QUIZ SECTION
Ulcerative Tumour on the Frontal Scalp: A Quiz
Myuzu KOIDE, Hiroyuki GOTO, Chika HIRATA, Junko SOWA-OSAKO and Daisuke TSURUTA
Department of Dermatology, Osaka Metropolitan University Graduate School of Medicine, 1-4-3, Asahimachi, Abeno-ku, Osaka 545-8585, Japan. E-mail: 1rmyu3@gmail.com
Citation: Acta Derm Venereol 2023; 103: adv13424. DOI https://doi.org/10.2340/actadv.v103.13424.
Copyright: © Published by Medical Journals Sweden, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Published: Jul 3, 2023
An 84-year-old woman was referred to the department of dermatology with an ulcerative tumour on her left frontal scalp. She had detected a nodule there 7 months previously, which had gradually enlarged with ulceration. Physical examination revealed a red ulcerative tumour on the left frontal scalp, 50×30 mm in size (Fig. 1a. Several indurative lesions of 10–25 mm were present around the tumour. Positron emission tomography–computed tomography (PET-CT) revealed accumulation of fluorodeoxyglucose in the lesion (Fig. 1b). Haematoxylin-eosin staining of the histopathological specimen revealed massive proliferation of sheet-like tumour nests composed of atypical epithelioid cells from the superficial dermis to the subcutis (Fig. 1c, d).
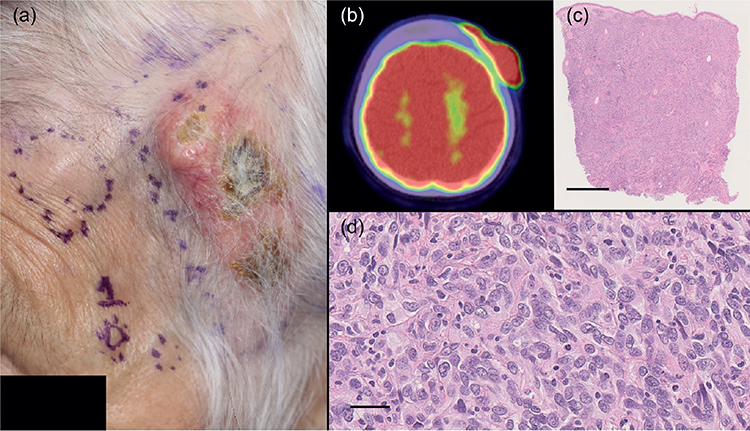
Fig. 1. Initial findings. (a) Physical examination revealed a red ulcerative tumour on the left frontal scalp, 50×30 mm in size, and several indurative lesions around the tumour (purple circles). (b) Positron emission tomography–computed tomography (PET-CT) showed accumulation of fluorodeoxyglucose in the lesion. (c) Histopathological examination revealed massive proliferation of sheet-like tumour nests from the superficial dermis to the subcutis (haematoxylin-eosin staining, bar = 1 mm). (d) Tumour nests were composed of atypical epithelioid cells (haematoxylin-eosin staining, bar = 20 μm). Informed consent was obtained from the patient.
What is your diagnosis? See next page for answer.
ANSWERS TO QUIZ
Ulcerative Tumour on the Frontal Scalp: A Commentary
Diagnosis: Epithelioid angiosarcoma
Based on the clinical findings of an ulcerative tumour on the head and neck region in an elderly patient and proliferation of atypical epithelioid cells, the initial tentative diagnosis was squamous cell carcinoma. However, the tumour nests were not continued into the epidermis. Immunohistochemistry revealed tumour cells that were strongly positive for vimentin, focally positive for epithelial membrane antigen, and negative for AE1/3, CK5/6, CK7, and p40 (Fig. 2a, b). Although poorly differentiated squamous cell carcinoma is sometimes negative for keratin staining and positive for vimentin, other diagnoses were considered, including malignant melanoma, lymphoma, and angiosarcoma (1). Additional immunohistochemistry was negative for carcinoembryonic antigen, CD3, CD34, CD56, CD79a, melan A, and S-100 protein, and positive for CD31 and D2-40 (Fig. 2c). Based on the results of haematoxylin-eosin staining and immunohistochemistry, a definitive diagnosis of epithelioid angiosarcoma was made, and the patient commenced radiotherapy and chemotherapy.
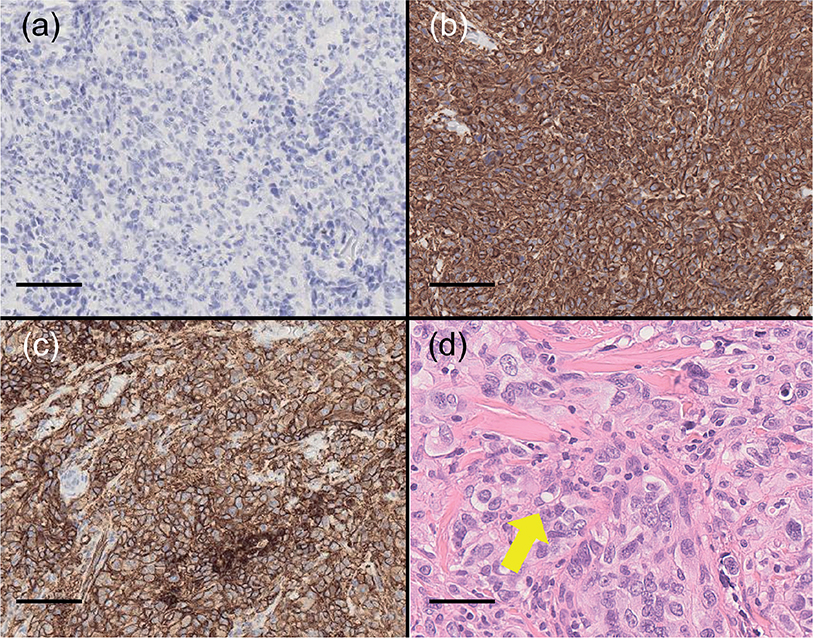
Fig. 2. Further histopathological findings. Immunohistochemistry revealed that tumour cells were (a) negative for AE1/3 (bar = 100 μm), (b) positive for vimentin (bar=100 μm), and (c) positive for CD31 (bar = 100 μm). (d) Intracytoplasmic vacuoles without erythrocytes (yellow arrow) were observed in some regions (bar = 20 μm).
Epithelioid angiosarcoma is a rare variant of angiosarcoma. Histopathological characteristics include sheet-like proliferation of large oval-to-round epithelioid cells with abundant eosinophilic cytoplasm, severe atypia, extravasation of erythrocytes, vascular differentiation, and intracytoplasmic vacuoles containing erythrocytes (2). In the current case, however, histopathological extravasation of erythrocytes was not present and, clinically, there was no purpura around the tumour. Several intracytoplasmic vacuole-like structures were present, but no erythrocytes were detected in the vacuoles (Fig. 2d). In such a case, diagnosis of epithelioid angiosarcoma is challenging. When proliferation of atypical epithelioid tumour cells that are negative for keratin expression is observed, the possibility of epithelioid angiosarcoma should be included in the differential diagnosis.