Table I. Distribution of socio-demographic variables for each disease
1French Society of Dermatology (SFD), 2College of Dermatology Teachers of France (CEDEF), Paris, 3Dermatology Department, University Hospital of Brest, 4University of Brest, Laboratory Interactions Epitheliums-Neurons (LIEN), Brest, 5French Federation of Continuing Education and Evaluation in Dermatology-Venerology, (FFFCED), Paris, 6Dermatology Department, University Hospital of Rouen, Rouen, and 7Aix-Marseille University, Health Service Research and Quality of Life Center, Dermatology Department, Timone Hospital, Assistance Publique Hôpitaux de Marseille, Marseille, France
The prevalence of psychological disorders in patients with common skin diseases was assessed in a large representative sample of the French adult population. General health, as measured by the EQ5D score, was significantly lower if patients reported having rosacea, atopic dermatitis, urticaria, fungal infections, psoriasis or acne. The proportions of participants reporting being extremely anxious or depressed were higher in those who reported having rosacea, atopic dermatitis or contact dermatitis. Difficulties in sexual and conjugal life were frequently reported by people with psoriasis, atopic dermatitis, contact dermatitis, urticaria and, in particular, acne. Sleep disorders were present in 30–50% of those who reported having acne, rosacea, eczema, psoriasis or urticaria. Sleep disorders may be related not only to pruritus, but also to disfiguring skin diseases. Anxiety and depression complications were mainly reported by those with disfiguring diseases. Sexual and conjugal dysfunctions were associated with all dermatoses (with the exception of warts).
Key words: atopic dermatitis; psoriasis; urticaria; acne; rosacea; mycosis; psyche; psychological.
Accepted May 19, 2020; Epub ahead of print May 25, 2020
Acta Derm Venereol 2020; 100: adv00175.
Corr: Laurent Misery, Department of Dermatology, University Hospital, FR-29609 Brest, France. E-mail: laurent.misery@chu-brest.fr
Anxiety, depression, sleep disorders, as well as sexual/conjugal difficulties are frequent among patients with common skin diseases.
Although numerous studies have shown that anxiety, depression, suicidal ideations, sleep disorders and sexual disorders are frequently observed in patients with psoriasis, atopic dermatitis, acne, alopecia areata, vitiligo, urticaria, hidradenitis suppurativa or other dermatological diseases, data on the epidemiology of psychiatric comorbidities of skin diseases are, to date, still scant. Only rare population-based studies have demonstrated significant associations of acne, eczema and psoriasis with suicidal thoughts (1–3).
More recently, an international multicentre observational cross-sectional study was conducted in 13 European countries to ascertain the association between depression, anxiety and suicidal ideation in various dermatological diagnoses (4). A total of 4,994 participants (3,635 patients and 1,359 controls) were recruited. Clinical depression was present in 10.1% of patients (controls 4.3%). Clinical anxiety was present in 17.2% (controls 11.1%, odds ratio (OR) 2.18). Suicidal ideation was reported by 12.7% of all patients (controls 8.3%, OR 1.94). For individual diagnoses, only patients with psoriasis had a significant association with suicidal ideation. The association with depression and anxiety was highest for patients with psoriasis, atopic dermatitis, hand eczema, and leg ulcers. The main limitation of this impressive study was that patients were recruited only among outpatients from departments of dermatology.
In this context, the French Society of Dermatology, the French College of Dermatology Teachers and the French Federation of Continuing Medical Education in Dermatology performed a population-based survey to assess the prevalence of skin diseases and skin demands in France, including data about their psychological and psychiatric consequences. This study is the second study conducted in the framework of the Objectifs Peau study (5, 6). The current study focused on quality of life, an-xiety, depression, sleep disorders and sexual or affective life among French people with skin diseases vs people without any skin disease.
Because this study used completely anonymized data and did not involve patient contact, institutional review board approval was not required.
A panel of experts including dermatologists and public health specialists developed a questionnaire that included various items specifically related to socio-demographics (sex, age, occupation, marital status, area of residency, and total income, among others) and health/comorbidities across the French population aged >15 years. Participants were also asked to declare if they had been previously concerned with one or more skin problems or skin diseases during the last 12 months, referring to a preselected list of the most common 31 skin diseases, including atopic dermatitis, psoriasis, alopecia areata, vitiligo and hidradenitis suppurativa, for which validated self-reported questionnaires were used to confirm the diagnosis, as described previously (5, 7, 8).
All participants were asked to complete the EQ5D questionnaire, which is a standardized generic instrument known to be a valuable instrument to assess the impairment of health-related quality of life (HRQoL) in patients with skin diseases (9, 10). The EQ5D consists of 2 parts (11). The EQ visual analogue scale (EQ-VAS) records respondents’ self-rated health on a visual analogue scale, ranging from 0 to 100, which correspond to the worst and the best imaginable health states, respectively. This information can be used as a quantitative measure of health outcome, as judged by the individual respondent. The EQ5D further assesses health status across dimensions of: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. Each health dimension has 3 response levels: “no problems”, “some problems” and “extreme problems”. The EQ5D reflects the current general health status. The validity and responsiveness of the EQ5D was found to be good in people with skin diseases (for psoriasis, and to a lesser extent for hidradenitis suppurativa, acne vulgaris and chronic venous ulcers) (10).
Questions on the impact of skin diseases (i.e. ”Because of my skin disease I tend to be withdrawn into myself”/”Because of my skin disease my relations with my partner are difficult”/”My skin disease affects my sexual life”/”Because of my skin disease I have sleep disturbances”) were the result of discussions with patients. Indeed, the questions were constructed within the framework of discussion groups with patients from patients’ associations, which were led by a sociologist, a psychologist and a patient-related outcome expert. The objective of these groups was to collect the patients’ verbatim reports to identify their most frequent problems.
The survey was conducted by a polling institute (HC Conseil Paris, France) between 1 September and 30 November 2016. A representative sample of the general population aged more than 15 years was recruited using a stratified proportional, sampling-with-replacement design. Proportional quota sampling was used to make the population representative of the French general population according to data of the French population published by the National Institute for Statistics and Economic Studies Institute (INSEE). Based on a database that contained the e-mail addresses of 900,000 internet users who agreed to participate in surveys (megabase-Quantar), fixed quotas of subjects fulfilling predefined socio-demographic criteria were decided. Thus, the sample was constructed on a double stratification of age * sex combined with the geographical area of residency. Data were collected via the internet by random selection of 20,000 persons from 900,000 internet users over the age of 15 years, who agreed to participate in surveys. Each selected participant was contacted by e-mail. If contact was not achieved, another potential participant with the same characteristics was randomly selected. Further details on the methodology of the Objectifs Peau study have been given elsewhere (7).
Statistics
Direct standardization was applied to allow for subgroup comparisons using the projected French population in 2015 according to the 2015 census of the French National Institute for Statistics and Economic Studies Institute (INSEE) for the following 6 age groups: 0–17, 18–29, 30–39, 40–49, 50–59, and ≥60 years. Crude and standardized prevalence estimates were calculated based on participants with available socio-demographic information. Confidence intervals for crude and standardized prevalence rates were computed using the Wilson score method (12) and gamma distribution (13), respectively. Standardized prevalence rates were compared assuming the prevalence ratio followed a log-normal distribution. Age-specific prevalence rates were compared using the χ2 test or Fisher’s exact test, as appropriate. A 2-sided α level of 0.05 was applied to determine statistical significance. All analyses were performed using SAS software (version 9.4; SAS Institute, Inc.).
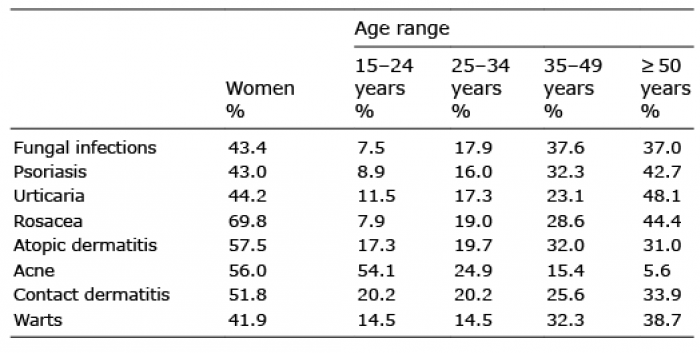
The initial contact participation rate for the digital study was 72% (5). Of the 20,012 participants who responded to the questionnaire, 9,760 were men (48.8%) and 10,252 (51.2%) were women. Further details are shown in Table I.
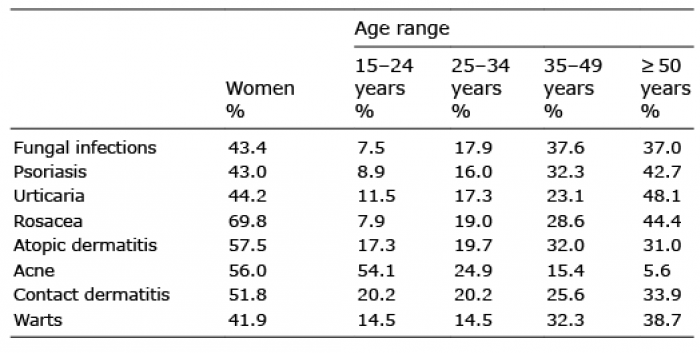
Table I. Distribution of socio-demographic variables for each disease
The EQ-VAS score was 76.8 in people who did not report any skin disease and 70.4 in those reporting at least one skin disease (p < 0.001). The score was similar in patients with warts or contact dermatitis vs people without these diseases. Significant differences were noted between healthy subjects (76.8 ± 8.1) and patients with any skin disease (70.4 ± 20.4) (p < 0.001) (Table II), revealing an impact on quality of life.
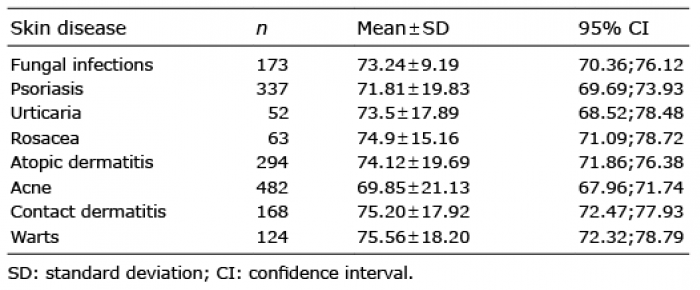
Table II. EQ visual analogue scale (EQ-VAS) scores according to the main skin diseases
One question of the EQ5D focuses on anxiety or depression, with no distinction between them. In total, 69.2% of French people who did not report any skin disease did not report being anxious or depressed, while only 46.7% among those reporting at least one skin disease did not report being anxious or depressed (p < 0.001). The proportions of people feeling moderately and extremely anxious or depressed among people with skin diseases vs those without any are shown in Table III. In all skin diseases studied (including warts and contact dermatitis), these proportions were significantly higher than those in controls.
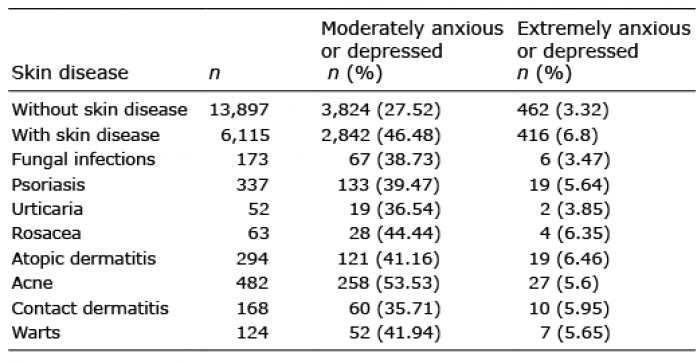
Table III. Proportions of people feeling moderately and extremely anxious or depressed. In all skin diseases studied, these proportions were significantly higher than those in controls (p < 0.001)
Some practical consequences of psychological distress were also evaluated using specific items on inward-looking attitudes, as well as the presence of sexual and conjugal difficulties and sleep disorders (Table IV). Between 20% and 30% of patients with psoriasis, atopic dermatitis, contact dermatitis or urticaria were withdrawn into themselves, whereas this was the case for more than 50% in individuals reporting acne. Difficulties in sexual and conjugal life were reported by 10–20% of people with psoriasis, atopic dermatitis, contact dermatitis or urticaria (but 5% for warts and 35% for acne). Sleep disturbances were present in 30–50% of patients who reported acne, rosacea, eczema, psoriasis or, especially, urticaria, but sleep disturbances were < 20% in those reporting warts or fungal infections or without dermatitis.

Table IV. Consequences of skin diseases on psychological distress
This study shows that the frequency of symptoms of psychological distress and alterations in quality of life is much higher in patients with skin diseases than in those without skin conditions. The main strength of this study was the large representative French population-based sample that allows extrapolation to the French population.
Although there is obviously no hierarchy of suffering between different diseases, our results were sometimes surprising, especially those obtained in patients with benign diseases such as warts or mycoses. Like cosmetic disorders (6), these conditions are associated with some impairment of quality of life. We found a lower impact of contact dermatitis than in previous studies (4, 14), which might be due to misdiagnosis by patients. The impairment of quality of life according to the measurement of EQ-VAS is less severe in the current study than in the previous study from the European Society for Dermatology and Psychiatry (ESDaP) (4), confirming that the recruitment of inpatients from dermatology departments in the ESDaP study was performed on patients with more severe illness and was therefore not generalizable to the entire skin disease population. In the current study, QOL impairment was most severe in patients with psoriasis and acne.
The EQ5D question on depression/anxiety is poorly discriminative, since it merges anxiety and depression. Nonetheless, it could be considered a convenient tool to roughly separate patients with moderate or severe psychiatric comorbidity from those without this comorbidity. It is less accurate than detection with the Hospital Anxiety and Depression Scale, which detects fewer patients (4). In any case, our results confirm that the feelings of being depressed or anxious are more common in patients with skin diseases, including the less severe skin diseases than in controls, and it is notable that these feelings mainly complicated visible diseases. Interestingly, our results on acne are not restricted to adolescents, who are known to suffer significantly from acne (2).
Surprisingly, there are very few studies on sleep disorders in patients with dermatological diseases (15). The relationship between sleep disorders and skin diseases is multifactorial: the presence of itch and pain, as well as comorbidity with anxiety, depression or other associated diseases.
Sleep disorders can be related to pruritus, especially urticaria, but also to disfiguration that pertains to a number of skin diseases, such as acne. In patients with psoriasis and psoriatic arthritis, sleep disorders might be related to an increased prevalence of obstructive sleep apnoea (OSA), restless legs syndrome (RLS) and insomnia, as shown in a recent systematic review (16). Moreover, symptoms of insomnia in patients with psoriasis can also be directly related to pruritus and pain, which are both relatively common in these conditions and treatments that reduce them are also successful in mitigating insomnia, while they do not improve OSA or RLS.
Sexual and conjugal dysfunctions were associated with most dermatoses (including mycoses but with the exception of warts) in our study. There have been very few studies exploring the association between sexual health and skin diseases. The largest published study is the European study by ESDaP, which was a study of sexual health using the item 9 of the Dermatology Life Quality Index (DLQI) as a proxy (17). Another recent French study focused on the impact of atopic dermatitis on sexual health (18). In the European study (17), the impact on sexual difficulties was particularly high in patients with hidradenitis suppurativa, prurigo, blistering disorders, psoriasis, urticaria, eczema, infections of the skin and pruritus. In this study, an impact on sexuality was strongly associated with itching, depression, anxiety, and even suicidal ideation. The French study (18) showed that the severity of AD, sites involved, and treatment type negatively impacted the sexual desire of patients and their partners. In addition, involvement of the genital and visible areas was associated with a higher burden and more significant alterations in quality of life.
The main limitation of the current study might be that sampling was based on Internet users, and not on enrolment from more exhaustive sources, such as electoral lists. In addition, as we were not able to find any data on the comparability of Internet users with the general population in France, it is quite plausible that in the older sector of the population, differences may exist between internet users and non-users. It should be noted that some misdiagnoses of skin diseases might have occurred, as we did not perform skin examinations. However, we used validated auto-diagnostic questionnaires, when available, to assess the prevalence of atopic dermatitis, psoriasis, alopecia areata, vitiligo and hidradenitis suppurativa.
Through the frequent feelings of decreased quality of life, as well as being depressed or anxious and the high prevalence of sleep disorders and negative effects on sexual/affective life, the current study confirms a significant psychological impact of the most common skin diseases. Dermatologists should pay more attention to the psychological distress of their patients, which they may underestimate (19).