SHORT COMMUNICATION
Drug-induced Granulomatous Panniculitis: Polarization of M1/M2 Macrophages
Naomi TANI, Nanako YAMADA and Yuichi YOSHIDA
Division of Dermatology, Department of Medicine of Sensory and Motor Organs, Faculty of Medicine, Tottori University, 86 Nishi-cho, Yonago, Tottori 683-8504, Japan. E-mail: taninaomi@tottori-u.ac.jp
Citation: Acta Derm Venereol 2023; 103: adv18855. DOI: https://doi.org/10.2340/actadv.v103.18855.
Copyright: © Published by Medical Journals Sweden, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: Nov 17, 2023; Published: Dec 20, 2023
INTRODUCTION
Granulomatous drug eruptions are rare entities of non-infectious granulomatous disease of the skin, which predominantly consist of histiocytes in the inflammatory infiltrate (1, 2). Here we report 2 cases of drug-induced granulomatous panniculitis with immunohistochemical findings.
CASE REPORTS
Case 1. A 72-year-old woman was referred to us with a 3-week history of redness and swelling of both lower legs and a 1-week history of red macules on both forearms. The patient had a past medical history of mitral valve and aortic valve replacement for infective endocarditis, hypertension, paroxysmal atrial fibrillation, type 2 diabetes mellitus, dyslipidaemia, hyperuricaemia and right internal carotid artery stenosis. The patient had been treated with azosemide for 4 years. Physical examination revealed erythema from both of the upper limbs to the hands (Fig. 1a) and extensive subcutaneous induration on both legs (Fig. 1b). Histopathology of a biopsied specimen taken from the left forearm showed granulomas in the superficial layer of the subcutaneous adipose tissue (Fig. 1c). Miescher’s radiating granulomas were also seen (Fig. 1d). Inflammatory infiltrates including histiocytes, lymphocytes and sparse eosinophils were seen around the granuloma. Histopathology of induration on the right lower leg showed granulomas from the deep dermis to the adipose tissue (Fig. 1e). Fibrosis of the septum area in the fat tissue and granuloma with inflammatory infiltrate were observed in a fat lobule. Inflammatory infiltrates were histiocytes, lymphocytes and sparse eosinophils. Both specimens were negative for Gram stain, periodic acid-Schiff stain and acid-fast bacillus stain. In immunohistochemical staining of the left forearm, there were many CD68-positive cells in epithelioid granulomas and interstitial area (Fig. 2a). CD11c (M1 macrophages)-positive cells were seen in epithelioid granulomas and partially in the interstitial area (Fig. 2b). In contrast, CD163 or MS4A4A (M2 macrophages)-positive cells were diffusely recognized in the interstitial area and scattered in the periphery of the epithelioid granuloma (Fig. 2c, d). Serum levels of angiotensin-converting enzyme (ACE) and soluble interleukin-2 receptor (sIL2R) were within normal ranges. There were no special findings on a chest X-ray. Based on these findings, we suspected sulphonamide diuretic-induced granulomatous panniculitis (3), and treatment with azosemide was discontinued. The swelling and induration in the extremities were improved within 4 weeks. Therefore, we made a diagnosis of granulomatous panniculitis due to azosemide.
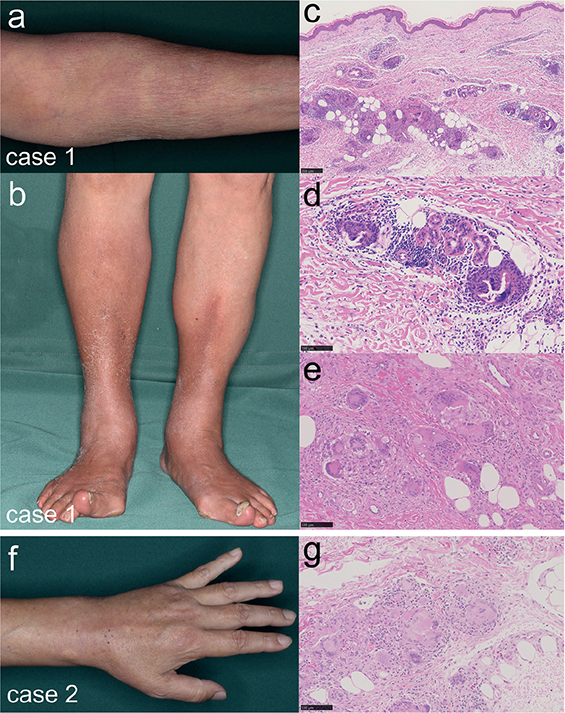
Fig. 1. Clinical and histological findings. (a, b) Clinical manifestation at the first visit of case 1. (a) Erythema on the upper limb. (b) Subcutaneous induration on both legs. (c–e) Histopathological findings of case 1. (c) Granulomas in the superficial layer of the subcutaneous adipose tissue (haematoxylin and eosin (H&E) staining, bar = 250 μm). (d) Miescher’s radiating granulomas (H&E staining, bar = 100 μm). (e) Granulomas from the deep dermis to the adipose tissue (H&E staining, bar = 100 μm). (f) Clinical manifestation at the first visit of case 2. Swelling from the periphery of the forearm to the back of the hand. (g) Histopathological findings of case 2. Granulomatous small nodule in the deep dermis to the adipose tissue containing multinucleated giant cells (H&E staining, bar = 100 μm).
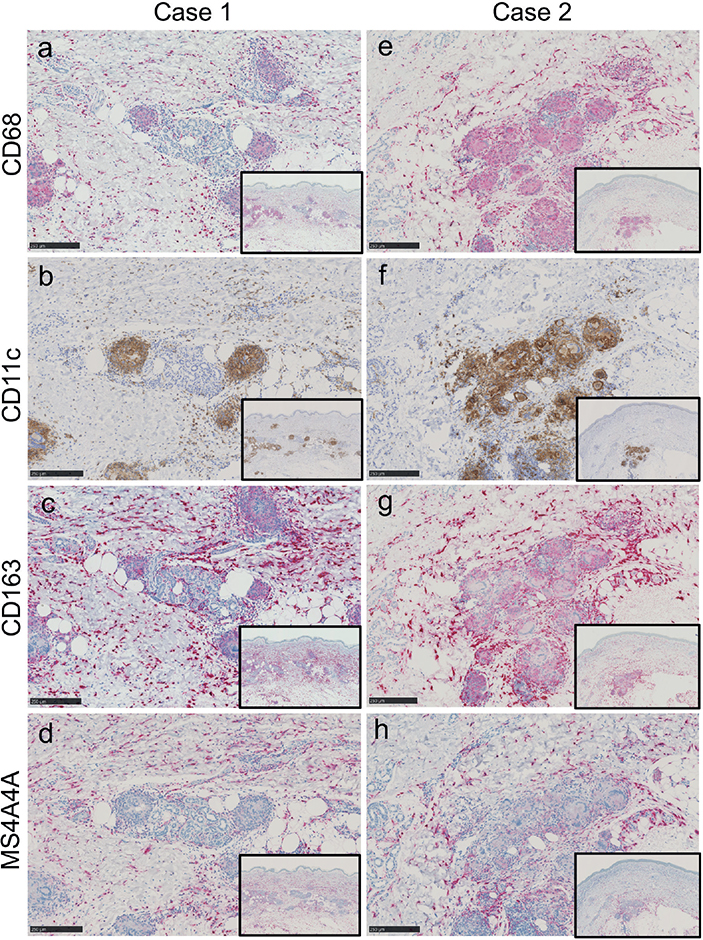
Fig. 2. Immunohistochemical findings of (a–d) case 1 and (e–h) case 2. Immunohistochemical staining of: (a, e) CD68, (b, f) CD11c, (c, g) CD163 and (d, h) MS4A4A (bar=250 μm).
Case 2. A 65-year-old man was referred to us with a 2-week history of swelling and pain in the limbs. The patient had a past medical history of hypertension and percutaneous coronary intervention for angina pectoris. The patient had been treated with irbesartan, nifedipine and trichlormethiazide for 10 years, and with aspirin, clopidogrel sulphate, rosuvastatin calcium and ethyl icosapentate for 3 years. Physical examination revealed swelling in the extremities (Fig. 1f). Histopathology of a biopsied specimen taken from the dorsal aspect of the left hand showed granulomatous nodules in the deep dermis to the adipose tissue with multinucleated giant cells (Fig. 1g). Inflammatory infiltrates including histiocytes, lymphocytes and a few eosinophils were seen around the granuloma. Immunohistochemically, CD68-positive cells were observed in epithelioid granulomas and interstitial area (Fig. 2e). CD11c-positive cells were seen in epithelioid granulomas and partially in the interstitial area (Fig. 2f). CD163 or MS4A4A-positive cells were diffusely seen in the interstitial area and slightly seen in the periphery of the epithelioid granuloma (Fig. 2g, h). Oral administration of irbesartan, nifedipine and trichlormethiazide was discontinued at the patient’s discretion. Three weeks after discontinuation of oral administration, swelling of the forearm, back of the hand and lower legs was improved. Based on these findings, a diagnosis of drug-induced granulomatous panniculitis was made.
DISCUSSION
Granulomatous drug eruptions are categorized as a rare subgroup of non-infectious granulomatous disease of the skin, characterized by a granulomatous pattern by predominance of histiocytes in the inflammatory infiltrate (1, 2). The 5 major types of cutaneous granulomatous drug eruptions are interstitial granulomatous drug reaction, drug-induced accelerated rheumatoid nodulosis, drug-induced granuloma annulare, drug-induced sarcoidosis, and miscellaneous presentations (2). It has been reported that several drugs, including angiotensin-converting enzyme inhibitors, anticonvulsants, antidepressants, antihistamine, anti-tumour necrosis factor (anti-TNF) agents, β-blockers, calcium-channel blockers, diuretics (furosemide, hydrochlorothiazide), herbal medications, histamine H2-receptor antagonists, immune checkpoint inhibitors, and lipid-lowering agents are involved in granulomatous reactions (2). In case 1, the symptoms improved after discontinuation of treatment with azosemide. In case 2, the skin symptoms improved after discontinuing administration of irbesartan, nifedipine and trichlormethiazide. In these cases, histopathological examination showed the presence of inflammatory infiltrates and granulomas mainly throughout the lobules of subcutaneous fat. Therefore, we made a diagnosis of drug-induced granulomatous panniculitis rather than erythema nodosum. Although the precise pathogenesis of drug-induced granuloma has not been elucidated, several mechanisms have been postulated: alteration of the antigenicity of dermal collagen and normal elaboration of collagen in the dermal repair mechanisms (4), an autoimmune phenomenon resulting from cytokine imbalance (5), and biochemical modifications that unbalance the activity of CD4 cells, particularly Th17 cells (6). We investigated the subtypes of macrophages immunohistochemically in the 2 cases in the current study. It is known that M1 macrophages, characterized by the expression of high levels of pro-inflammatory cytokines, promote granuloma formation and macrophage microbicidal activity. In contrast, M2 macrophages, characterized by the expression of anti-inflammatory cytokines, inhibit these effects and promote tissue remodelling and immunoregulatory functions (7). Among granulomatous diseases, the ratio of M1 and M2 macrophages has been studied in sarcoidosis, and it has been reported that M2 macrophages were more predominantly observed in systemic sarcoidosis than in cutaneous sarcoidosis (8). However, the polarization of each macrophage in drug-induced granulomatous panniculitis has not been investigated. In the current cases, M1 macrophages were mainly seen in the epithelioid granuloma and M2 macrophages were observed with a predominance in the interstitial area and periphery of the granuloma. The pattern of macrophage polarization may depend on the stage of granuloma formation. Further accumulation and examination of cases at various stages are necessary to determine the role of each macrophage in the formation of drug-induced granuloma.
In conclusion, we reported here 2 cases of drug-induced granulomatous panniculitis. The macrophages infiltrating tissue showed polarization in the lesion, which could be related to the formation process of drug-induced granulomatous panniculitis. Drug-induced granulomatous panniculitis is rare, but it is important to consider the patient’s drug history when searching for the cause.
REFERENCES
- Izikson L, English JC. Noninfectious granulomatous diseases: an update. Adv Dermatol 2006; 22: 31–53.
- Shah N, Shah M, Drucker AM, Shear NH, Ziv M, Dodiuk-Gad RP. Granulomatous Cutaneous drug eruptions: a systematic review. Am J Clin Dermatol 2021; 22: 39–53.
- Perrin C, Lacour JP, Castanet J, Michiels JF. Interstitial granulomatous drug reaction with a histological pattern of interstitial granulomatous dermatitis. Am J Dermatopathol 2001; 23: 295–298.
- Magro CM, Crowson AN, Schapiro BL. The interstitial granulomatous drug reaction: a distinctive clinical and pathological entity. J Cutan Pathol 1998; 25: 72–78.
- Lamrock E, Brown P. Development of cutaneous sarcoidosis during treatment with tumour necrosis alpha factor antagonists. Australas J Dermatol 2012; 53: e87–e90.
- Vigne C, Tebib JG, Pacheco Y, Coury F. Sarcoidosis: an underestimated and potentially severe side effect of anti-TNF-alpha therapy. Joint Bone Spine 2013; 80: 104–107.
- Asai J. What is new in the histogenesis of granulomatous skin diseases? J Dermatol 2017; 44: 297–303.
- Isohisa T, Asai J, Kanemaru M, Arita T, Tsutsumi M, Kaneko Y, et al. CD163-positive macrophage infiltration predicts systemic involvement in sarcoidosis. J Cutan Pathol 2020; 47: 584–591.