QUIZ SECTION
Hyperpigmentation in an Elderly Patient with Atopic Dermatitis: A Quiz
Zhe WU1#, Wenqing ZHANG2,3#, Chenglong WU2,3, Kaili ZHOU2,3 and Zhirong YAO2,3*
1Department of Dermatology, Shanghai Children’s Hospital, School of Medicine, Shanghai Jiao Tong University, 2Department of Dermatology, Xinhua Hospital Affiliated to Shanghai Jiaotong University School of Medicine, and 3Institute of Dermatology, Shanghai Jiao Tong University School of Medicine, Shanghai, China. *E-mail: dermatology.yao@sohu.com
#These authors contributed equally to this work.
Citation: Acta Derm Venereol 2023; 103: 13351. DOI https://doi.org/10.2340/actadv.v103.13351.
Copyright: © Published by Medical Journals Sweden, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Published: Sep 6, 2023
A 73-year-old asian man was admitted to our hospital with severe atopic dermatitis pruritus and body hyperpigmentation during the previous year. He had been diagnosed with atopic dermatitis 6 years previously and had a history of chronic fatigue. Physical examination revealed hyperpigmentation, erythematous scaly plaques, and papules all over his body (Fig. 1), and swollen lymph nodes in the leleft supraclavicular (level VB), right cervical (level IIB), and left occipital (upper level VA).

Fig. 1. Clinical images showing erythematous scaly plaques and papules with generalized hyperpigmentation. Written permission is given by the patient to publish these photos.
What is your diagnosis?
Differential diagnosis 1: Addison’s disease with atopic dermatitis
Differential diagnosis 2: Post-inflammatory hyperpigmentation with atopic dermatitis
Differential diagnosis 3: Mycosis fungoides
Differential diagnosis 4: Kimura’s disease
See next page for answer.
ANSWERS TO QUIZ
Hyperpigmentation in an Elderly Patient with Atopic Dermatitis: A Commentary
Diagnosis: Addison’s disease with atopic dermatitis
Histological examination of the skin lesions revealed epidermal hyperplasia and spongiosis with focal basal liquefaction, and perivascular lymphoid infiltrated with melanocytes, melanophages, eosinophils and plasma cells in the superficial and deep dermis (Fig. 2).
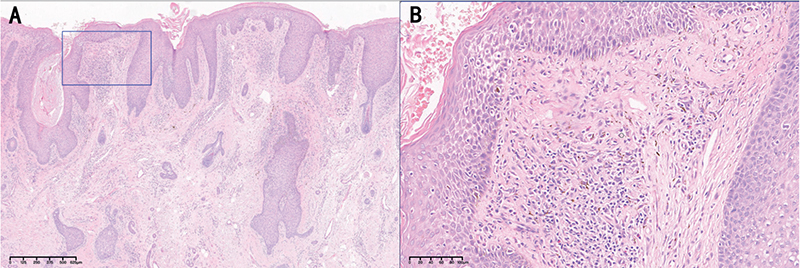
Fig. 2. Epidermal hyperplasia and spongiosis with focal basal liquefaction, and perivascular lymphoid infiltrate with melanocytes, melanophages, eosinophils and plasma cells in superficial and deep dermis. (Haematoxylin and eosin, original magnification: (A) ×40; (B) ×200).
Incisional biopsy of right cervical and left supraclavicular lymph nodes both indicated dermatopathic lymphadenitis without eosinophils.
Biochemical investigations showed an increased eosinophil count (1.55×109/L; reference range 0–0.7×109/L) and markedly elevated serum IgE levels (2,370 IU/mL; reference range 0–100 IU/mL). The computerized tomography abdomen manifestations of adrenal gland were nodular hyperplasia on the left adrenal gland. Comprehensive metabolic panel examinations demonstrated low fasting plasma glucose (FPG) (3.74 mmol/L; reference range 3.9–6.1 mmol/L), low morning serum cortisol level (3.0 μg/dL; reference range 6.2– 19.4 μg/dL) and an elevated level of adrenocorticotropic hormone (ACTH) level (1,232 pg/mL; reference range 7.5–67.2 pg/mL).
A diagnosis of Addison’s disease with atopic dermatitis was made. After treatment with oral glucocorticoid replacement (hydrocortisone 20 mg in the morning, 10 mg in the afternoon) for 2 weeks, the patient’s symptoms subsided rapidly.
Addison’s disease is a relatively rare endocrine disorder, with an estimated prevalence of 93–140 per million in white populations (1). Generalized hyperpigmentation is observed in almost all adult patients with Addison’s disease as well as 67% of paediatric patients, arising from cross-reactivity between the ACTH produced by the corticotrophs and melanocortin 1 receptor on keratinocytes (2, 3). Early identification is crucial, since postponed treatment could result in a potentially fatal adrenal crisis.
In the current case, the elderly patient had had atopic dermatitis for 6 years. The evolution of skin discoloration may be mistaken for post-inflammatory hyperpigmentation (PIH). The differential diagnosis for the erythrodermic appearance and enlarged lymph nodes should also include mycosis fungoides and Kimura’s disease.
Finally, the diagnosis of primary adrenal insufficiency with atopic dermatitis was confirmed by the high level of ACTH and the pathological findings of the skin and lymph nodes.
This is the first case in which a patient had both Addison’s disease and atopic dermatitis skin manifestations (2AD). The term “monism” has been used in diagnostics to illustrate how a single disease can cause 2 or more clinical presentations, which may hamper clinical reasoning. This unusual case indicates that a “dualistic” or “pluralistic” view should be considered in prevalent diseases, especially in the elderly population, in order to prevent missed diagnoses or misdiagnoses.
REFERENCES
- Arlt W, Allolio B. Adrenal insufficiency. Lancet 2003; 361: 1881–1893.
- Lause M, Kamboj A, Fernandez Faith E. Dermatologic manifestations of endocrine disorders. Transl Pediatr 2017; 6: 300–312.
- Michels A, Michels N. Addison disease: early detection and treatment principles. Am Fam Physician 2014; 89: 563–568.