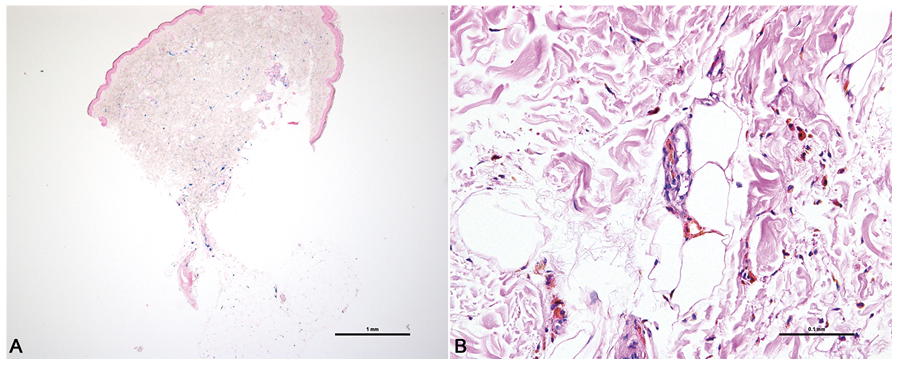
Fig. 1. Histopathological findings. (A) Iron deposit (Berlin-blue stain x20) in the whole dermis (predominantly 2–3 mm depth) and subcutis. (B) Presence of macrophages with phagocytosed hemosiderin (haematoxylin-eosin stain x200).
1Department of Dermatology, Inselspital, Bern University Hospital, University of Bern, Switzerland, 2Centro Studi GISED, Bergamo, Italy, 3Skinpulse Dermatology & Laser Centre, Geneva, and 4Department of Dermatology, Centre Hospitalier Universitaire Vaudois (CHUV), Lausanne, Switzerland
Intravenous ferric carboxymaltose is increasingly used to treat iron deficiency. However, a common side-effect is paravenous extravasation of iron preparations, resulting in cutaneous siderosis. Quality-switch-ed (QS) lasers and, recently, picosecond (PS) lasers have been used to treat these hyperpigmentations with variable success. The optimal treatment protocol remains unclear. The aims of this study were to assess the response of cutaneous siderosis to treatment with pigment lasers and to determine the optimal wavelength, number of treatment sessions and pulse duration. Fifteen patients with cutaneous siderosis on the arms were included. The effectiveness of laser treatment was evaluated using a 5-point standard Physician Global Assessment (PGA) grading system. Differences in continuous variables between distinct groups of patients were assessed with a Mann–Whitney U test. In all 15 patients clearance of at least 50% was obtained. In 12 patients, at least 75% of pigment was removed. In conclusion, pigment lasers are an effective and safe method to treat cutaneous siderosis.
Key words: siderosis; iron; laser.
Accepted Apr 28, 2020; Epub ahead of print May 4, 2020
Acta Derm Venereol 2020; 100: adv00148.
Corr: Kristine Heidemeyer, Department of Dermatology, University Hospital, Inselspital, Freiburgstrasse, CH-3010 Bern, Switzerland. E-mail: Kristine.heidemeyer@insel.ch
Intravenous iron solution drugs are increasingly used to treat iron deficiency. A rare side-effect is paravenous extravasation of iron preparations, resulting in cutaneous siderosis. Pigment-targeting lasers have been used to treat these hyperpigmentations with variable success. The optimal treatment protocol remains unclear. This retrospective study with 15 patients aimed to assess the response of cutaneous iron deposit after treatment with pigment lasers and to determine optimal treatment parameters. The effectiveness of laser treatments was evaluated using a 5-point grading system. In all 15 patients a clearance of at least 50% was obtained. In 12 patients, at least 75% of pigment was removed.
Iron deficiency is the most common nutritional disorder worldwide and the most common cause of anaemia. Iron deficiency affects more than 2 billion people worldwide. In Europe, the prevalence of iron deficiency has been estimated at between 12% and 40% (1, 2).
Lack of iron may result in chronic fatigue, depression, restless legs syndrome, irritability and hair loss (2–4). Parenteral iron replacement has become popular in recent decades, particularly in patients with intolerable side-effects with oral treatment, non-compliance or unsatisfactory effect of oral supplementation. In Switzerland, parenteral iron replacement has been increasingly used in primary care centres, and its use is 1,000-fold higher than in the UK (1). Ferric carboxymaltose is, by far, the most used drug in Switzerland for intravenous iron supplementation. In addition to serious side-effects, including fatal allergic reactions (5), another well-recognized complication is the development of a greyish-brown hyperpigmentation as a result of the paravenous leakage of intravenous iron, leading to cutaneous siderosis (6–8). Due to this poor aesthetic appearance, there is a strong need for efficient treatments. To date, however, there are scant data in the literature about the possible and most efficient therapeutic options. Treatments with quality-switched (QS) lasers are reported in a few cases with different wavelengths: 532, 755 and 1,064 nm (6, 7, 9–12). QS lasers, developed in the 1980s, are efficient in the removal of exogenous and endogenous pigments, such as tattoos, as well as epidermal and dermal melanin lesions. They were the first lasers to demonstrate usefulness in the removal of pigments by selective photothermolysis, with good aesthetic outcome (13). The laser light emitted at 10–9 s is absorbed by pigment particles, leading to fragmentation of these particles by a photothermal and photoacoustic effect. Smaller particles can be then phagocyted by macrophages, and transported via the lymphatic system into the lymph node (14). Furthermore, there are reports describing the successful use of QS lasers in the management of cutaneous siderosis in stasis dermatitis and after sclerotherapy (6).
Recently, the development of picosecond (PS) lasers has provided a new tool for pigment removal. Due to a shorter pulse duration (300–750 10–12 s), PS lasers are more efficient than QS lasers in removing exogenous pigments, by acting with a stronger photoacoustic effect, leading to a smaller fragmentation of the pigments (15). However, there is debate about the superiority of PS lasers, which may act more in a sub nano-spectrum domain. In fact, in some reports, the PS lasers did not appear to show a significant advantage for the treatment of tattoos compared with QS lasers (16). The current study aimed to evaluate the efficacy of pigment-lasers in treating cutaneous siderosis and to explore the effect of other clinical variables on treatment response.
Study design
A retrospective analysis was conducted of 15 consecutive female patients treated with lasers for cutaneous siderosis occurring after extravasation of iron preparations. The study was performed between January 2011 and August 2019. None of the patients received any previous treatment. Patients were identified in our electronic medical report database by the keywords “iron” and “siderosis”. Two identified patients were not included as they were in poor general health and did not want to travel. Relevant data (demographics, localization, type of laser, wavelength, treatment session, time to treatment start, time to last picture, side-effects) were collected in a standardized clinical report form. The Ethics Committee of the Canton of Bern, Switzerland (project ID 2019-01632) approved the study.
Treatment protocol
All patients, except one, were treated with QS lasers, including QS Nd:YAG laser (Revlite and Medlite C6, Cynosure, Westford, MA, USA) at 1,064 nm or frequency doubled (a mechanism generating radiation with the double frequency of the initial laser wavelength, using a non-linear optical material) at 532 nm (in 14 cases). One patient was treated with a QS ruby laser, at 694 nm (Sinon, Alma Lasers, Caesarea, Israel). Eleven patients were treated with a wavelength of 1,064 nm, 2 with a combination of 1,064 nm and 532 nm, one with 532 nm and one with 694 nm. A spot size of 4 mm was used with the ruby laser, while spot sizes of 4–6 mm were used with the Nd:YAG laser, depending on the fluence required. When the fluence needed could not be produced by the laser with the 6-mm spot, the spot size was changed to 4 mm to be able to increase the fluence. All patients were treated with a fluence leading to an endpoint of a slight purpura. Because of pigment lightening after each session, the fluence was increased at each session to reach the endpoint mentioned above (fluence range: 1,064 nm/6 mm: 0.9–5.8 J/cm2; 1,064 nm/4 mm: 2.1–7.9 J J/cm2; 532 nm/6 mm: 0.5–1.4 J/cm2; 532 nm/4 mm: 1.6–2.2 J/cm2). Pulse duration in our device is fixed at 5–20 ns. Treatment was performed with 10 Hz frequency. No topical anaesthesia was used.
Post-treatment care included sunscreen SPF 50+, and after the first few sessions, a medium-potency topical steroid (mometason fuorate cream) was given. The treatment interval was a minimum of 4 weeks. Treatment was stopped when the patient was satisfied with the aesthetic result and therefore declined further treatment sessions.
In one patient a split-lesion trial was performed with PS 1,064 nm and QS 1,064 nm.
Histological examination
In one case, light microscopy studies of a skin biopsy obtained from an untreated cutaneous area of siderosis were performed to better assess the pigment distribution and pigment depth. The histological findings showed a hemosiderosis with presence of macrophages with phagocytosed hemosiderin present up to the subcutaneous fat. The deposits were predominantly found 2–3 mm deep, but could also be observed at the lowest margin of the biopsy specimen at a depth of 5 mm (Fig. 1).
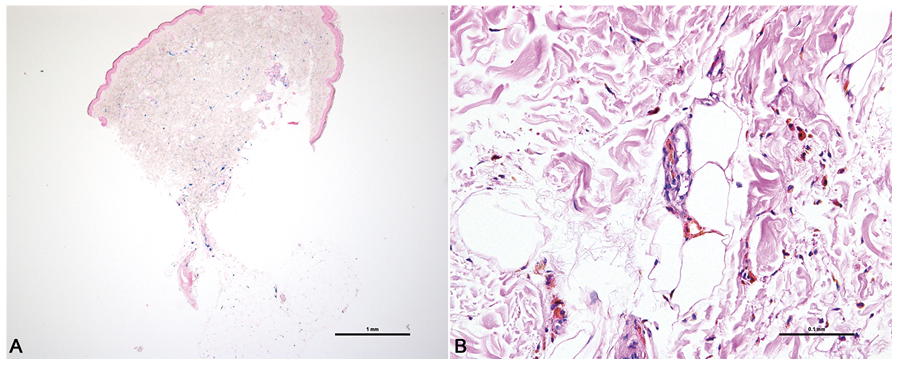
Fig. 1. Histopathological findings. (A) Iron deposit (Berlin-blue stain x20) in the whole dermis (predominantly 2–3 mm depth) and subcutis. (B) Presence of macrophages with phagocytosed hemosiderin (haematoxylin-eosin stain x200).
Evaluation by Physician Global Assessment grading system
Standardized photographs were taken of patients’ iron siderosis before and at the earliest 6 weeks after treatment. Five independent board-certified dermatologists evaluated clinical improvement, defined as clearance of lesion according to a 5-point standard Physician Global Assessment (PGA) grading system. The following scale was used: 1: <25%, 2: 25–49%, 3: 50–74%, 4: 75–90%, and 5: >90%.
The median PGA among all raters (n = 5) was taken as the main study outcome and its distribution was tested against a reference score of 2 points in the PGA scale (poor improvement).
Statistical analysis
Descriptive statistics were reported as absolute and relative frequencies for nominal variables, while means with standard deviations (SD) and medians with ranges were used for continuous variables. One sample Wilcoxon signed-rank test was used to assess overall PGA difference from a reference score of 2. PGA differences between distinct groups of patients were assessed by using Mann–Whitney U test. For continuous variables, the optimal cut-off threshold was computed based on the significance of the test.
Absolute agreement among assessors for the overall PGA was calculated by using intraclass correlation coefficient (ICC) with 2-way random mean measure and reported with its 95% confidence interval (95% CI). All tests were considered statistically significant at p-value < 0.05. Analyses were performed with SPSS v.26 (IBM Corp. Armonk, NY, USA).
Demographics and treatment location
All 15 patients were female, with a Fitzpatrick’s skin photo-type I–IV. The median age at first treatment was 43 years (range 15–66 years). Cutaneous siderosis was found on the elbow pit in 12 (80%) of 15 patients and on the wrist in the remaining 3 patients (20%). A total of 2–9 treatment sessions were performed (mean ± SD: 4.5 ± 2.4). The mean ± SD treatment interval was 2.4 ± 1.0 months (range 4–45 weeks). The mean ± SD time from iron perfusion to initiation of laser treatment was 9.6 ± 5.3 months (Table I).
Correlation between overall PGA and follow-up time was not significant (p = 0.29).

Table I. Survey of the clinical characteristics and treatment protocol of the 15 patients
Clearance according to Physician Global Assessment
The overall median PGA of 4 (range 3–4) was significantly higher than a reference value of 2 (poor improvement). Five of the patients (33.3%) had an overall clearance rate of 5, corresponding to a response of over 90%. Hence, all patients achieved a clearance of at least 50%. The ICC among assessors for the overall PGA is 0.76 (95% CI: 0.50–0.91), corresponding to a substantial agreement (Table II).
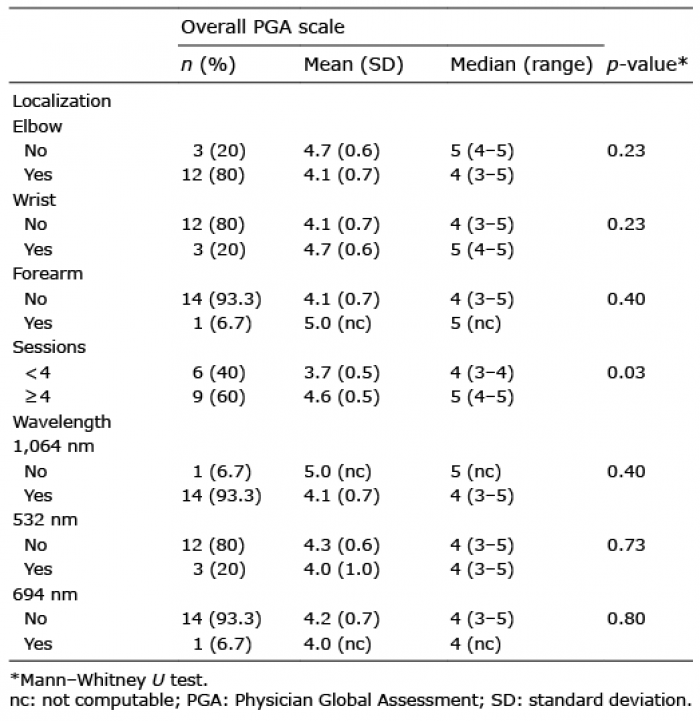
Table II. Overall efficacy according to localization, number of sessions and wavelength of laser
Anatomical location
It was observed that more laser sessions (7.3 ± 2.9) were needed to achieve patient satisfaction when treating cutaneous siderosis on the wrists compared with other anatomical locations (3.8 ± 1.7) (p = 0.048). No significant difference was observed between other anatomical locations. In general, a better clearance rate was observed when the treatment was performed over 4 or more sessions (p = 0.03).
Wavelength
There were apparently no significant differences in terms of efficacy between 1,064 nm and 532 nm (single or in combination with 1,064 nm). The number of treatment sessions was independent of the wavelength used.
Pulse duration
In one patient, a split treatment with QS laser and PS laser was performed during the first session. A slightly better clearance was observed with QS lasers.
Side-effects
During laser treatment, all patients felt a burning sensation, but no anaesthetic ointment was needed or requested by the patients. The slight purpura obtained as the endpoint of the treatment invariably resolved within 10 days in all patients. In one case (Fitzpatrick’s skin photo-type III), temporary hyperpigmentation and prolonged erythema were observed after treatment with QS and PS at 532 nm. These side-effects disappeared spontaneously within 4 months. No other persistent side-effect was observed.
Paravenous leakage of intravenous iron at the infusion site results in circumscribed greyish to brown hyperpigmentation in 1.6–1.8% of treated patients (8). Skin hyperpigmentation is persistent and does not resolve spontaneously, causing significant psychological stress for patients. Using light microscopy studies, the exogenous pigment is found within numerous macrophages in all dermal layers as well as in the subcutaneous fat tissue. Therefore, superficial treatments, such as creams, peelings and dermabrasion, are not effective (12).
Only a few case reports and one case series, focusing on the effectiveness of removal of cutaneous siderosis, have been published in English (6, 7, 9–12). The current retrospective study of 15 treated patients represents the largest series reported so far. The findings show that QS lasers are efficient and useful in the management of cutaneous siderosis due to paravenous leakage of intravenous iron (Fig. 2). With a mean of 4.5 treatment sessions, a clearance of at least 50% was observed in all patients.
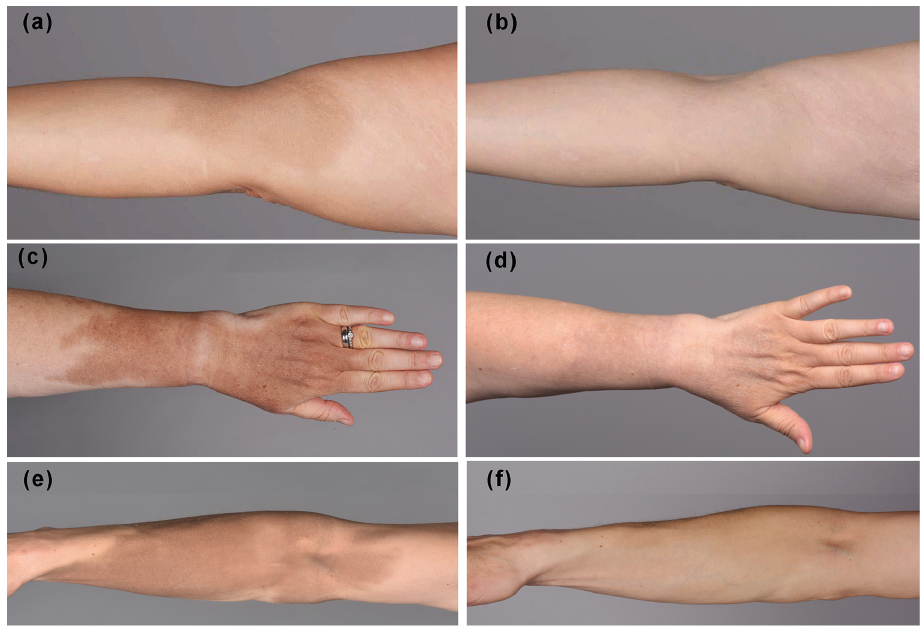
Fig. 2. Treatment of cutaneous siderosis with quality-switched (QS) lasers. Lesion in the elbow (a) before and (b) after 5 treatment sessions with QS 1,064 nm laser. Cutaneous siderosis on the wrist (c) before and (d) after 9 sessions with QS 1,064 nm laser. Lesion on the elbow and forearm (e) before and (f) after 6 laser sessions with QS 1,064 laser.
For most patients a QS YAG laser at 1,064 nm was used to remove the pigment. A few lesions were also treated with other wavelengths (either 532 nm or 694 nm) or with shorter pulse durations (350–550 ps). As we performed these comparisons only within the first session, it is difficult to draw any conclusion as to which wavelength or which pulse duration is superior. This can be explained both by the limited study sample size and power for this kind of analysis. Furthermore, the different wavelengths have advantages and disadvantages concerning their penetration depth and absorption peak. Iron has a major absorption peak at 410–415 nm (6). Ferric carboxymaltose has no distinct maximum absorption wavelength. However, there is an absorption band at around 470–500 nm (17, 18), explaining the good response to 532 nm lasers. Nevertheless, it is likely that the comparable overall rating of the 532 nm and 1,064 nm wavelength is that the penetration depth of the 532 nm wavelength is not deep enough. Furthermore, the risk of post-inflammatory hyperpigmentation is higher with the 532 nm than the 1,064 nm wavelengths, especially in darker skin types. The latter may thus pose a dilemma for both the treatment and evaluation by the physician. In one patient, combined treatment was given: QS 532 nm followed by QS 1,064 nm. However, the results obtained in this case do not support the idea that the combination is superior to the use of a single wavelength. Our overall findings indicate that more than 4 treatment sessions resulted in a better response rate. In analogy with what has been observed and reported for tattoos on the extremities, such as wrist and ankle, successful treatment of cutaneous siderosis involving the wrist required more treatment sessions.
Besides the wavelength, spot size also influences the penetration depth of the laser. Light scatters at the border of the target zone (19). Therefore, a smaller spot size will result in a greater proportion of the light being scattered, leading to less depth in penetration of light.
As the pigment in cutaneous siderosis is lying deep, the largest possible spot-size with the required fluence should be chosen in order to reach the deepest pigment possible.
Side-effects were limited to a mild burning sensation, lasting a few hours and a slight purpura, resolving within 7–10 days. We did not observe any case of hypopigmentation or blistering, as reported in another case series (12). These complications are probably best avoided by adapting wavelength to the skin type.
Some papers describe that PS lasers are more efficient in tattoo removal than QS lasers (15), excluding some above-mentioned exceptions. Considering histological similarities between iatrogenic cutaneous siderosis and decorative tattoos, it was a reasonable assumption that PS lasers would have been more efficient than QS lasers in the removal of cutaneous siderosis. Furthermore, the median core diameters of the 2 available ferric carboxymaltose products in Switzerland are 5.0 ± 0.8 nm (Venofer®, Venofer, Vifor (International) Inc., St. Gallen, Switzerland) and 11.7 ± 44 nm (Ferinject®, Vifor (International) Inc.) (20). These reported sizes are therefore even smaller than the mean size of a black ink particle (50–400 nm), a further reason that PS lasers should be more efficient. Nonetheless, in our split-lesion case, there was no obvious difference between the observed results. Nevertheless, additional studies that include a larger number of cases are required to definitively address this issue.
In conclusion, physicians should be familiar with the best treatment options of iatrogenic cutaneous siderosis, as increasing cases can be expected. Our retrospective study indicates that QS lasers are an effective and safe method. Different wavelengths appear to be useful for treatment, because the penetration depth (which is deeper with longer wavelength) is equally important as the absorption peak of iron (415 nm). Somehow, surprisingly our preliminary findings do not support the ideas that PS are more efficient than QS lasers in the removal of cutaneous siderosis, although the particle size of iron particles is very small. However, randomized controlled trials with a higher number of patients are needed to draw any definitive conclusion.
The authors have no conflicts of interest to declare.