Table I. Characteristics of the patients with chronic pruritus (n = 197)
1Department of Dermatology, University Hospital of Brest and 2University of Brest, Laboratoire Interactions Epitheliums Neurones (LIEN), Brest, France
Chronic pruritus (CP) can occur in the absence of skin diseases, and may be secondary to various causes. The aim of this study was to retrospectively analyse the causes of CP without skin disease in a cohort of patients from the dermatology department, including all patients hospitalized for management of their CP between 2008 and 2018. A total of 197 patients with CP without skin disease were included, mean age 66.7 years, 50.8% men. The main causes identified were psychogenic pruritus (41.1% of patients), neuropathic (36.5%), endocrine (12.2%), haematological (9.6%) and iatrogenic (7.1%) causes. The cause was unknown in 20.8% of patients. Total percent is more than 100 because some patients had several etiologies. Only one aetiology of CP was identified in most patients (69.5%), and 2 aetiologies (in 18.3%) or more (in 12.2%). Concerning symptomatic treatments, emollients were prescribed for 40.6% of patients and topical steroids for 20.3%. Among systemic treatments, gabapentinoids (33%), antidepressants (27.4%) and antihistamines (25.3%) were prescribed. The efficacy of these treatments was rarely complete.
Key words: pruritus; itch; chronic pruritus; psychogenic pruritus; neuropathic pruritus; systemic pruritus.
Accepted Sep 7, 2020; Epub ahead of print Sep 14, 2020
Acta Derm Venereol 2020; 100: adv00274.
doi: 10.2340/00015555-3630
Corr: Emilie Brenaut, Department of Dermatology, University Hospital, FR-29200 Brest, France. E-mail: emilie.brenaut@chu-brest.fr
This study examined the causes of chronic pruritus in the absence of skin diseases. The main causes identified were psychogenic pruritus (41.1% of patients), neuropathic (36.5%), endocrine (12.2%), haematological (9.6%) and iatrogenic (7.1%) causes. Psychological evaluation is useful in these patients. Aetiological and symptomatic treatments were often ineffective; hence there is a need to find new treatments.
According to the International Forum for the Study of Itch (IFSI), chronic pruritus (CP) is defined as the presence of itch for at least 6 weeks (1). CP may occur secondary to a skin disease (e.g. eczema, atopic dermatitis, hives, scabies, or psoriasis), but it can also occur in the absence of skin diseases. The causes of CP in the absence of skin diseases are numerous and include systemic (hepatic, renal, haematological, endocrine, iatrogenic), psychogenic, and neuropathic causes (2–4). Management of CP includes taking a patient history, clinical examination, laboratory tests, and radiological examinations (5). Depending on the suspected aetiology, other tests may be performed (e.g. skin biopsies), to detect a pemphigoid at a pre-bullous stage or a small-fibre neuropathy. Consultation with a psychologist or a psychiatrist is often proposed, as CP can be psychogenic and can have a major impact on quality of life. In the absence of an identified cause, CP is termed “CP of unknown origin”, and the assessment must be repeated (6–11). The aim of the current study was to identify the causes of CP without skin disease in a cohort of patients hospitalized for the check-up of their CP, its characteristics, the results of laboratory and radiological examinations, the evolution of the condition, the treatments prescribed, and their efficacy.
This study was observational, retrospective and monocentric. The patients included in the study were inpatients of the dermatology department of the University Hospital of Brest who underwent a check-up for their CP from January 2008 to December 2018. Patients who met the following criteria were included in the analysis: age 18 years and older; hospitalized for one day or more in the dermatology department; CP in the absence of any skin diseases specific to a pruriginous skin disease; and agreement to participate. Patients with pruriginous skin disease or those who declined to participate were excluded. The identification of patients was made by means of a request to the medical information department of our hospital.
The following information was collected from medical records: demographic data; usual treatments; medical history; characteristics of CP; presence of scratching lesions; results of biological, histological and radiological assessments; and the conclusion of the psychiatric examination. In the follow-up, the treatments received for CP, and its evolution were recorded.
The main objective of this study was to analyse the identified cause(s) of the CP. The secondary objectives were to analyse the characteristics of the pruritus, the results of laboratory and radiological examinations, the evolution, treatments, and the efficacy of treatment (complete, partial, no efficacy). After checking the inclusion and exclusion criteria, an information letter with an opposition form was sent to patients. Non-response after 15 days confirmed their agreement to participate, and data were collected. The study protocol was approved by the Jurisdictional Ethics Committee of Brest, France (ID: 29BRC18.0247).
Quantitative data were described by their mean, standard deviation (SD), median, extreme values and the number of missing data. Qualitative data were described as percentages.
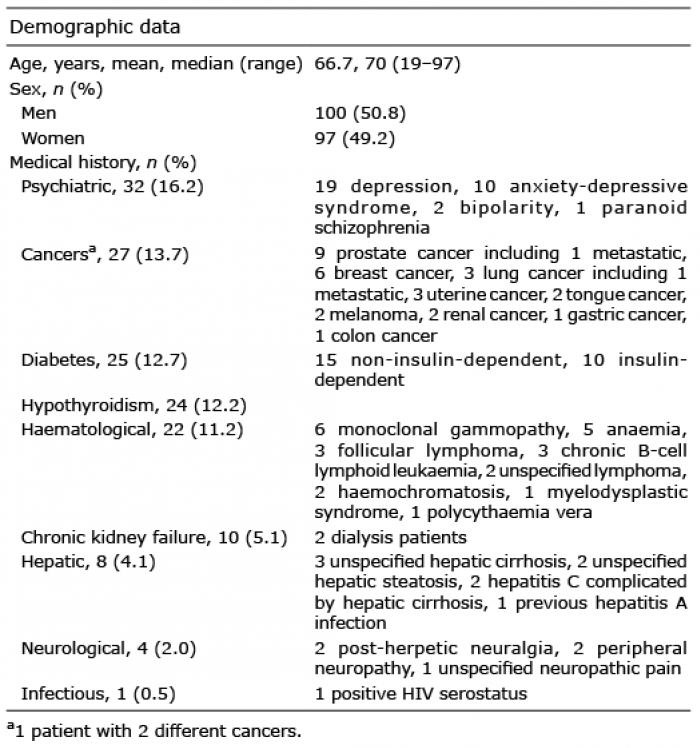
Demographic characteristics of the population and medical history
A total of 197 patients were included. Four patients declined to participate. The demographic characteristics and medical history of the patients are shown in Table I. Concerning the usual treatment, the mean number of medications was 4.2 ± 3.4 per patient (from 0 to 14). Among drugs that were potential inducers of pruritus, 14.3% of patients were treated with an enzyme converting enzyme inhibitor, 16.8% a sartan, 17.9% a calcium channel blocker, 24.5% a statin, 6.1% oral anti-diabetic drugs, 2.6% amiodarone, 0.5% chloroquine, 5.6% opioids, and 3.1% tramadol. Proton pump inhibitors were used in the usual treatment of 24.5% and L-thyroxin in 12.2% of patients.
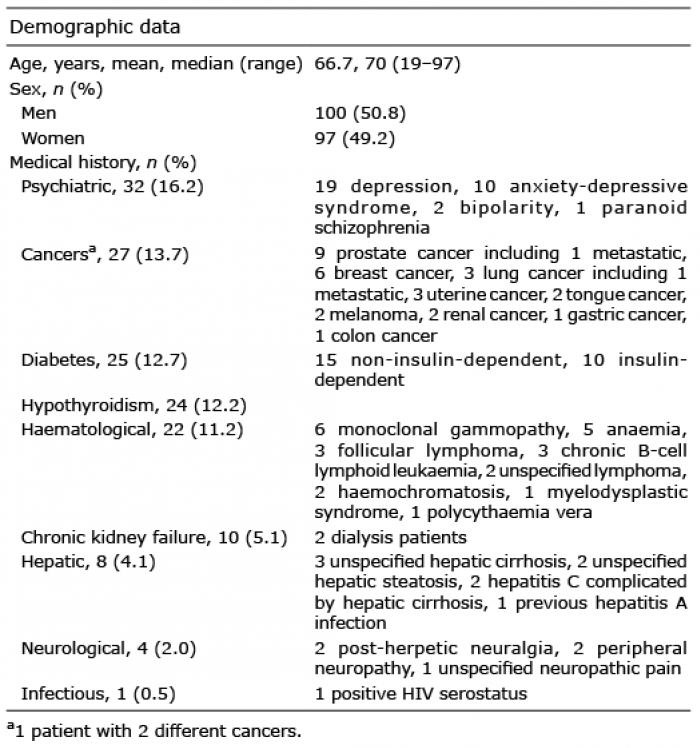
Table I. Characteristics of the patients with chronic pruritus (n = 197)
Characteristics of pruritus
Pruritus was present for more than 10 years for 20.8% of patients, for 5–10 years for 17.8%, for 1–5 years for 36.0% and for less than one year for 25.4% of patients. Pruritus was predominantly diurnal for 99.0% of patients, but 84.2% of patients had nocturnal pruritus. Twenty percent of patients had aquagenic pruritus, and 87.8% of patients had intermittent pruritus. Scratching lesions were present in 65.5% of patients: 62.8% of whom presented with excoriations, 8.5% lichenification and 51.2% prurigo lesions. The presence of scratching lesions, according to the aetiology of CP, is shown in Fig. 1.
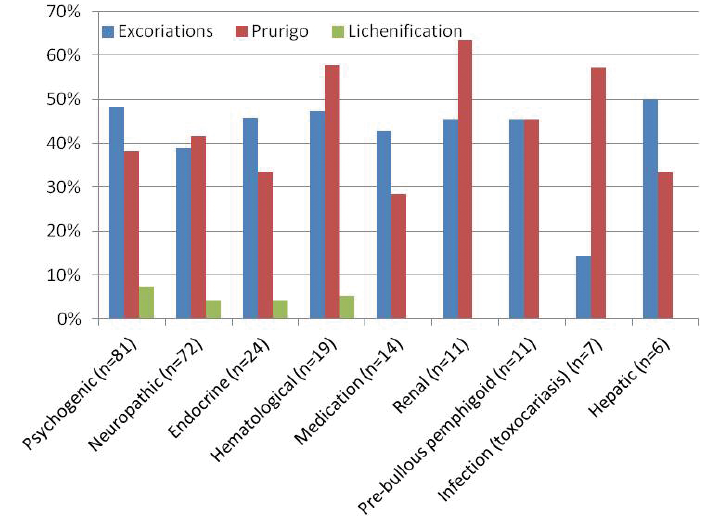
Fig. 1. Scratching lesions according to the aetiology of pruritus.
Biological, histological and imaging data
Biological and histological data are shown in Table II. Concerning the 23 patients with a monoclonal gammopathy, 8 presented with a kappa IgM peak, 5 an IgM lambda, 5 IgG kappa, 3 an IgG lambda, 1 an IgA kappa and 1 an IgA lambda peak. When performed, 23.2% (13/56) of toxocariasis serologies were positive (Western blot), and 6.5% (2/31) of parasitological examinations of stools were positive (1 for Endolimax nana and 1 for Blastocystis hominis).
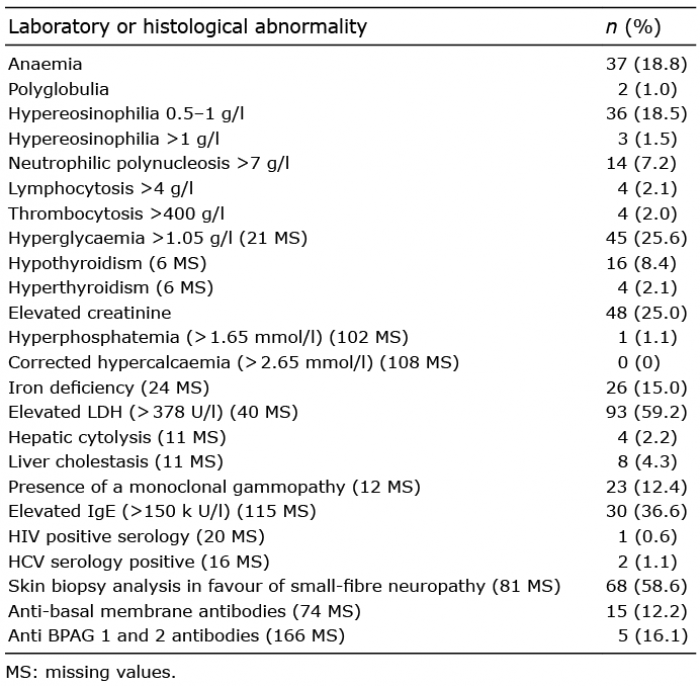
Table II. Biological and histological data
On chest X-ray, 11/138 (8.0%) patients had vertebral osteoarthritis, 7/138 (5.1%) had non-calcified alveolar opacities and 6/138 (4.3%) had adenopathies. On abdominal ultrasonography, 17/123 (13.8%) patients had hepatic steatosis, 10/123 (8.1%) patients had hepato-megaly, and 4/123 (3.3%) patients had steatosis and hepatomegaly. An atypical lesion associated with hepatic hilar polyadenopathies was found in one patient. On thoraco-abdomino-pelvic computed tomography (CT) scans, 3/54 (5.6%) patients had neoplasias (2 lung cancers and 1 colon cancer), 4/54 (7.4%) had degenerative spines, 1/54 (1.9%) had chronic hepatopathy and 2/54 (3.7%) had hepatomegaly. A case of lymphoma recurrence was revealed by positron emission tomography (PET). On spinal magnetic resonance imaging (MRI), 4/18 (22.2%) patients presented degenerative spine alone, 3/18 (16.7%) stenosis alone and 2/18 (11.1%) degenerative spine and stenosis.
Psychiatric consultation
Only 117/197 (59.4%) patients received a psychiatric consultation. The distribution of the main established diagnoses after this consultation is shown in Fig. 2. Some patients had 2 diagnoses (e.g. psychogenic pruritus and depression), and depression was diagnosed in 12 patients (10.3%), anxiety in 11 (9.4%) and anxio-depressive syndrome in 2 (1.7%). In 10 patients, the diagnosis of psychogenic pruritus was made before psychiatric consultation, and the patients declined the consultation.
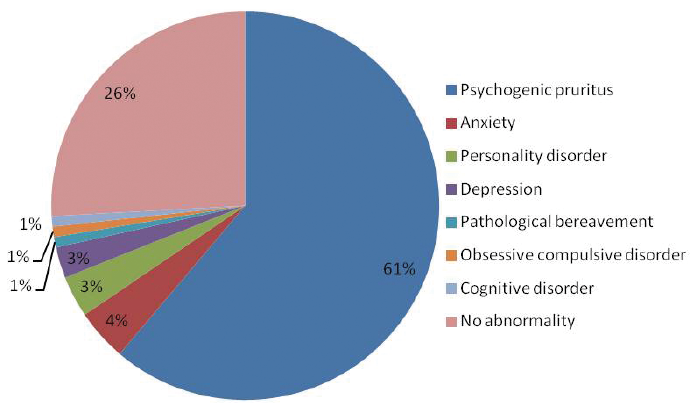
Fig. 2. Diagnosis after the psychiatric consultation (n = 117).
Causes of chronic pruritus
The causes of CP identified after the assessment are shown in Table III. Most patients (69.5%) had one aetiology, 18.3% had 2 aetiologies, and 12.2% had 3 or more aetiologies.
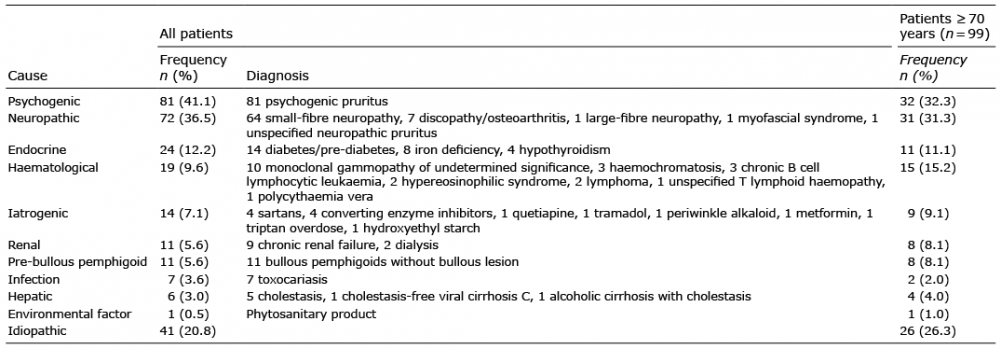
Table III. Causes of chronic pruritus
Treatments received for pruritus and efficacy
Concerning the aetiological treatments, 11 patients were treated for toxocariasis (10 with albendazole and 1 with ivermectin), with complete efficacy for one patient, partial for 4 and inefficacy for 2 (no data for the 4 other patients). Five patients received iron supplementation, with no effect on the pruritus. Many medications were stopped because they were considered to be potential inducers of pruritus: converting enzyme inhibitor therapy (5 patients), sartans (5), calcium channel blockers (1), statins (1), allopurinol (1), triptan (1) and tramadol (1). Of these 15 patients, only the cessation of sartans resulted in improved pruritus.
Patients received 1.7 ± 1.6 (mean ± SD) (range 0–10) treatments for their pruritus. Treatments and their efficacy are presented in Table IV. The treatment for each patient was adapted to the cause, for example patients with neuropathic pruritus were often treated with gabapentinoids, patients with psychogenic pruritus were treated with anxiolytics, antidepressants or psychological/psychiatric care. Ten patients (5.1%) were lost to follow-up without treatment, 8 patients (4.1%) were untreated, and 8 patients (4.1%) had spontaneous remission. Five patients received antipsychotic drugs (risperidone), 1 for delusional infestation and 4 for psychogenic pruritus, with a partial efficacy for 1, inefficacity for 1, and no data for the 3 others.
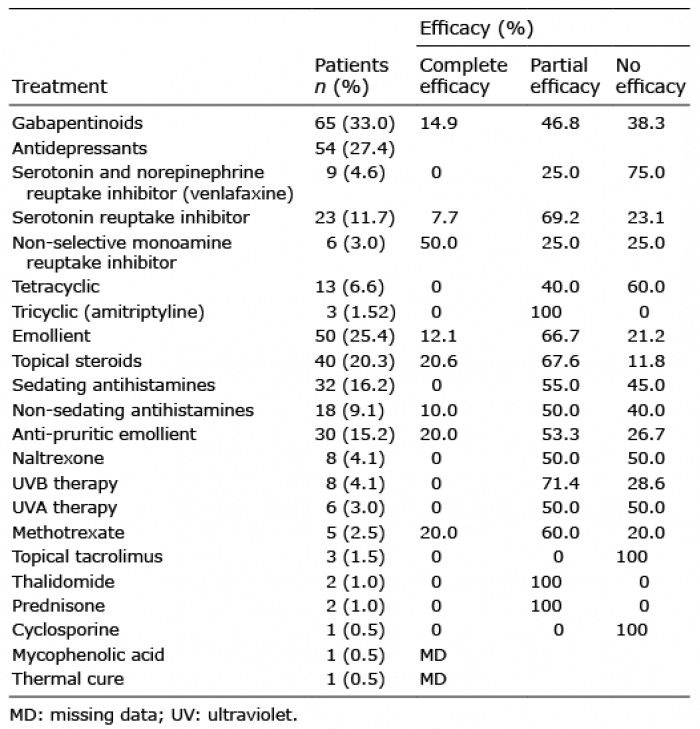
Table IV. Efficacy of treatments on pruritus
Evolution at the date of the last follow-up
At the time of the final follow-up, 27.9% of patients had improved, 51.3% had persistent pruritus, 17.8% were lost to follow-up, and 3.0% were followed up by another dermatologist. The duration of patient follow-up ranged from 6 days to more than 7 years (mean 10.6 months).
In our cohort of patients, the main causes of CP were psychogenic pruritus (41.1%) and neuropathic pruritus (36.5%). The high frequency of psychogenic origin demonstrates the importance of a consultation with a psychiatrist for these patients. Anxiety was diagnosed in 10.3% of patients and depression in 9.4% (2 patients had anxio-depressive syndrome). In a European study including 27 patients with prurigo, 37% had anxiety and 29% had depression, according to the Hospital Anxiety and Depression Scale (HADS) (12). In the current study, 40.6% of patients did not receive a psychiatric consultation; therefore, anxiety and depression could be underdiag-nosed. It should be useful to apply the HADS questionnaire to all patients with CP in order to screen for anxiety and depression and to undertake a specialized consultation. In the current study, the diagnosis of psychogenic pruritus was made according to defined criteria, with the presence of 3 mandatory and at least 3 optional criteria (13). The high frequency of psychogenic pruritus in this study can be explained by a recruitment bias because our centre is recognized to treat this type of pruritus (14).
Concerning neuropathic pruritus, the main aetiology was small-fibre neuropathy (SFN). SFN has received increasing attention in the last 20 years, especially with the introduction of intraepidermal nerve fibre density measurements (15). Patients with SFN present with autonomic symptoms and mainly sensory symptoms, such as pain, pruritus, burning, tingling or numbness. Sometimes, pruritus is the main complaint symptom of these patients; therefore, staged skin biopsies are useful to examine for this disease (16). Recently, Pereira et al. (17) proposed characteristics of a neuropathic origin: the beginning of the itch on normal skin, an association with additional painful symptoms, alleviation with cold/ice application and itch occurring in attacks. We also proposed the Neuropathic Pruritus 5 (NP5) for the diagnosis of neuropathic pruritus (18).
Few studies have investigated the frequency of causes of CP. Weisshaar et al. (19) investigated 132 patients with pruritus via a questionnaire. Of these patients, 57% had pruritus due to dermatoses, 36% due to systemic disease, and 8% of unknown origin. The quality of life was impaired in both populations (19). In a retrospective study, Wallengren et al. (20) included 139 patients with CP, of whom 17.2% presented a neuropathic pruritus, 22% a psychiatric disease, and 26.6% a pruritus of unknown origin. The most severe and long-lasting itch was found in patients with multiple systemic diseases and in those with pruritus of unknown origin (20). In a study including 49 patients with generalized pruritus in the absence of skin diseases, the main aetiologies were endocrine diseases (33%), haematological and lympho-proliferative diseases (14.6%), and 37.5% an unknown origin (6–8, 21).
The patients in the current study had many usual treatments that could potentially induce pruritus, and numerous comorbidities (e.g. 12.7% had diabetes and 12.2% had hypothyroidism). There were many abnormalities in their biological results that could explain the pruritus (e.g. 15% of patients with martial deficiency, 12.4% monoclonal peak). CP can be multifactorial, and the primary cause can be difficult to identify. Concerning treatments, 24.5% of our patients were treated with proton pump inhibitors and 12.2% with L-thyroxine. This rate is the same as the use of these treatments in the French population; thus, there is no evidence to indicate that they are potential inducers of pruritus. The cessation of treatments that were potential inducers of pruritus had little effect on the evolution of CP in our cohort.
Senile pruritus is defined as idiopathic pruritus in a patient older than 70 years of age. In our study, pruritus was idiopathic in only 26% of the 99 patients aged 70 or more. This population often had few comorbidities and took few medications; therefore, the term senile pruritus can be used only after the check-up. The question remains as to the relevance of the term “senile pruritus”. If senile pruritus exists, one of the physiopathological hypotheses could be deafferentation (22).
Interestingly, scratching lesions were particularly frequent in renal and haematological pruritus.
Hypereosinophilia was frequent (occurring in 20% of patients in the current study), and the level of eosinophils could orient the type of treatment for some authors (10). If presence of blood or tissue eosinophilia, some authors propose to start immunomodulator therapy and if not, to start gabapentinoids (23). The search for toxocariasis was sometimes realized, but its place in the assessment of pruritus assessment remains to be confirmed. CP may be a cutaneous manifestation of toxocariasis, but no significant relationship has been found (5, 7, 24). Among the serologies performed, 23.2% were positive, and the treatment of toxocariasis was never accompanied by complete regression of the pruritus.
Study limitations
Among the limitations of this study, the fact that it is mono-centric may be result in recruitment bias, which could explain an over-represented number of patients with neuropathic and psychogenic pruritus (14, 25). Some aetiologies could be under-represented (e.g. hepatic or renal pruritus) because these patients may have been treated by specialists. Because the current study is retrospective, complete data were not available; in particular, quality of life was not studied. Patients were recruited if the check-up was performed during hospitalization for one day or more, but outpatients were not recruited. The population affected by CP is heterogeneous, as highlighted in this study; therefore, research on the pathophysiology and development of treatments is difficult.
Future research
Chronic prurigo, a model of CP, has been well defined recently, and treatments are in development for this disease (26, 27). Different randomized controlled trials are recruiting patients, and new molecules are promising, including monoclonal antibodies, NK1R antagonists, and opioid receptor agonists/antagonists.
Conclusion
The main causes of CP in the current cohort of patients were psychogenic and neuropathic pruritus. Almost one-third of patients had 2 causes or more of their CP. Aetiological treatment was often ineffective, and symptomatic treatments had moderate efficacy; thus, there is a need to find new treatments for CP.