SHORT COMMUNICATION
Atypical Herpes Simplex: An Important Diagnosis to Consider
Elisabet NYLANDER1, Daniel LIEB NOSEK2 and Fiona LEWIS3
1Department of Public Health and Clinical Medicine, Dermatology and Venereology, 2Department of Medical Biosciences, Umeå University, SE-90185 Umeå, Sweden and 3St John’s Institute of Dermatology, Guy’s & St Thomas’ NHS Trust, London UK. E-mail: elisabet.nylander@umu.se
Citation: Acta Derm Venereol 2023; 103: adv15324. DOI: https://doi.org/10.2340/actadv.v103.15324.
Copyright: © Published by Medical Journals Sweden, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: Jun 4, 2023; Published: Aug 16, 2023
Competing interests and funding: The authors have no conflicts of interest to declare.
INTRODUCTION
Herpes simplex is a common viral infection which is lifelong. There are two types of herpes simplex virus (HSV) that may cause genital herpes; HSV-1 and HSV-2. The WHO estimates that 67% under age 50 globally have HSV-1 and 13% HSV-2. Herpes simplex infection is nowadays diagnosed by PCR test from ulcers and blisters, also making it possible to differ between HSV-1 and HSV-2. Approximately 50–60% of women in Western countries are infected with HSV-1 and approximately 20% with HSV-2 (1). Herpes simplex infection is mainly asymptomatic, even the primary infection, and persons affected are often unaware of the disease (2), although they may shed virus and thus transmit the infection. In addition, older persons may have forgotten that they had an infection earlier in life. It is not known why some individuals infected with HSV-2 experience frequent recurrences, while most of those infected have a silent infection (3).
Recurrences are also often asymptomatic (4). When symptomatic, typical signs of herpes infection are groups of small vesicles and ulcers with background erythema accompanied by itch, burning and pain. Clinical signs can, however, be atypical, emphasizing the importance of suspecting herpes simplex when examining a patient with symptoms and signs but no clear diagnosis.
MATERIALS AND METHODS
Two (unrelated) women were, quite close in time, attending our Vulva Clinic, at the Department of Dermatology and Venereology, University Hospital, Umeå, Sweden, due to rapidly expanding ulcers in the ano-genital area. The symptoms had been present for a few weeks and rapidly deteriorated, making passing urine painful as well as causing constant burning of the vulva. Neither patient had fever or was systemically unwell.
Patient 1. 77 years old, was referred from a gynaecological clinic at another hospital. She had a former diagnosis of an autoimmune disease, vasculitis, which was treated with prednisolone, 30 mg a day, and methotrexate, which had been temporarily stopped. The patient had undergone surgery several years ago due to thyroid malignancy. When attending our clinic, she reported 4 weeks of painful ulcers in the ano-genital area. She denied having had similar symptoms previously.
On examination she had erosions on the left labium majus, extending towards the buttocks and perianally, and on the edges of clitoris and the clitorial prepuce (Fig. 1). The clinical picture was quite atypical. Swabs for candida, bacteria and herpes simplex were taken and 3 biopsies had been taken by the referring gynaecologist.

Fig. 1. Patient 1 at initial presentation to the clinic. The dark ulcers are due to biopsies a few days previously.
Patient 2. 79 years old, had a previously suggested diagnosis of atypical psoriasis and 1 year before attending, bullous pemphigoid was postulated, but never confirmed. She was otherwise healthy and appeared at the clinic with 3 weeks’ history of vulval pain and itch. Before attending she had used an ultrapotent corticosteroid ointment with only little relief of the symptoms. On examination she had changes in the whole vulva, erythema on the inner aspects of labia minora, with more erosions on the left than the right side, and some brown-white hyperkeratotic round areas near the anterior commissure and on the labia majora. In the vagina the mucous membrane was hyperkeratotic (Fig. 2). Swabs and 2 biopsies were taken.

Fig. 2. Patient 2 at initial presentation to the clinic.
RESULTS
Patient 1. The swabs taken from the ulcers were positive for Candida albicans, skin bacteria and HSV-2. One of the biopsies also confirmed the findings of herpes simplex (Fig. 3). The biopsies were characterized by ulceration and a dense mixed infiltrate of plasma cells, neutrophils, and some eosinophils. In one of the biopsies there was an area with viable epithelium, showing typical changes for herpes simplex infection: acantholysis (loss of coherence between epidermal cells due to the breakdown of intercellular bridges) and multinucleate pale keratinocytes with steel-grey nuclei and nuclear moulding (conformity of adjacent cell nuclei to one another). Some pink intranuclear inclusions surrounded by an artefactual cleft (Cowdry type A inclusions) could also be seen. (There were signs of dermal necrosis and reactive vascular changes, but no vasculitis.) There were no signs of dysplasia (Fig. 3A).
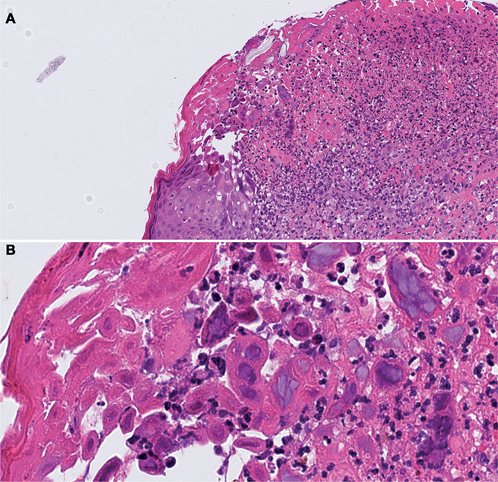
Fig. 3. Biopsy from the lesion in patient 1, showing typical lesions for herpes virus (acantholysis, multinucleate pale keratinocytes with steel-grey nuclei and nuclear moulding). (A) An overview of the skin with ulceration and a mixed inflammatory infiltrate. (B) Acantholysis, nuclear molding and focally, pink intranuclear inclusions (Cowdry type A inclusions). Scanned at 40X magnification, presented in (A) 20X and (B) 80X digital zoom*. H&E stain. *Corresponding to 0.23 microns per pixel.
Patient 2. Swabs taken from the ulcers were positive for Candida albicans as well as for HSV-1. Staphylococcus aureus was also seen. The biopsies showed only inflammation and hyperplasia.
Both patients denied having had herpes infection previously. The patients were both treated with valaciclovir, with the usual dose 500 mg twice a day for 10 days, due to diminished or suspected diminished function of the kidneys, respectively. They were also treated with fluconazole, 150 mg, for their Candida infection and lidocaine 5% ointment for pain relief. Patient 2 also received flucloxacillin for 1 week.
The women both started recovering from their symptoms within days. Due to relapse of the burning sensations and pain a few weeks later they both received another 10-day course of the antiviral medication and the symptoms ceased again.
DISCUSSION
Both of these patients presented with symptoms that were not typical of any genital dermatological disease. When patients attend and symptoms do not clearly fit into a well-known disease it is important to consider a new perspective. Examining both patients evoked the suspicion that the changes could be due to dysplasia or even have malignant potential.
When patients present with ano-genital ulceration herpes simplex should always be considered, which may seem atypical and even mimic other diseases. Anamnesis is of little help, as these patients both denied ever having had herpes infection. It is important to take PCR tests and start treatment as soon as possible. Symptoms ceased soon after administrating antiviral medication (valaciclovir). The patients’ histories also indicate that treatment must be extended for a longer time than usual to avoid a quick relapse.
This report is also in agreement with the report by Laerke Sand & Thomsen (1), that in older immunosuppressed women an initial non-primary infection may mimic a primary infection with disseminated lesions.
ACKNOWLEDGEMENT
The patients provided written informed consent.
REFERENCES
- Laerke Sand F, Thomsen SF. Skin diseases of the vulva: infectious diseases. J Obstet Gynaecol 2017; 37: 840–848.
- WHO Newsletter April 2023. Available from: who.int/newsroom/fact sheets/detail/herpes simplex virus
- Löwhagen G-B, Bonde E, Forsgren-Brusk U, Runeman B, Tunbäck P. The microenvironment of vulvar skin in women with symptomatic and asymptomatic herpes simplex virus type 2 (HSV-2) infection. J Eur Acad Dermatol Venereol 2006; 20: 1086–1089.
- Omarova S, Cannon A, Weiss W, Bruccoleri A, Puccio J. Genital herpes simplex virus – an updated review. Adv Pediatr 2022; 69:149–162.