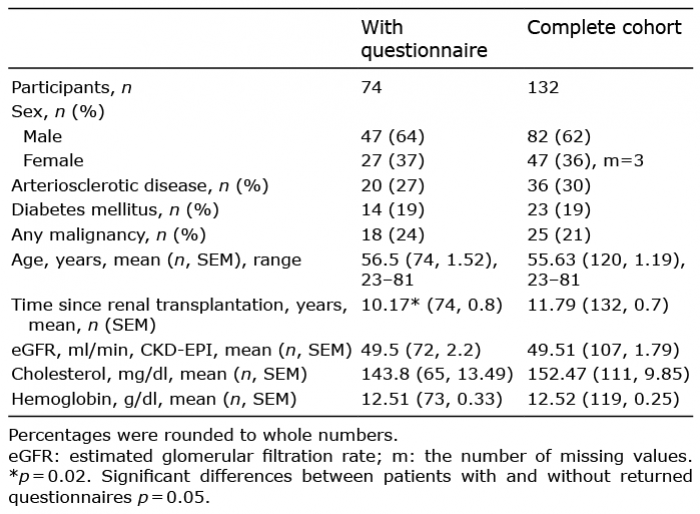
Table I. Patient characteristics
1Department of Internal Medicine, Division of General Internal Medicine and Nephrology, Robert-Bosch-Hospital, Stuttgart, 2Occupational Dermatology, Department of Dermatology, University Hospital Heidelberg, Ruprecht Karls University, Heidelberg, 3Institute for Medical Psychology, University Giessen, Giessen, and 4Department of Internal Medicine, Division of Nephrology, DKD Helios Klinik, Wiesbaden, Germany. E-mail: severin.schricker@rbk.de
Acccepted Feb 10, 2020; Epub ahead of print Feb 13, 2020
Acta Derm Venereol 2020; 100: adv00066
Chronic kidney disease (CKD) can lead to chronic pruritus (CKD-aP) and may resolve after renal transplantation (RTx) (1). However, little is known about the prevalence of CKD-aP after RTx. The present study investigated a cohort of patients who received a functional graft, but did not require dialysis, and tried to identify correlations between the incidence of pruritus and a range of clinical and laboratory findings.
Patients and controls
A cohort of patients who underwent RTx between 1976 and 2014 in a single nephrology centre in Wiesbaden, Germany was evaluated. Patients were recruited during their routine follow-up visit if they had received a functional graft and did not require dialysis. The study was approved by the Institutional Review Board. A total of 132 patients provided informed consent and were recruited into the study. A questionnaire was used to collect information from each patient relating to current itch, history of pruritus and skin diseases.
The questionnaire included the following questions: Do you suffer from itching? (yes/no); Did you suffer from prolonged itching during your previous period of dialysis? (yes/no/I don’t know); How long have you suffered from itching? (days/months/years); Where does it itch? (face/scalp/head+neck/arms/back/hands/abdomen/legs/breast/feet/anal+genital area); How would you rate the intensity of your current itch in the last 24 h on a visual analogue scale from 0 (no itch) to 10 (most imaginable itch)? Is the itching worse during a specific season (summer/autumn/winter/spring); Have you ever seen a doctor because of itching? (no/dermatologist/general practitioner/other); Do you suffer from a skin disorder diagnosed by your doctor? (psoriasis/eczema/atopic dermatitis/other skin disease); Do you suffer from any of the following conditions (dry/flaky/greasy skin).
A range of data were extracted from medical records, including clinical and laboratory parameters, the medication administered during follow-up, the time elapsed since RTx, sex, age, blood pressure and immunosuppressant medication, frequent comorbidities (e.g. diabetes, vascular diseases, malignancy, and dermatological disease), laboratory data (creatinine, calculated glomerular filtration rate (CKD-EPI), haemoglobin, cholesterol levels, proteinuria), and medications (cyclosporine, tacrolimus, sirolimus, everolimus).
Chronic itch (CI) was defined as itchy skin lasting for more than 6 weeks (2). The present study defined patients as having CI when they reported itching for months or years. History of CI was assumed if prolonged itching was reported during the pre-transplant period of dialysis dependence.
Statistical analysis
Statistical analysis was performed using SPSS Statistics for Windows, Version 20.0. (Armonk, NY, USA: IBM Corp.). Two data outliers were removed from the analyses because of implausibility. The Mann-Whitney U test was used to compare the medians of independent groups, and χ-squared test and Pearson’s and Fisher’s exact tests were used to identify significant differences between frequencies in each category of data. The significance of correlations was determined by Spearman’s rho statistic.
Patient characteristics are shown in Table I. Of the 132 patients recruited during routine follow-up, 74 returned the questionnaire (56.1%); the mean length of time since RTx was 10.17 ± 0.78 (standard error of the mean; SEM) years. Eight of these 74 patients reported that they experienced a clinical form of dermatosis other than chronic pruritus and were excluded from further analysis. Eleven of the remaining 66 patients (17%) reported that they experienced itch; 8 of these (12%) were diagnosed with CI (2 of these patients had experienced itch for months, while 6 had experienced itch for years). The prevalence of CI prior to RTx was higher (35%) than after transplantation (12%) (Table II). The mean pruritus VAS score in cases diagnosed with CI was 3.2 (median: 2, n = 3 reported a pruritus intensity > VAS 3). There was no significant association between the occurrence of pruritus and the time elapsed since transplantation. In addition, there was no significant association between the presence of CI before (i.e. while on dialysis) and after transplantation (including patients with (n = 74, df = 2, p = 0.114) and without (n = 66, df = 2, p = 0.120) dermatosis). There was a moderate correlation between the intensity of CI and transplant function (n = 62, CKD-EPI r = 0.30, p = 0.018), while overall transplant function was good (estimated glomerular filtration rate (eGFR) (ml/min, CKD-EPI) 49.5 ± 2.2 (SEM), n = 72). All patients received immunosuppressive treatment.
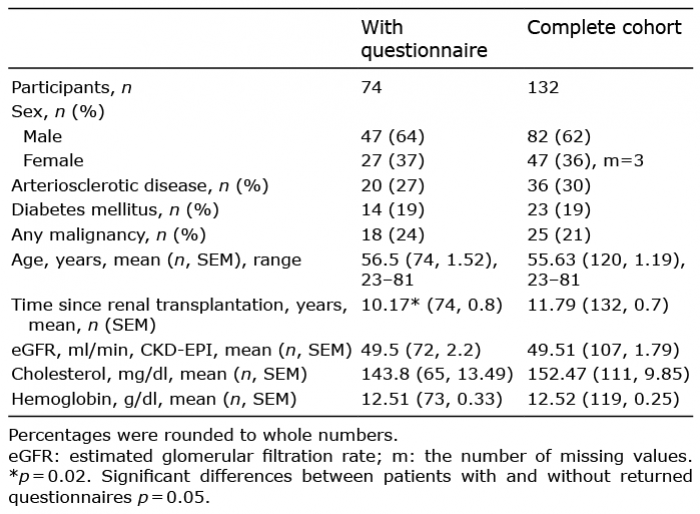
Table I. Patient characteristics
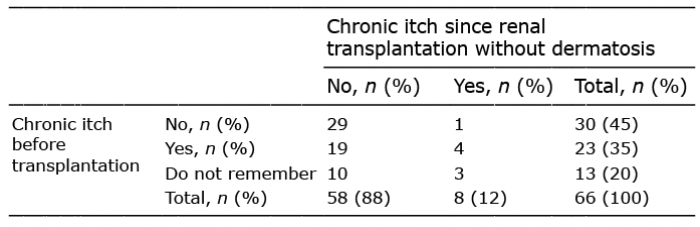
Table II. Prevalence of chronic itch before and after transplantation
The prevalence of pruritus and associated factors in dialysis patients is well documented (3–7). However, a substantial proportion of patients with functioning renal transplants also experience pruritus (8, 9) and little is known of this condition. Altmeyer et al. (1) previously reported that itching stopped following transplantation, while other authors reported a high prevalence of pruritus in the post-transplant population (9, 10). It is therefore important that we expand our understanding of this condition, as pruritus is associated with important dimensions in the quality of life (9–11).
The present study confirmed that the prevalence of chronic pruritus in RTx patients was lower than in pre-transplantation or dialysis patients. These findings are in line with previous papers reporting a prevalence of CI in 11–32% of patients after transplantation (9, 10). Our analysis showed that some patients experienced CI more than 10 years after RTx, which might be brought about either by a persisting itch stimulus or a previous sensitization of itch-signalling pathways (12). The prevalence of CI could potentially be related to under-reported dermatological (xerosis, atopic dermatitis) or systemic diseases, or certain laboratory factors (such as parathyroid hormone and phosphorus), as reported previously (3–5); these factors were not evaluated in the present study.
This study has some limitations. First, due to the design of the questionnaire with regards to the pre-transplantation period, it is possible that recall bias may have occurred. This might explain the somewhat lower prevalence of CI in dialysis patients compared with some previously published data (10). On the other hand, our data is more in line with more recent publications involving dialysis patients with pruritus which reported a prevalence of CI of approximately 25% (5). Furthermore, it was not possible to investigate the correlation between the duration of itching before and after transplantation, or to investigate the potential impact of certain drugs, such as loop diuretics (12), because only a limited amount of data regarding these compounds have been obtained. Finally, an observational approach does not allow conclusions to be drawn on causality. This study found no evidence of a correlation between the history of itching during dialysis and after transplantation, thus suggesting that the pathogenesis of itch differed in patients undergoing RTx. On the other hand, a previous study involving sequential skin biopsies reported restored uraemic skin alterations after RTx (1), while another study reported the persistence of uraemic-induced alterations in connective tissue (13), with sustained clinical problems.
In conclusion, compared with patients on dialysis, the prevalence of pruritus seems to be lower after renal transplantation, although this could not be proved statistically.
The authors have no conflicts of interest to declare.