
Table I. Patients’ characteristics at baseline
1Department of Dermatology and Allergy, Herlev and Gentofte Hospital, University of Copenhagen, DK-2900 Hellerup, and 2Copenhagen Research Group for Inflammatory Skin, Herlev and Gentofte Hospital, Hellerup, Denmark. E-mail: christopher.willy.schwarz.01@regionh.dk
Accepted Aug 21, 2020; Epub ahead of print Aug 26
Acta Derm Venereol 2020; 100: adv00265.
doi: 10.2340/00015555-3620
Psoriasis is associated with metabolic syndrome, including diabetes mellitus (1). The association between psoriasis and hyperglycaemia is not understood (2). However, systemic inflammation in psoriasis, driven by T helper cells type 17 (Th17 cells) and production of interleukin (IL)-17A (3), has been suggested to play a role. An experimental study has reported that Th17 promotion, IL-1β, and IL-6 secretion results in an inflammatory environment that inhibited insulin response in specific cells (4), which suggests a possible role for IL-17A in insulin resistance.
A recent study by Ikumi et al. (5) identified a significant positive correlation between Psoriasis Area and Severity Index (PASI) and haemoglobin A1c (HbA1c) level in 39 patients with psoriasis. In addition, they found that treatment of psoriasis with anti-IL-17A (secukinumab and ixekizumab) lowered HbA1c after 4 months of treatment in a subgroup of 14 patients.
Using a larger sample size, the current study aimed to assess the potential correlation between PASI and HbA1c, and to investigate the antidiabetic role of anti-IL-17A and, in comparison, anti-IL-12/-23.
All patients with psoriasis treated with anti-IL-17A (secukinumab) or anti-IL-12/-23 (ustekinumab) from June 2016 through November 2019 in the Department of Dermatology and Allergy, Herlev and Gentofte Hospital, Denmark, were included in the study. Only biologic-naïve patients were included, and patients were excluded if no baseline PASI and no measures of HbA1c before (maximum 90 days) and after at least 120 days of treatment were available.
Spearman’s rank correlation coefficient was used to assess the relationship between baseline PASI and HbA1c levels. To compare changes in HbA1c, Wilcoxon signed-rank test was used, as the data were not normally distributed.
A total of 75 biologic-naïve patients were identified. Of these, 3 patients received antidiabetic treatment and were excluded from the calculations, resulting in a final total of 72 included patients (Table I).

Table I. Patients’ characteristics at baseline
No significant correlation was found between baseline PASI and HbA1c levels (Spearman’s ρ = –0.05, p = 0.69). When pooling both treatments, no significant change was found in HbA1c after the start of biologic treatment (Fig. 1). Analysing the 2 biologics separately did not alter the results (Table II).
Since HbA1c is in the normal range, the patients in the current study are generally not candidates for antidiabetic treatment. A sensitivity analysis of patients with HbA1c ≥ 37 mmol/mol (n = 19, the 3 patients receiving antidiabetic treatment included) also showed no association (p = 0.22). This indicates that treatment with secukinumab or ustekinumab does not lower HbA1c in a population of patients in whom antidiabetic measures might be relevant.

Fig. 1. Haemoglobin A1c (HbA1c) before and after at least 120 days of treatment with secukinumab or ustekinumab.
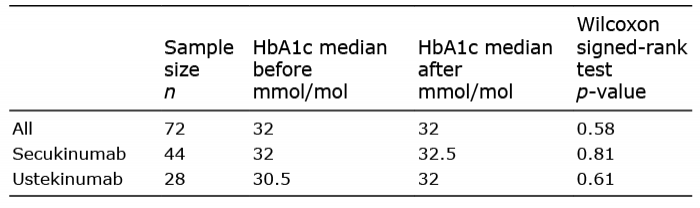
Table II. Comparison of haemoglobin A1c (HbA1c) before and after at least 120 days of treatment with secukinumab or ustekinumab
In contrast to the study by Ikumi et al. (5), the results of the current analysis revealed no association between psoriasis severity and HbA1c and no association between anti-IL-17A or anti-IL-12/-23 treatment and reduction of HbA1c. The patients were comparable in terms of body mass index to the study population provided by Ikumi et al. (5) (Table I). However, different characteristics of the 2 study populations could impact on the results. In the analysis of anti-IL-17A and HbA1c by Ikumi et al. (5), 3 of the 14 patients received antidiabetic treatment, while, in the main analysis, the current study excluded patients receiving antidiabetic treatment. A sensitivity analysis, which included only patients with higher HbA1c and the 3 patients who received antidiabetic treatment, supports this finding. It is important to note the observational character of both studies and the lack of control groups. Based on a power calculation (β = 0.80, α = 0.05) for a paired t-test, and with an effect size based on data from Fig. 1c in the study by Ikumi et al. (5), a sample size of n = 21 was required to confirm the association between anti-IL-17A or anti-IL-12/-23 and reduction in HbA1c (6). The Wilcoxon signed-rank test is the non-parametric version of the paired t-test and usually has less statistical power. Even so, the current sample size should be sufficient to confirm the previous findings.
These findings are supported by the results of a post-hoc analysis of 3,010 patients with psoriasis, which investigated the effects of secukinumab, etanercept, and placebo on metabolic parameters, in which no effect of secukinumab on fasting plasma glucose was found (7). Supported by an experimental study, in which blocking IL-17A with secukinumab did not restore insulin sensi-tivity (8), all indicating that IL-17A does not play a major role in type 2 diabetes through inflammation-mediated insulin resistance.
In conclusion, this study found no correlation between PASI and HbA1c levels and no evidence for an overall change in HbA1c related to treatment with secukinumab or ustekinumab.
Conflicts of interest: CWS have no conflicts of interest to declare. NDL has been a paid speaker for Eli Lilly and Janssen-Cilag. CZ has been a paid speaker for Pfizer, Eli Lilly, Novartis, LEO Pharma, and CSL and has been a consultant or has served on advisory boards with Eli Lilly, Janssen-Cilag, Novartis, AbbVie, Takeda, Amgen, Almirall, and CSL. CZ has served as an investigator for Janssen-Cilag, AstraZeneca, Pfizer, Eli Lilly, Takeda, Regeneron, Amgen, MSD, LEO Pharma, AbbVie, Novartis, Boehringer Ingelheim, Sanofi, and CSL. LS has been a paid speaker for AbbVie, Sanofi, Eli Lilly, Novartis, and LEO Pharma and has been a consultant or has served on advisory boards with AbbVie, Janssen-Cilag, Novartis, Eli Lilly, LEO Pharma, UCB, Almirall, and Sanofi. She has served as an investigator for Takeda, Regeneron, Amgen, MSD, CSL, AbbVie, Janssen-Cilag, Boehringer Ingelheim, AstraZeneca, Eli Lilly, Novartis, Sanofi, Pfizer, and LEO Pharma and has received research and educational grants from AbbVie, Novartis, Sanofi, Janssen-Cilag, and LEO Pharma.