Suicide in young children is rare; the incidence increases towards the end of adolescence. Skin disorders confer a high prevalence of psychiatric and psychological comorbidities. However, published research on suicidal behaviour in adolescents and children with skin disorders is sparse. The aim of this study was to identify the prevalence of suicidal behaviour in children and adolescents under 18 years of age with chronic skin disorders and associated contributing risk factors. MEDLINE, PsycINFO, EMBASE, CINAHL and Cochrane databases were searched from inception to October 2020 for suicide or suicide attempts in patients under 18 years old with chronic skin disorders. The study protocol was logged on PROSPERO (CRD42020083528). Returned texts were reviewed independently by 2 authors. Bias was assessed according to Joanna Briggs Institute criteria. Five studies met the inclusion criteria; 4 cross-sectional surveys and 1 retrospective matched-cohort study. A total of 31,641 patients with acne, atopic dermatitis, body dysmorphic disorder or psoriasis were identified. Prevalence of suicidal ideation was 0.45% (psoriasis) to 67% (body dysmorphic disorder). The prevalence of suicidal attempts ranged from 0.08% (psoriasis) to 21.9% (acne). Patients with acne or atopic dermatitis had significantly increased odds ratio for suicidal attempts. Meta-analysis could not be performed owing to the heterogeneity and sparsity of data. Suicidal risk in skin disorders amongst adolescents and children under the age of 18 years old is broad and complex. The suicidal risk remained after adjusting for depression, suggestive of an alternative mechanism.
Key words: adolescence; chronic skin disease; childhood; paediatric; suicide; systematic review.
Accepted Aug 11, 2022; Epub ahead of print Aug 11, 2022
Acta Derm Venereol 2023; 103: adv00851.
DOI: 10.2340/actadv.v102.1502
Corr: Richard Barlow, University Hospital Coventry and Warwickshire, Clifford Bridge Rd, Coventry, CV2 2DX, UK. E-mail: Richard.barlow2@nhs.net
SIGNIFICANCE
This study examined suicidal behaviour among children and adolescents with chronic skin disorders. The results show that the rate of suicide attempts varies greatly between children and adolescents with acne, eczema, body dysmorphic disorder or psoriasis. Suicidal attempts reported were in the range 0.08% (in psoriasis patients) to 21.9% (in patients with acne). The overall risk for suicidal behaviour in children and adolescents with skin disorders is therefore high. Dermatologists need to be aware of what to look for in this population. The overall risk is more complex to interpret than originally thought and is multifactorial.
INTRODUCTION
Suicide in younger children is rare and is often misreported as accidental or unintentional death (1). It is, however, one of the main causes of death in young adults in many countries worldwide, and these deaths are particularly devastating for the families involved. Five cases of suicide in children under 13-years-old were reported during 2014 to 2016 in England, out of a total of 922 deaths by suicide in under 25-year-olds (2). Comorbid dermatological and respiratory disorders were among the most prevalent co-factors (9%). More recently, it has been speculated that COVID-19 has disproportionately impacted on children and adolescents than in years prior compared with other age groups. There were 25 cases of suicide in children recorded in the first 56 days of COVID-19 lockdown in England 2020 (April–May); with weak evidence to suggest the rate was higher than the corresponding pre-pandemic period in 2019 (p = 0.14). Restricted access to education, recreational activities, disruption to care and support services, tensions at home and isolation were postulated to contribute (3). Whilst this data represents England only, it may well represent other countries similarly affected by the COVID-19 pandemic.
There is a high level of suicide rates as people approach late adolescence and early adulthood (4). The World Health Organization reported suicide as the third leading cause of death in 15–19-year-olds in 2016 worldwide (5). Suicide was in the top 5 causes of death for 10–14-year-olds in 18 countries in 2016 (6). Furthermore, suicide deaths represent the tip of the iceberg of suicidal behaviour and mental distress. It is estimated that for every suicide death in a 12–17-year-old, there are approximately 100 times (in males) and 1,000 times (in females) more hospital attendances for self-harm (7). The numbers presenting to community mental healthcare services are approximately 10 times higher (7).
There is an established link between chronic skin disorders and the mental and psychological health of an individual (8). This ranges from lowered self-confidence to anxiety, depression and suicide; indeed, it is reported that over a third of dermatological patients have comorbid psychiatric and psychological conditions (9). Several studies have examined this relationship in adults with chronic skin disorders. Other work has highlighted risk factors for suicide in the general population, including comorbid depression, deliberate self-harm and previous suicide attempts (10). The prevalence of suicide and associated risk factors in children and adolescents with skin disorders are less well documented.
Childhood and adolescence represents an important stage in the development of a person’s self-identity. Experiences during this time inform the individual’s adulthood and interpretation of the world. The integumentary system is intimately concerned with many people’s sense of self, and it is crucial, therefore, that the burden of suicide and its associated risk factors are explored in the context of skin disorders.
This study aimed to systematically review the current evidence examining the prevalence of attempted or completed suicides, and the risk factors contributing to this behaviour, in children and adolescents (under 18 years of age) with chronic skin disease. The intended outcomes of the study were to help assess the prevalence of this phenomenon, the contributing risk factors, and to better equip healthcare professionals in the management of patients.
MATERIALS AND METHODS
Protocol, registration and search strategy
The study protocol was logged in the University of Nottingham, UK, PROSPERO database (ID number CRD42020083528) prior to data synthesis. An electronic literature search, using 823 terms, was conducted across 5 electronic databases (MEDLINE, PsycINFO, EMBASE, Cochrane database and CINAHL) up to October 2020 with no lower date limit. A full list of search terms is available online in Appendix S1. The final list of papers generated was then compiled, together with additions recommended from experts in the field.
Inclusion criteria
- Peer-reviewed, observational studies (cohort, case-control and cross-sectional) with a patient group under 18 years old with chronic skin disease.
- Outcome defined as suicide and non-fatal suicide attempts.
- English language publications with no restrictions imposed on location.
Exclusion criteria
- Qualitative studies, case reports, comments, abstracts and editorials.
- Outcome other than suicide or non-fatal suicide attempts.
Study selection
Literature search results were screened by 2 reviewers (PM and SH) to identify all citations that met the inclusion criteria, followed by more detailed examination by 2 other reviewers (RB and GP). Discrepancies in selection were reviewed by a third reviewer (AB) for arbitration.
Risk of bias in individual studies
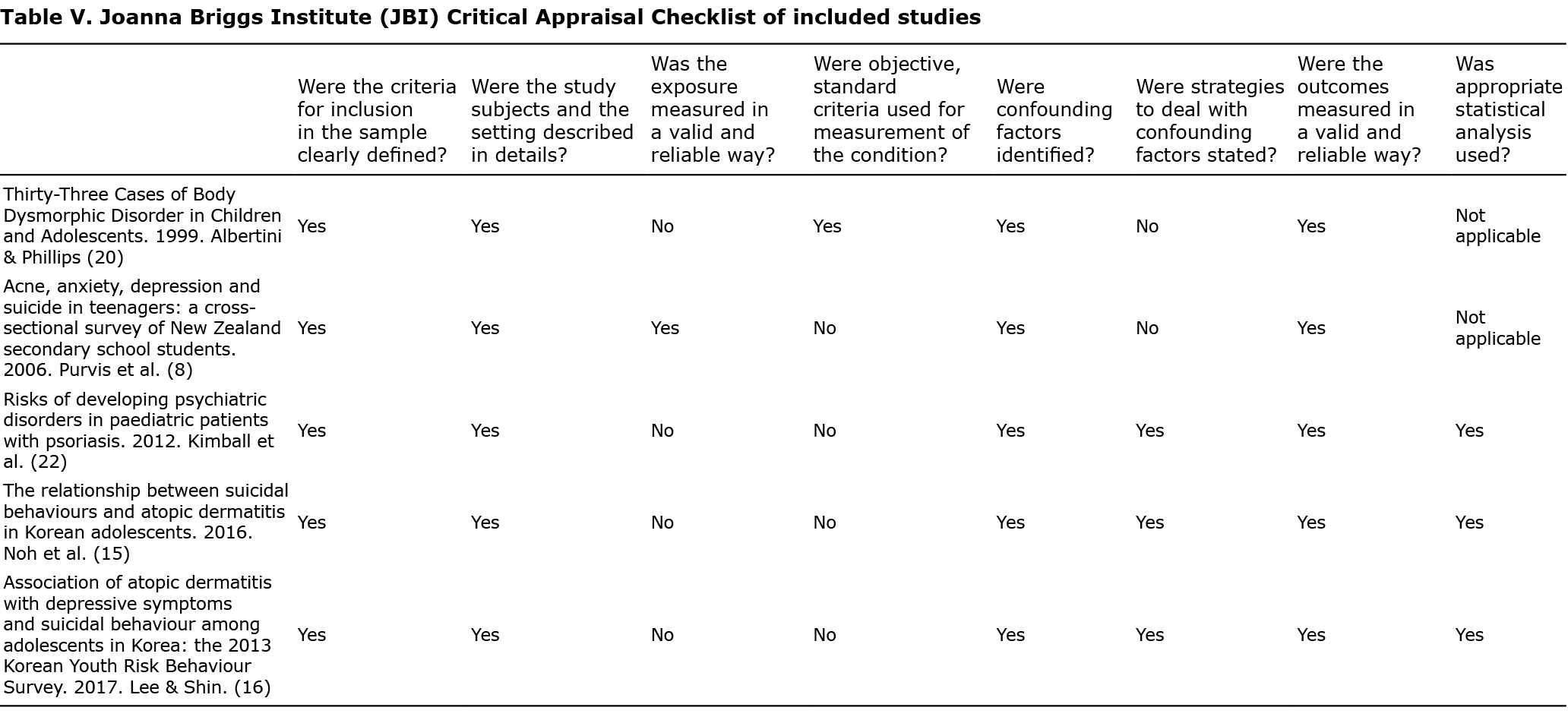
Included studies were assessed for risk of bias by RB and PM, using the Joanna Briggs Institute (JBI) Critical Appraisal Checklist (11).
Summary measures and synthesis of results
Characteristics of the included studies were described, and the results discussed in a narrative synthesis. Meta-analysis for each skin condition was planned if sufficient homogenous studies were identified.
RESULTS
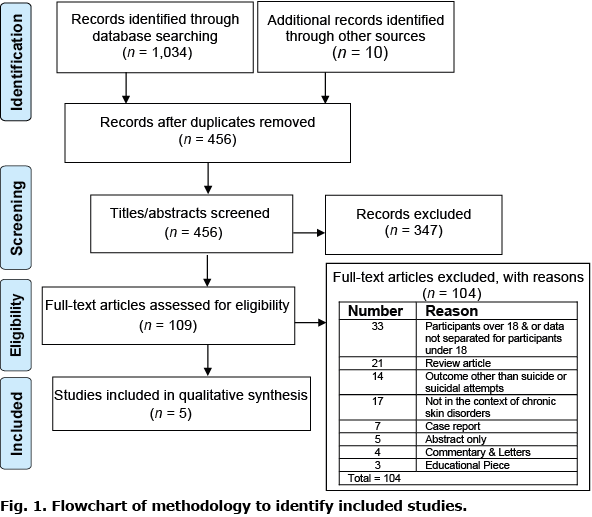
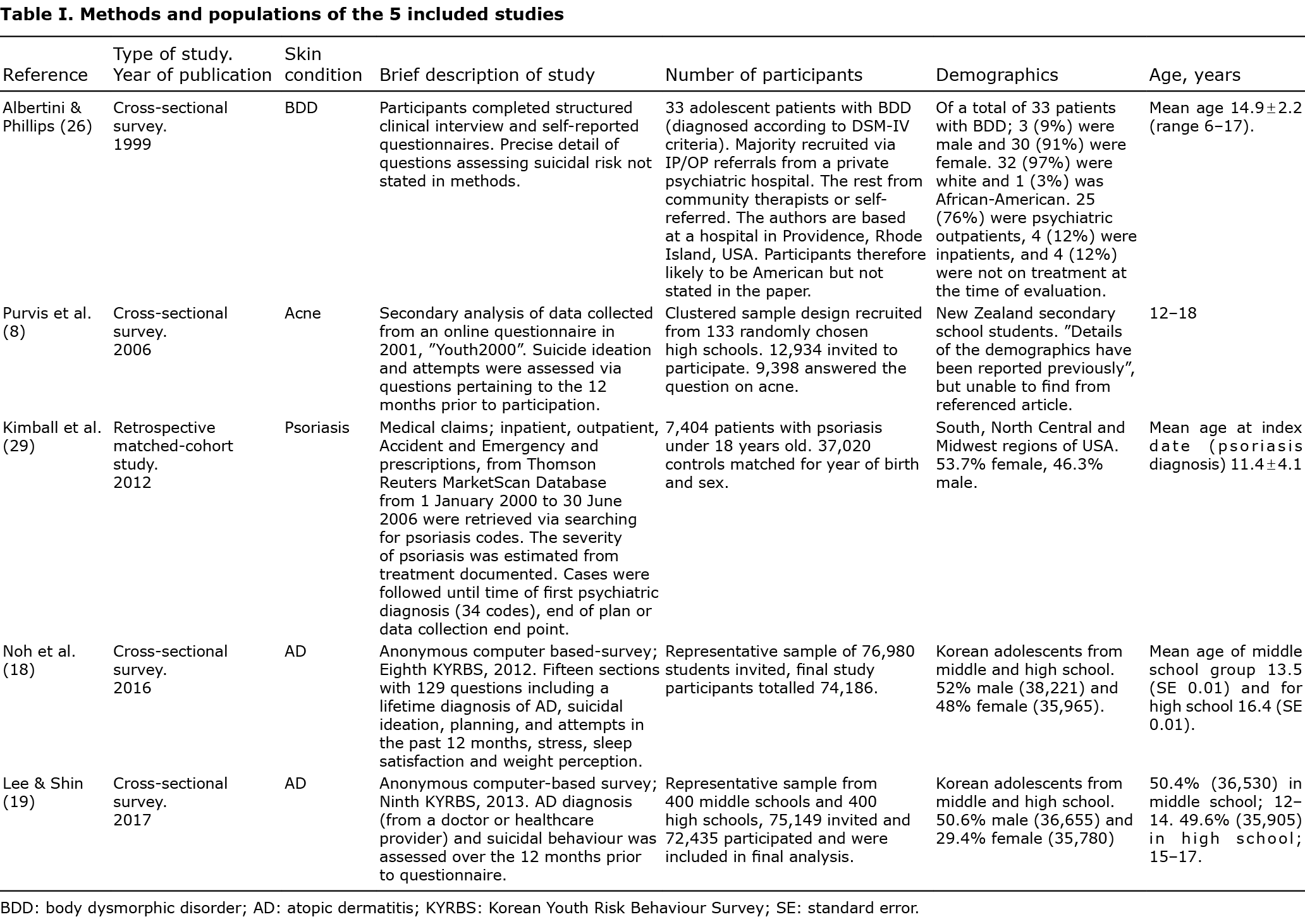
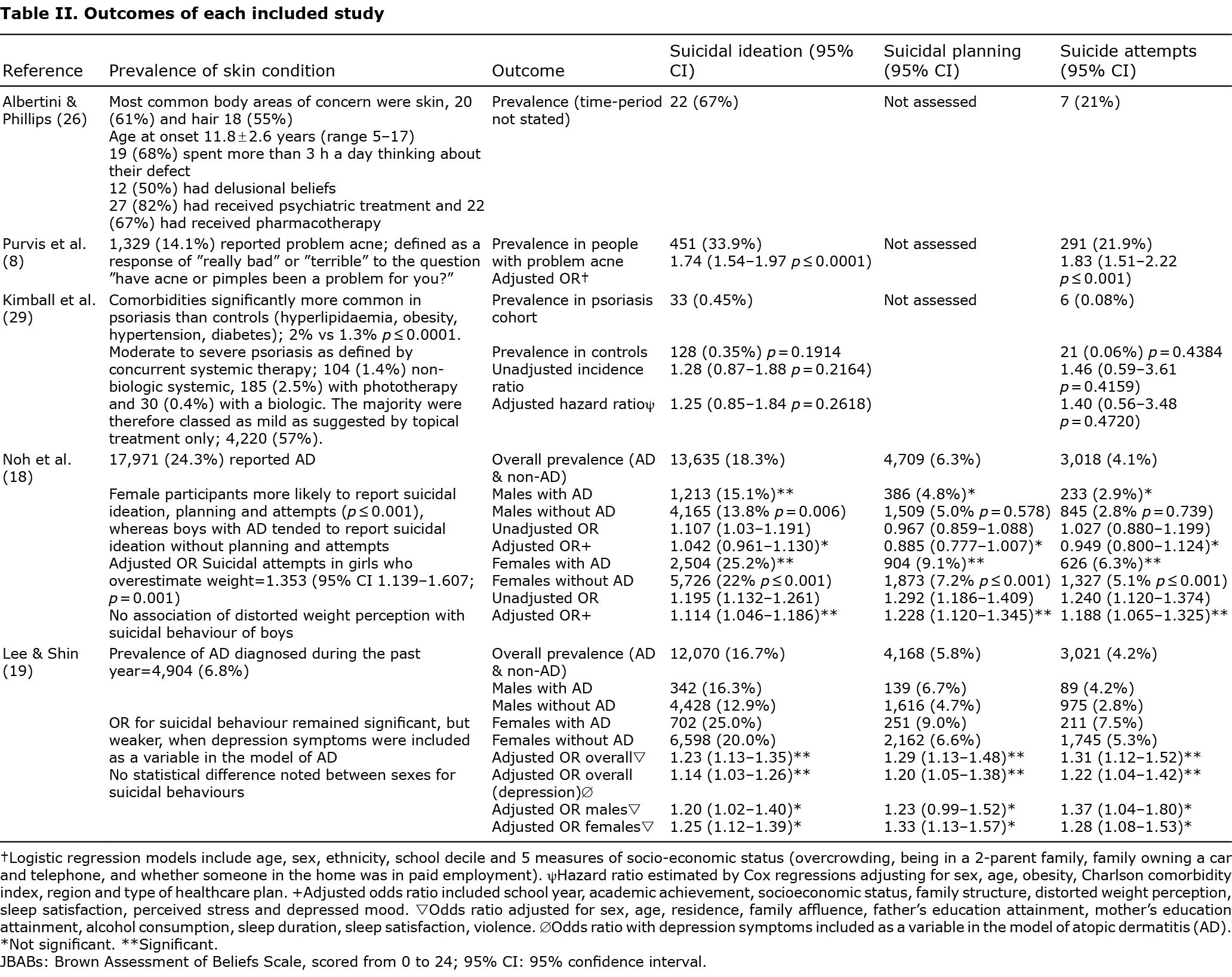
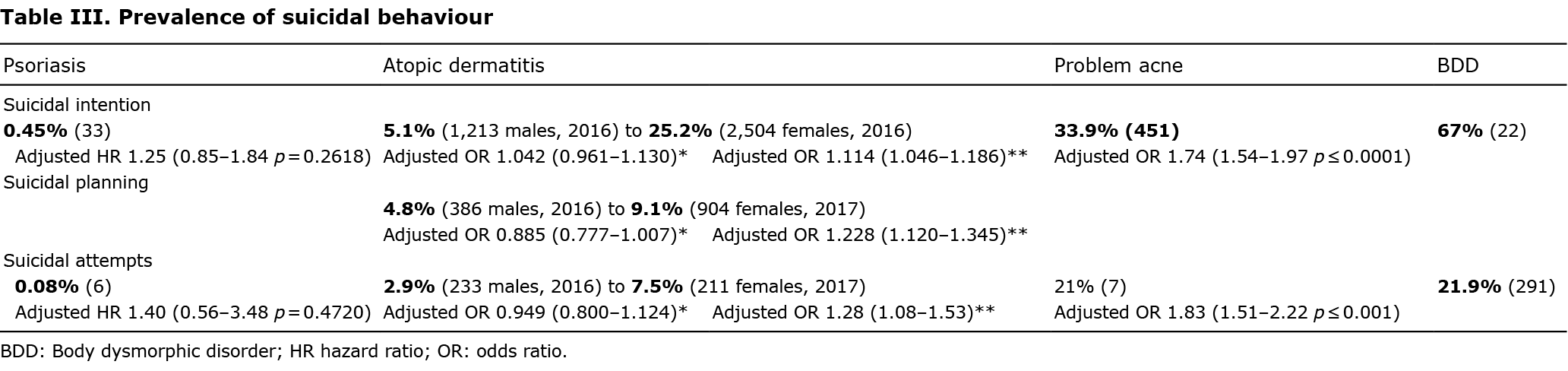
Five studies met the inclusion criteria (Fig. 1). Methods and populations of the included studies are outlined in Table I and the outcomes are shown in Table II. Table III shows a summary of the prevalence of suicidal behaviour for each skin condition. All reported data is from the original papers.
DISCUSSION
Acne
Purvis et al. (12) demonstrated high levels of suicidal behaviour in adolescent New Zealanders with acne. Self-assessment of severity suggests this may be more accurate than objective measures when correlating with suicidal behaviour. Importantly, the finding for suicidal attempts remained significant after controlling for co-existent depressive symptoms and anxiety; odds ratio (OR) 1.5 (95% confidence interval (95% CI) 1.21–1.86).
It is important to note, however, that suicidal behaviour is comparatively high in adolescents; lifetime rates of suicidal ideation and attempts have been reported at 22.5% and 5.2%, respectively, at 18 years old (10). Therefore, the reportedly high incidence of suicidal attempts in patients with severe acne may be representative of the combined baseline risk in this age and the higher prevalence of acne towards late adolescence.
In addition, this study did not comment on acne treatments received. Isotretinoin has been linked with suicidal behaviour, including suicide attempts, in patients with acne. It is highly effective in treating severe and nodulo-cystic acne since its introduction in the 1980s. Case reports and case series to date suggest that it has caused depression and suicide deaths in some individuals (13,14). These findings have not been reproduced in larger cohorts including one paper in the year 2000 of 7,535 patients with acne treated with isotretinoin across Canada and the UK (15), and a study in the Czech Republic of 100 patients with acne treated with isotretinoin in 2008 (16). More recently, a cohort and nested case-time-control study of 443,814 patients with acne exposed to isotretinoin in France, in 2019, demonstrated a lower incidence of suicide compared with controls (17). Overall, these studies found no evidence that use of isotretinoin is associated with an increased risk of depression, suicide, or other psychiatric disorders. Isotretinoin was, in fact, shown to improve rates of depression in many cases thought to be secondary to improvement of acne.
The prevalence of acne is greater in adolescents and young adults therefore identifying suicidal behaviour rates in adults alone is challenging. A cross-sectional study conducted in 2000 by Gupta et al. (18) reported prevalence of suicidal ideation in people with self-reported mild-to-moderate acne, mean age 23 (± 6.8 years) of 5.6%. Other studies report up to 7.1% prevalence for suicidal ideation in adults (19). Interestingly, a Finnish study of male military conscripts aged 18–25 years old with acne, demonstrated no significant increase in comorbid psychopathology including suicidal ideation compared to controls (20). It may well be that suicidal behaviour in children and adolescents with acne therefore is higher than the rates in adults.
Atopic dermatitis
Two of the included studies examined suicidal behaviour in atopic dermatitis (AD) from the 8th and 9th Korean Youth Risk Behaviour Survey (KYRBS) (21, 22), an annual survey in Korea that aims to identify suicidal risk factors in adolescents. Korea has higher rates of suicide in adolescents compared with the rest of the world.
AD was shown to have a profound effect on suicidal behaviour, particularly in females who were prone to overestimate their weight. The psychosocial burden of the patient is also shouldered by close family members. A study from Japan extended this further and demonstrated prevalence of homicide–suicidal ideation as high as 3.28% in parents and family (23).
Other research has shown that children with eczema are at a significantly higher risk of psychotic experiences by age 13 years; OR 1.33 (95% CI 1.04–1.69) adjusted for sex, social class and ethnicity in a UK cohort (24). There is already an established link between psychosis and suicidal risk, although it remains unclear how AD contributes. A Finnish study examining atopic disorders in twins showed a small shared genetic risk for atopic and depressive symptoms disorders (25).
There is a substantial body of literature examining suicidal behaviour in adults with AD and a broad range, similar to the paediatric population is noted. Suicidal ideation has been reported at 2.1% to 21.5%, suicide attempt at 0.86–2.03% (26, 27). It may well be therefore that the rate of suicidal attempt is indeed higher in the paediatric population. Certainly, the risk is high in both age groups regardless, as reported by a recent systematic review; suicidal ideation was 44% more likely in patients with AD (pooled odds ratio, 1.44; 95% CI, 1.25-1.65) and suicide attempt was 36% more likely (pooled odds ratio, 1.36; 95% CI, 1.09-1.70) compared to controls (28).
Body dysmorphic disorder (diagnosed by Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) criteria)
Albertini & Phillips (29) reported high levels of suicidal behaviour, particularly striking given the age range of 5–17 years. The study did not define the time-frame examined in the questionnaire; however, similar findings have been reported in BDD with a prevalence of suicide attempts at 13.9% for under 20-year-olds (30).
The study population location was not documented, although the authors were based in Rhode Island, USA. Comorbid psychopathology was present in the majority of cases.
A recent meta-analysis of adults with BDD demonstrated a lifetime suicide attempt rate of 35.2%, which dropped to 18.9% when controlled for substance abuse (31). The study was limited by heterogeneity of the included studies and did not include completed suicide rates in quantitative analyses. Therefore, it could be argued that the risk of suicide and related behaviour is particularly high in adolescents and children.
Psoriasis
Kimball et al. (30) showed that children and adolescents with psoriasis were more likely to develop psychiatric disorders (adjusted HR 1.25, 95% CI 1.11–1.40; p = 0.0001); depression, anxiety and bipolar disorder were the most common (32). Patients with psoriasis were also more likely to be on psychiatric medication (adjusted HR 1.47 95% CI 1.34–1.61; p ≤ 0.0001).
Suicidal ideation has been estimated at 6–12.7% for adult patients with psoriasis of varying severity (26). A Danish group identified that the risk of self-harm and suicide attempts was found to be increased only in adults under 30 years old compared to controls (incidence rate ratio = 1.81, 95% CI 1.02-3.20, p = 0.043) (33). Despite data in adult populations suggesting a higher burden of suicidal behaviour compared with children in the context of psoriasis it is important to note that data from Kimball et al. is likely to represent the lower bound of risk given the majority of the psoriasis patients were using topical treatments only.
Other skin conditions
Alopecia. Suicidal behaviour in alopecia is probably under-acknowledged; 4 cases of suicide in male adolescents with alopecia areata were reported in Australia in 2011. None had previous psychiatric disorders prior to diagnosis. Common themes following diagnosis included social withdrawal and school avoidance. All were under the care of a psychologist or psychiatrist at the time of death (34). Treatment modalities were not reported.
Additional risk factors
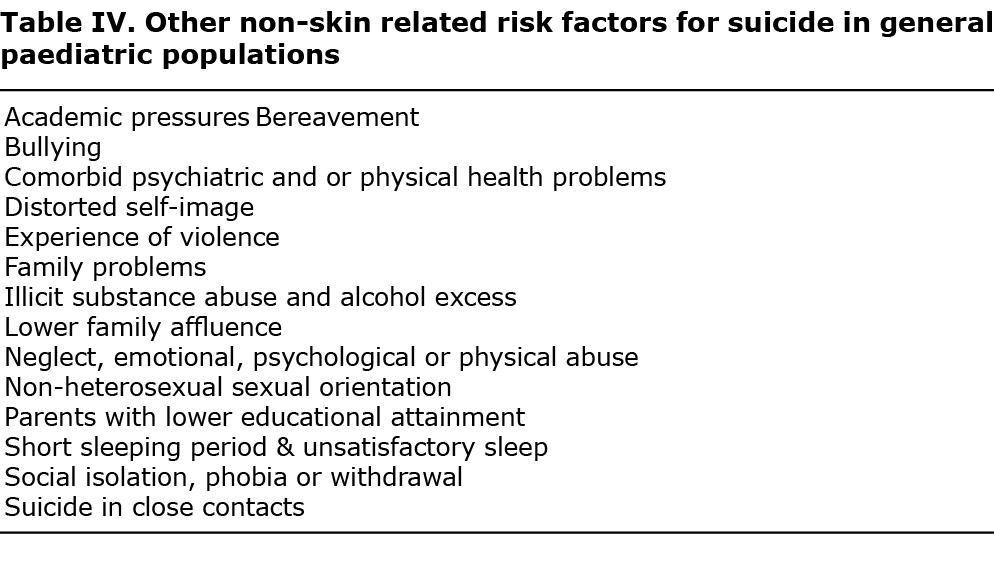
Non-skin related risk factors. The relationship between deliberate self-harm (DSH) and suicidal risk is complex, with the majority of patients demonstrating this behaviour not intending to commit suicide. Previous suicide attempts remain the leading risk factor for further attempts. Additionally, sexual abuse in childhood has been identified as a potent risk factor. Table IV demonstrates other non-skin related risk factors for suicide in general paediatric populations as well as other factors identified from the included studies.
Skin-related risk factors. Scarring and itching contribute to suicidal ideation in adolescence, comparable to chronic pain (35).
Vitamin D deficiency has been hypothesized to play a role in attempted and completed suicides, which peak in the spring when vitamin D levels are lowest in the Northern hemisphere. Low levels of 25(OH)D have been associated with pro-suicidal factors, such as worsening of depression, anxiety, psychosis and other medical conditions. There may be a protective role in these populations, although this relationship needs further exploration (36).
Whilst not a skin disorder, tattoos and piercings (T/P) can be used as a surrogate marker for other risk-taking behaviours. A cross-sectional survey examining 484 people, aged 12 years and over in the USA demonstrated a higher mean suicide index score in people with T/P, 1.28, compared with those without T/P, 0.83 (p = 0.028). The suicidal behaviour risk was higher at extremes of adolescence for people with tattoos and those with piercings aged over 11 years. Interestingly, the number of tattoos had no influence on risk-taking behaviour scores (suicide p = 0.683) (37). Scores for other risk- index taking behaviours, including disordered eating, gateway and hard drug use, and sexual behaviour were higher for those participants with 1 or more T/P. The authors did not declare what aspect of each risk-taking behaviour was specifically examined.
Conversely, there are numerous blog posts and videos on social media which document the use of T/P by people with BDD as a way of controlling their condition and empowering them to transform what they feel are problem areas into artistic pieces. Therefore, T/P and other forms of body art may well be markers for BDD.
Similarly, indoor tanning has been significantly associated with risk-taking behaviour including binge-drinking and unhealthy weight control in male and female students in the USA. In addition, indoor tanning was linked with promiscuity and illegal drug use in females, and taking steroids without prescription, smoking cigarettes and attempting suicide in males (p = 0.006) (38).
The variable findings of the 5 included studies demonstrate the complexity of suicidal risk in skin disorders amongst adolescents and children under the age of 18 years. Importantly, the suicidal risk remained after adjusting for depression, which suggests alternative mechanisms for observed behaviour, inflammation may provide us with part of the explanation (39).
Increased levels of TNF-alpha, IL-1β, IL-6 and IL-10 have been shown to be elevated in people with suicidal-related behaviour. Indeed, people with increased inflammation (CRP >3) have been shown to be up to 4 times more likely to commit suicide compared with CRP < 1 (40). It is thought that disordered inflammation can disrupt tryptophan catabolism which in turn alters the sensitivity of the HPA axis. It has also been postulated that the cytokine storm of COVID-19 may have a role in the psychiatric symptoms reported in people with long COVID (41). Additionally, NSAIDS and cytokine inhibitors may well work to augment antidepressant treatment response (39).
A clear risk for suicidal behaviour in mild to severe skin disorders in children and adolescents exists, and there may also be a risk for suicidal behaviour in close family members. However, there is obviously a distinct lack of scientific study in this population regarding this subject.
Three of the studies examined New Zealand and Korean adolescents; populations known to have higher than average suicidal risk compared with other adolescents. Despite this, the collated findings are applicable to our daily practice, given the sparsity of data. Critical appraisal was conducted using the Joanna Briggs Institute (JBI) Checklist for analytical cross-sectional studies (Table V).
Overall, these findings emphasize the necessity of a thorough examination of the skin, noting both endogenous and exogenous changes, in conjunction with a holistic assessment of the child or adolescent. Particular attention should be paid to the socioeconomic background, cultural aspects of the individual, progress in school and the family as a whole. These combined factors will generate insight into the complex risk of suicidal behaviour for the healthcare professional. Dermatologists should also be aware that they may be one of few people to see the entire canvas of a person’s identity through the lens of a skin examination.
ACKNOWLEDGEMENTS
The authors thank David Lewis Library Assistant Aneurin Bevan University Health Board (UHB) and Rosemary Soper, Cardiff and Vale UHB Librarian.
The authors have no conflicts of interest to declare.
REFERENCES
- Gray D, Coon H, McGlade E, Callor WB, Byrd J, Viskochil J, et al. Comparative analysis of suicide, accidental, and undetermined cause of death classification. Suicide Life Threat Behav 2014; 44: 304–316.
- Appleby L, Kapur N, Shaw J, Hunt IM, Flynn S, Ibrahim S, et al. The National Confidential Inquiry into Suicide and Homicide by People with Mental Illness. Making Mental Health Care Safer: Annual Report and 20-year Review. University of Manchester; 2016 [Cited 2022 March 12]. Available from: https://documents.manchester.ac.uk/display.aspx?DocID=37580.
- Odd D, Williams T, Appleby L, Gunnell D, Luyt K. Child suicide rates during the COVID-19 pandemic in England. J Affect Disord Rep 2021; 6: 1–6.
- Miron O, Yu KH, Wilf-Miron R, Kohane IS. Suicide Rates Among Adolescents and Young Adults in the United States, 2000–2017. JAMA 2019; 321: 2362–2364.
- Suicide in the world: global health estimates [Internet]. World Health Organisation; 2019 [Cited 2022 March 12]. Available from: https://apps.who.int/iris/handle/10665/326948.
- Kyu HH, Stein CE, Pinto CB, Rakovac I, Weber MW, Purnat TD, et al. Causes of death among children aged 5–14 years in the WHO European Region: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Child Adolesc Health 2018; 2: 321–337.
- Geulayov G, Casey D, McDonald KC, Foster P, Pritchard K, Wells C, et al. Incidence of suicide, hospital-presenting non-fatal self-harm, and community-occurring non-fatal self-harm in adolescents in England (the iceberg model of self-harm): a retrospective study. Lancet Psychiatry 2018; 5: 167–174.
- Jafferany M, Pastolero P. Psychiatric and Psychological Impact of Chronic Skin Disease. Prim Care Companion CNS Disord 2018; 26: 17nr02247.
- Gupta MA, Gupta AK, Ellis CN, Koblenzer CS. Psychiatric evaluation of the dermatology patient. Dermatol Clin 2005; 23: 591–599.
- Fergusson DM, Woodward LJ, Horwood LJ. Risk factors and life processes associated with the onset of suicidal behaviour during adolescence and early adulthood. Psychol Med 2000; 30: 23–39.
- Moola S, Munn Z, Tufanaru C, Aromataris E, Sears K, Sfetcu R, et al. Chapter 7: Systematic reviews of etiology and risk. JBI Manual for Evidence Synthesis. 2020. Available from https://synthesismanual.jbi.global.
- Purvis D, Robinson E, Merry S, Watson P. Acne, anxiety, depression and suicide in teenagers: A cross-sectional survey of New Zealand secondary school students. J Paediatr Child Health 2006; 42: 793–796.
- Bachmann C, Grabarkiewicz J, Theisen FM, Remschmidt H. Isotretinoin, depression and suicide ideation in an adolescent boy. Pharmacopsychiatry 2007; 40: 128.
- Schaffer LC, Schaffer CB, Hunter S, Miller A. Psychiatric reactions to isotretinoin in patients with bipolar disorder. J Affect Disord 2010; 122: 306–308.
- Jick SS, Kremers HM, Vasilakis-Scaramozza C. Isotretinion use and risk of depression, psychotic symptoms, suicide, and attempted suicide. Arch Dermatol 2000; 136: 1231–1236.
- Nevoralová Z, Dvořáková D. Mood changes, depression and suicide risk during isotretinoin treatment: A prospective study. Int J Dermatol 2013; 52: 163–168.
- Droitcourt C, Nowak E, Rault C, Happe A, Nautout BL, Kerbrat S, et al. Risk of suicide attempt associated with isotretinoin: a nationwide cohort and nested case-time-control study. Int J Epidemiol 2019; 48: 1623–1635.
- Gupta MA, Gupta AK. Depression and suicidal ideation in dermatology patients with acne, alopecia areata, atopic dermatitis and psoriasis. Br J Dermatol 1998; 139: 846–850.
- Picardi A, Mazzotti E, Pasquini P. Prevalence and correlates of suicidal ideation among patients with skin disease. J Am Acad Dermatol 2006; 54: 420–426.
- Rehn LMH, Meririnne E, Höök-Nikanne J, Isometsä E, Henriksson M. Depressive symptoms, suicidal ideation and acne: a study of male Finnish conscripts. J Eur Acad Dermatol Venereol 2008; 22: 561–567.
- Noh HM, Cho JJ, Park YS, Kim JH. The relationship between suicidal behaviors and atopic dermatitis in Korean adolescents. J Health Psychol 2016; 21: 2183–2194.
- Lee S, Shin A. Association of atopic dermatitis with depressive symptoms and suicidal behaviors among adolescents in Korea: The 2013 Korean Youth Risk Behavior Survey. BMC Psychiatry 2017; 17: 3.
- Kimata H. Prevalence of suicidal ideation in patients with atopic dermatitis. Suicide Life Threat Behav 2006; 36: 120–124.
- Khandaker GM, Zammit S, Lewis G, Jones PB. A population-based study of atopic disorders and inflammatory markers in childhood before psychotic experiences in adolescence. Schizophr Res 2014; 152: 139–145.
- Wamboldt MZ, Hewitt JK, Schmitz S, Wamboldt FS, Räsänen M, Koskenvuo M, et al. Familial association between allergic disorders and depression in adult Finnish twins. Am J Med Genet 2000; 96: 146–153.
- Gupta MA, Pur DR, Vujcic B, Gupta AK. Suicidal behaviors in the dermatology patient. Clin Dermatol 2017; 35: 302–311.
- Milch W, Wildt BT, Dieris B, et al. Suicidal ideation in adult patients with atopic dermatitis: a German cross-sectional study. Acta Derm Venereol 2017; 97: 1189–1195.
- Sandhu JK, Wu KK, Bui TL, Armstrong AW. Association between atopic dermatitis and suicidality: a systematic review and meta-analysis. JAMA Dermatology 2019; 155: 178–187.
- Albertini RS, Phillips KA. Thirty-three cases of body dysmorphic disorder in children and adolescents. J Am Acad Child Adolesc Psychiatry 1999; 38: 453–459.
- Phillips KA, Didie ER, Menard W, Pagano ME, Fay C, Weisberg RB. Clinical features of body dysmorphic disorder in adolescents and adults. Psychiatry Res 2006; 141: 305–314.
- Pellegrini L, Maietti E, Rucci P, Burato S, Menchetti M, Berardi D, et al. Suicidality in patients with obsessive-compulsive and related disorders (OCRDs): A meta-analysis. Compr Psychiatry 2021; 108: 152246.
- Kimball AB, Wu EQ, Guérin A, Yu AP, Tsaneva M, Gupta SR, et al. Risks of developing psychiatric disorders in pediatric patients with psoriasis. J Am Acad Dermatol 2012; 67: 651–657.
- Egeberg A, Hansen PR, Gislason GH, Skov L, Mallbris L. Risk of self-harm and nonfatal suicide attempts, and completed suicide in patients with psoriasis: a population-based cohort study. Br J Dermatol 2016; 175: 493–500.
- Sinclair RD. Alopecia areata and suicide of children. Med J Aust 2014; 200: 145.
- Halvorsen JA, Dalgard F, Thoresen M, Bjertness E, Lien L. Itch and pain in adolescents are associated with suicidal ideation: A population-based cross-sectional study. Acta Derm Venereol 2012; 92: 543–546.
- Tariq MM, Streeten EA, Smith HA, Sleemi A, Khabazghazvini B, Vaswani D, et al.Vitamin D: a potential role in reducing suicide risk? Int J Adolesc Med Health 2011; 23: 157–165.
- Carroll ST, Riffenburgh RH, Roberts TA, Myhre EB. Tattoos and body piercings as indicators of adolescent risk-taking behaviors. Pediatrics 2002; 109: 1021–1027.
- Guy GP, Berkowitz Z, Tai E, Holman DM, Jones SE, Richardson LC. Indoor tanning among high school students in the United States, 2009 and 2011. JAMA Dermatology 2014; 150: 501–511.
- Yan W-J, Jiang C-L, Su W-J. Life in the flame: Inflammation sounds the alarm for suicide risk. Brain Behav Immun Health 2021; 31: 100250.
- Batty GD, Bell S, Stamatakis E, Kivimäki M. Association of systemic inflammation with risk of completed suicide in the general population. JAMA Psychiatry 2016; 73: 993–995.
- Debnath M, Berk M, Maes M. Changing dynamics of psychoneuroimmunology during the COVID-19 pandemic. Brain Behav Immun Health 2020; 5: 100096.