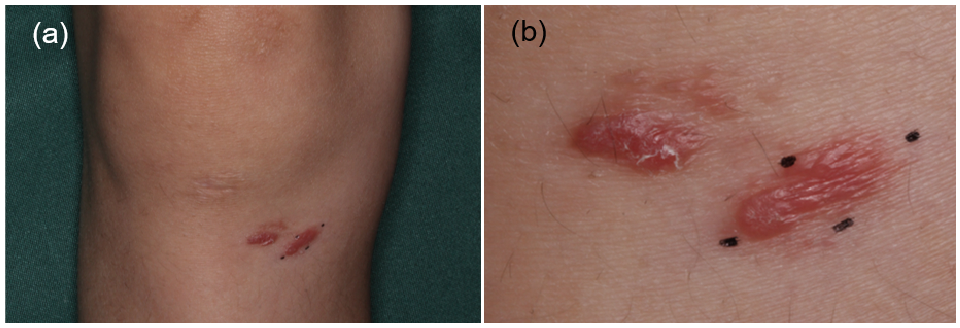
Fig. 1. (a) Nodules on the right knee. (b) Close-up view.
Division of Dermatology, Department of Medicine of Sensory and Motor Organs, Faculty of Medicine, Tottori University, 36-1, Nishi-cho, Yonago, Tottori 683-8504, Japan. E-mail: higoto@tottori-u.ac.jp
A 12-year-old boy was referred to our clinic with nodules on his knee. The nodules had been present for 8 months and there was no improvement with corticosteroid ointment treatment. Physical examination revealed shiny red nodules on his right knee (Fig. 1a, b). The nodules were 10 × 4 mm and 12 × 5 mm in size. There was no palpable lymph node in the inguinal, axillary or cervical region.
What is your diagnosis? See next page for answer.
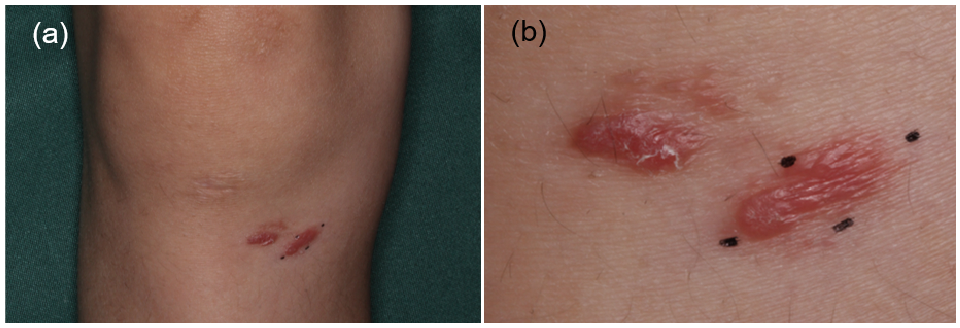
Fig. 1. (a) Nodules on the right knee. (b) Close-up view.
Acta Derm Venereol 2020; 100: adv00231.
Diagnosis: Primary cutaneous marginal zone lym-phoma
The whole lesions were resected and histopathological, immunohistochemical and electron microscopic examinations were performed (Fig. 2a–d). Histopathological examination revealed dense infiltration of plasma cells, lymphoid cells and histiocytes in the dermis (Fig. 2a). Approximately 80% of the infiltrating cells in the specimen were plasma cells. The plasma cells showed mild atypia and a few mitotic figures (Fig. 2b). Immunohistochemically, the atypical plasma cells were positive for CD79a and CD138 and more than 95% of these cells were positive for Igκ (Fig. 2c). Electron microscopy revealed the development of a rough endoplasmic reticulum (rER) in the cytoplasm of plasma cells (Fig. 2d). Some plasma cells appeared normal, but others had an atypical nucleus and dilated rER and large mitochondria. Positron emission tomography-computed tomography did not reveal any other lesions, and the results of bone marrow biopsy were normal. A diagnosis of primary cutaneous marginal zone lymphoma (PCMZL) was made. The patient was followed-up without additional treatment for 9 months, with no sign of recurrence.
PCMZL is defined as a cutaneous B-cell lymphoma, composed of lymphoid cells, plasma cells and histiocytes (1, 2). In the current case, plasma cells accounted for more than 80% of the infiltrating cells. Cases such as the current one used to be diagnosed as primary cutaneous plasmacytoma previously, but such cases have recently been diagnosed as PCMZL (1, 3, 4). This type of lymphoma is more common in adults than in children, and the prognosis is generally favourable (1, 2). The upper arms and trunk are common sites for PCMZL, and lesions on the lower extremities are rare (2, 5). Immunohistochemically, plasma cells showed monotypic expression of immunoglobulin κ chain in the current case, which supports the diagnosis of PCMZL (6). In electron microscopy, immature plasma cells were characteristic of previously reported cases of plasmacytoma (3, 7, 8). Some plasma cells appeared normal in the current case, but other atypical plasma cells had large and developed mitochondria and dilated rER in the cytoplasm. The dilated rER suggests active production of protein, and large mitochondria suggest the necessity of a large amount of energy in the atypical plasma cells. In patients with PCMZL, treatment with resection and/or radiation therapy is common, and chemotherapy including rituximab is also an option (2, 9, 10). Radiation therapy was not given in the current case because of the risk of it causing bone growth disorder, and the patient was followed-up after complete resection. When a nodule is observed in a child, the possibility of lymphoma, including not only T-cell lymphoma, but also B-cell lymphoma, must be considered.
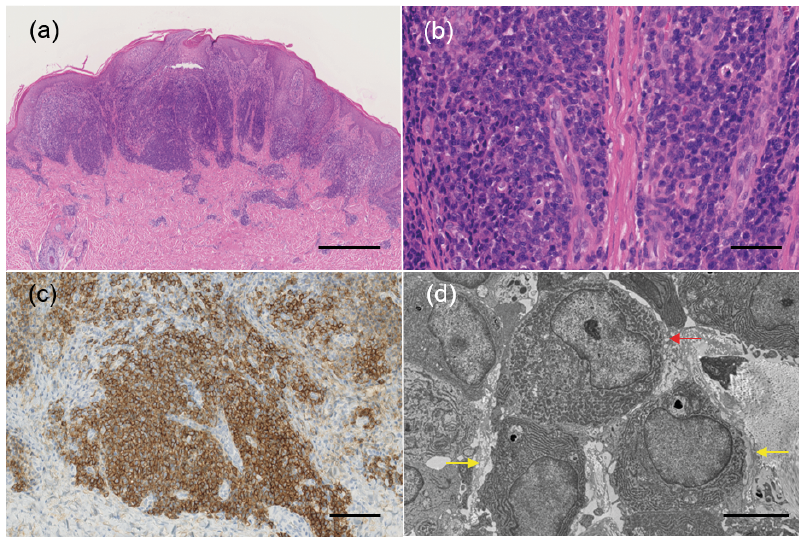
Fig. 2. (a) Histopathological examination revealed dense infiltration of inflammatory cells in the dermis (haematoxylin and eosin (H&E) staining, bar=500 μm). (b) High magnification showed infiltration of plasma cells, lymphoid cells and histiocytes. Plasma cells were predominant with mild atypia and a few mitotic figures (H&E staining, bar=50 μm). (c) Plasma cells were positive for CD138 (CD138 staining, bar=100 μm). (d) Electron microscopy revealed proliferation of plasma cells. Some plasma cells seemed normal (yellow arrows), but others had large and developed mitochondria and dilated rough endoplasmic reticulum (rER) in the cytoplasm with an atypical nucleus (red arrow) (bar=5 μm).