SHORT COMMUNICATION
Minocycline-induced Hyperpigmentation Confined to Lupus Miliaris Disseminatus Faciei
Masakazu KAKURAI, Rie HONDA*, Hanako MIYAHARA and Shusaku ITO
Division of Dermatology, Hitachi General Hospital, Hitachi General Hospital, 2-1-1 Jonan, Hitachi, Ibaraki 317-0077, Japan. *E-mail: rie.honda.ss@hitachi.com
Citation: Acta Derm Venereol 2023; 103: adv18462. DOI: https://doi.org/10.2340/actadv.v103.18462.
Copyright: © Published by Medical Journals Sweden, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: Oct 30, 2023; Published: Dec 7, 2023
Competing interests and funding: The authors have no conflicts of interest to declare.
INTRODUCTION
Lupus miliaris disseminatus faciei (LMDF) is an idiopathic granulomatous inflammatory dermatosis characterized by red-to-yellow facial papules, which is treated with oral therapy including minocycline (1). Minocycline-induced hyperpigmentation confined to areas of inflammation or scars has been reported in patients with acne (2–5), but not in patients with LMDF. We report here a case of minocycline-induced hyperpigmentation confined to facial inflammatory lesions in a patient with LMDF.
CASE REPORT
A 75-year-old Japanese woman was referred to our hospital with a 4-month history of facial papules and gradual hyperpigmentation of facial skin. The facial papules had first developed 3 years earlier and were suspected to be LMDF by skin biopsy. At that time the symptoms had responded well to oral minocycline, 100 mg/day, for 2 months, but the LMDF lesions recurred after its cessation. Therefore, oral minocycline had been continued to prevent exacerbation of the lesions, which did not occur during a total of 29 months of treatment. The facial papules recurred 4 months prior to presentation, and hyperpigmentation gradually developed within papules with the continuation of minocycline. Discontinuation of the oral minocycline was not possible because the patient was more concerned about further exacerbation of LMDF lesions than hyperpigmentation and the patient strongly requested continuing the oral minocycline. She also took eldecalcitol for osteoporosis. Physical examination revealed blue-black macules confined to facial papules (Fig. 1a–c). Dermoscopy revealed blue-black and brown macules within papules conforming to the outline of pits (Fig. 1d). Hyperpigmentation was absent on other skin areas, the oral mucosa, teeth, sclera and nails. Five-millimetre punch biopsies of a skin-coloured papule and hyperpigmented papule on the face (Fig. 2a) revealed that the former had central areas of necrosis surrounded by epithelioid cell granuloma, histiocytes and lymphocytes with a multinucleated giant cell in the dermis (Fig. 2b,c), whereas the latter showed pigment granules in the dermis (Fig. 2b). Staining with Masson-Fontana for melanin, Prussian blue for iron and von Kossa for calcium was positive in extra- and intra-cellular macrophages in the upper dermis (Fig. 2d–f), but negative in the skin-coloured papule. Ziehl-Neelsen and periodic acid–Schiff staining were negative. Laboratory test results, including a complete blood cell count, metabolic panel and T-SPOT, and a computed tomography of the chest, were normal. Taken together, LMDF and minocycline-induced hyperpigmentation were diagnosed. After cessation of minocycline treatment at the first visit, topical tacrolimus and oral roxithromycin were administered, and the hyperpigmented lesions attenuated slightly within 2 months.
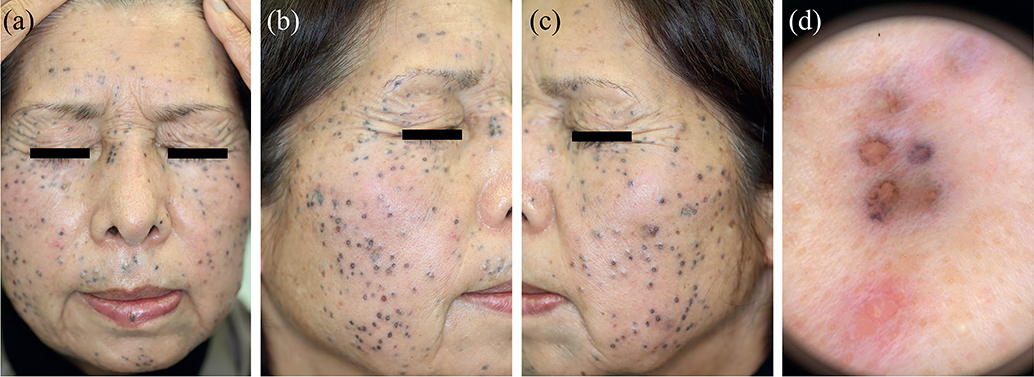
Fig. 1. Clinical findings. (a–c) Clinical images of blue-black macules confined to multiple papules up to 3 mm in diameter on the face. (d) Dermoscopy from the lower jaw revealed blue-black and brown macules in areas of papules conforming to the outline of pits, and a pink-coloured papule (X10). Permission from the patient is given to publish these photos.
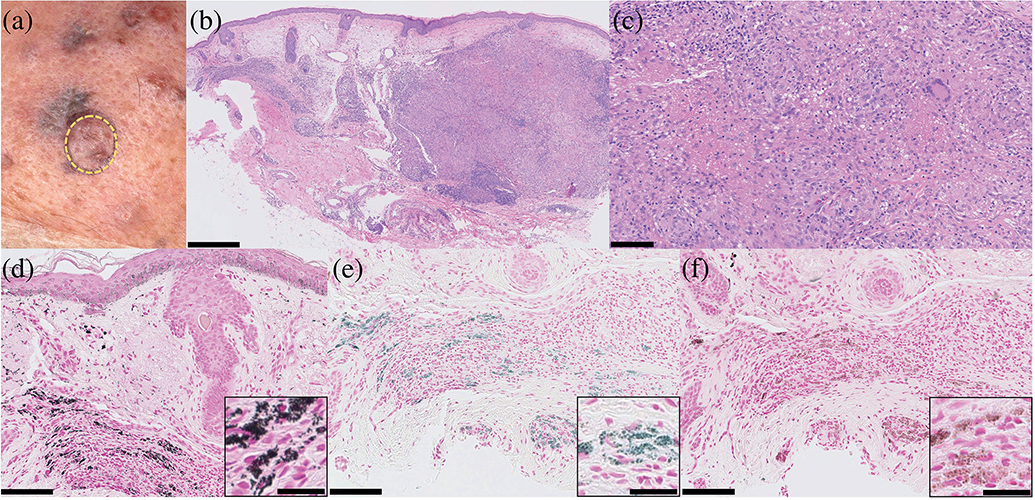
Fig. 2. Clinical and histological findings. (a) Five-millimetre punch biopsy of a skin-coloured papule and hyperpigmented papule from the right lower jaw: yellow circle. (b, c) A haematoxylin-eosin-stained slide of the skin-coloured papule revealed central areas of necrosis surrounded by epithelioid cell granuloma, histiocytes and lymphocytes with a multinucleated giant cell in the dermis, (b) and the hyperpigmented papule showed pigment granules in the dermis (bar=500 and 100 μm, respectively). (d–f) Histochemical staining with: (d) Masson-Fontana for melanin; (e) Prussian blue for iron; and (f) von Kossa for calcium was positive in extra- and intra-cellular macrophages in the upper dermis. (Bars in large images=100 μm; inset, bars=25 μm).
DISCUSSION
Oral minocycline is widely used for dermatoses, including LMDF, acne and rosacea (1–5). Minocycline-induced hyperpigmentation occurs in 3–15% of patients, particularly with prolonged use (5). Minocycline-induced hyperpigmentation confined to areas of inflammation or scars has been reported in patients with acne (2–5). We report here a case of hyperpigmentation confined to facial inflammatory lesions in a patient with LMDF who was receiving minocycline. To the best of our knowledge, there is no previous report of minocycline-induced hyperpigmentation in a patient with LMDF.
Minocycline-induced hyperpigmentation is categorized into 3 types based on clinicopathological features (3–5). Type I is characterized by blue-black macules in areas of inflammation or scars on the face, resulting from iron-containing pigment granules in the dermis (3–5). Type II presents as blue-grey macules or diffuse hyperpigmentation occurring on extremities, due to iron- or melanin-containing pigment granules in the dermis (4, 5). Type III presents as a diffuse muddy-brown hyperpigmentation in sun-exposed areas, due to increased melanin deposition in the basal layers (4, 5). Moreover, a variant of Type I, characterized by blue-grey macules confined to acne scars on the back with melanin and calcium deposition in the dermis, has been described as a fourth type of minocycline-induced hyperpigmentation (4). In the current case, facial hyperpigmentation was clinically regarded as type I. However, the histological features of hyperpigmentation included melanin-, iron- and calcium-containing pigment granules in the dermis, which were not seen in the histological findings of the 3 distinct types of minocycline-induced hyperpigmentation.
Although the pathogenesis of minocycline-induced hyperpigmentation remains unknown (2–5), a proposed mechanism involves the contribution of iron chelates of minocycline in the dermis (6). The causal link between minocycline and hyperpigmentation confined to LMDF lesions is unclear, but clinicopathological features of hyperpigmentation in the current case are highly notable. Clinicians should be aware of the features of minocycline-induced hyperpigmentation and the need for rapid cessation of minocycline when hyperpigmented lesions develop.
REFERENCES
- Al-Mutairi N. Nosology and therapeutic options for lupus miliaris disseminatus faciei. J Dermatol 2011; 38: 864–873.
- Basler RS, Kohnen PW. Localized hemosiderosis as a sequela of acne. Arch Dermatol 1978; 114: 1695–1697.
- Fenske NA, Millns JL, Greer KE. Minocycline-induced pigmentation at sites of cutaneous inflammation. JAMA 1980; 244: 1103–1106.
- Mouton RW, Jordaan HF, Schneider JW. A new type of minocycline-induced cutaneous hyperpigmentation. Clin Exp Dermatol 2004; 29: 8–14.
- Eisen D, Hakim MD. Minocycline-induced pigmentation. Incidence, prevention and management. Drug Saf 1998; 18: 431–440.
- Gordon G, Sparano BM, Iatropoulos MJ. Hyperpigmentation of the skin associated with minocycline therapy. Arch Dermatol 1985; 121: 618–623.