferation and subsequent formation of xanthogranulomas.
Considering the underlying haematological diseases of multiple adult XG, a complete and careful haematological workup was performed in the current patient. Laboratory evaluation showed neutropaenia and anaemia (white blood cell count 1,900/μl, normal range 3,500–9,500/μl; neutrophil 0.5×109/l, normal range (1.8–6.3) ×109/l; red blood cell count 2.19 ×1012/l, normal range (4.3–5.8) ×1012/l; haemoglobin 77 g/l, normal range 130–173 g/l; platelets 188 ×109/l, normal range (125–350) ×109/l). Inflammation-related indicators were elevated, including ferritin levels (724 ng/ml, normal range 23.9–336.2 ng/ml) and C-reactive protein (71.7 mg/l, normal range < 8 mg/l). Biopsies from bone marrow revealed 10% myeloblasts. The patient was diagnosed with myelodysplastic syndrome with excess blasts-2 (MDS-EB2) by haematologists, and scored 6 points on the revised International Prognostic Scoring System and 4 points on the World Health Organization Prognostic Scoring System, suggesting a high-risk disease. He was treated with sindilimab plus decitabine. After the first cycle of chemotherapy, the skin lesions disappeared. After 4 cycles of therapy, biopsy from bone marrow showed 1.5% myeloblasts.
The differential diagnoses of multiple adult XG include generalized granuloma annulare, eruptive xanthoma, generalized eruptive histiocytoma, etc. Generalized granuloma annulare is characterized clinically by widespread annular plaques or umbilicated papules and histologically featured by palisading granulomas. Diabetes and hyperlipidaemia may be risk factors for the development of granuloma annulare (6). Eruptive xanthomas commonly present as small, grouped, red-brown papules on the extensor sides of the trunk and extremities, with the condition of extreme hypertriglyceridaemia. The skin biopsy specimens were characterized by foam cells and extracellular lipid deposition (7). Generalized eruptive histiocytoma (GEH), an extremely rare subtype of non-Langerhans cell histiocytosis, is characterized by recurrent crops of small papules, axially distributed, healing with hyperpigmented macules. The histological findings show a monomorphic histiocytic infiltrate mixed with scarce inflammatory cells (8).
This case alerts clinicians that umbilicated papules may occur in XG, suggesting that XG should be included in the differential diagnosis of umbilicated skin lesions. In addition, multiple adult XG can serve as a cutaneous marker of underlying haematological diseases; hence a complete and careful haematological workup should be recommended when XG is suspected in adult patients.
ACKNOWLEDGEMENTS
We thank the patient for granting permission to publish this information. We also thank Ping Tu, MD, Xixue Chen, MD, and Yang Wang, MD, all from Peking University First Hospital, for their assistance in pathology.
REFERENCES
- Meyer M, Grimes A, Becker E, Browning J, Assanasen C, Libow L, DeNapoli T. Systemic juvenile xanthogranuloma: a case report and brief review. Clin Exp Dermatol 2018; 43: 642–644.
- Raygada M, Arthur DC, Wayne AS, Rennert OM, Toretsky JA, Stratakis CA. Juvenile xanthogranuloma in a child with previously unsuspected neurofibromatosis type 1 and juvenile myelomonocytic leukemia. Pediatr Blood Cancer 2010; 54: 173–175.
- Liy-Wong C, Mohammed J, Carleton A, Pope E, Parkin P, Lara-Corrales I. The relationship between neurofibromatosis type 1, juvenile xanthogranuloma, and malignancy: a retrospective case-control study. J Am Acad Dermatol 2017; 76: 1084–1087.
- Shoo BA, Shinkai K, McCalmont TH, Fox LP. Xanthogranulomas associated with hematologic malignancy in adulthood. J Am Acad Dermatol 2008; 59: 488–493.
- Larson MJ, Bandel C, Eichhorn PJ, Cruz PD, Jr. Concurrent development of eruptive xanthogranulomas and hematologic malignancy: two case reports. J Am Acad Dermatol 2004; 50: 976–978.
- Barbieri JS, Rosenbach M, Rodriguez O, Margolis DJ. Association of granuloma annulare with type 2 diabetes, hyperlipidemia, autoimmune disorders, and hematologic malignant neoplasms. JAMA Dermatol 2021; 157: 817–823.
- Marogi EP, Ohiomoba RO, Stone NJ. Eruptive xanthomas: importance of recognition to reduce delay of effective triglyceride reduction. Am J Med 2022; 135: 444–447.
- Cardoso F, Serafini NB, Reis BD, Nuñez MD, Nery JA, Lupi O. Generalized eruptive histiocytoma: a rare disease in an elderly patient. An Bras Dermatol 2013; 88: 105–108.