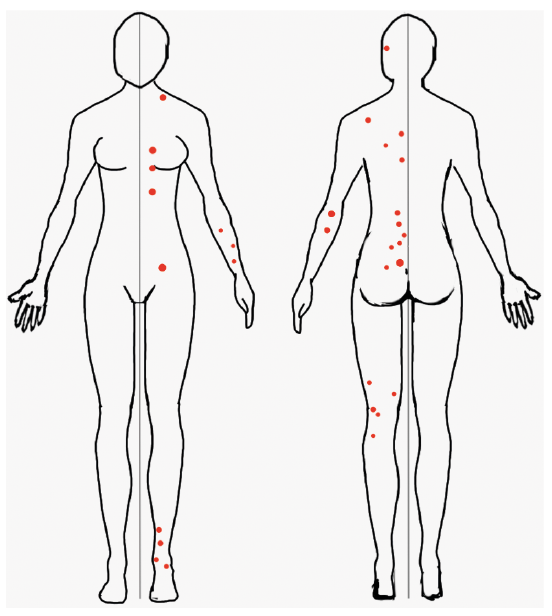
Fig. 1. Localization of basal cell carcinomas on patient’s body.
Department of Dermatology, Venereology and Allergology, Wroclaw Medical University, Chalubinskiego 1, PL-50-368 Wroclaw, Poland. E-mail: jacek.szepietowski@umed.wroc.pl
Accepted Mar 18, 2020; Epub ahead of print Mar 19, 2020
Acta Derm Venereol 2020; 100: adv00101
Basal cell carcinoma (BCC) is the most frequent skin malignancy, usually evolving as a solitary lesion on sun-exposed areas (1). Much less frequently, multiple BCCs may be a sign of syndromic disorder, such as naevoid basal cell carcinoma syndrome (NBCCS) or Bazex-Dupré-Christol syndrome. The unilateral localization of syndromic multiple BCCs is possibly due to post-zygotic mutations (2); however, non-syndromic cases of unilateral multiple BCCs are extremely rare. We report here a case of a patient with non-syndromic unilateral BCCs and a literature review of reported cases.
A 55-year-old Caucasian woman was admitted to the Dermatosurgery Unit, Department of Dermatology, Venereology and Allergology, Wroclaw Medical University, due to multiple skin lesions. The patient reported that the first lesion appeared on the left calf 20 years earlier, following a premature menopause. Initially, the lesion was red and pruritic (numerical rating scale 4/10 points). The lesion healed spontaneously after 3 months. Since then, multiple lesions, limited to the left side of the body, started to emerge. The patient did not report any comorbidities; she was generally in good health. The woman reported extensive ultraviolet (UV) exposure, frequent burning and use of tanning beds, but denied any radiation exposure. Moreover, she declared working with harmful substances (e.g. formaldehyde, sulphur dioxide). To date, she has been on hormonal replacement therapy for 19 years and associated it with the skin lesions. The family history towards dermatological diseases was negative, although a melanoma-related death of the patient’s aunt could not be excluded.
On admission, physical examination revealed multiple, red, scaling patches (26 superficial BCCs) as well as non-pruritic nodules (5 nodular BCCs) localized exclusively on the left side of the body; namely, on the trunk, extremities, neck and behind the ear (Figs 1 and 2). Complete cutaneous inspection did not reveal any other changes on the skin. Due to lack of other findings, NBCCS was excluded. Histological examination of multiple lesions confirmed superficial and nodular BCCs.
It was decided to excise nodular type of BCCs (during step-by step primary closure) and to use cryosurgery (a total of 3 sessions) with nitric dioxide for superficial type of BCCs, with very good aesthetic results. At the first follow-up (1 month after treatment) the majority of the superficial lesions had healed with good aesthetic outcome and the nodular ones had scarred properly.
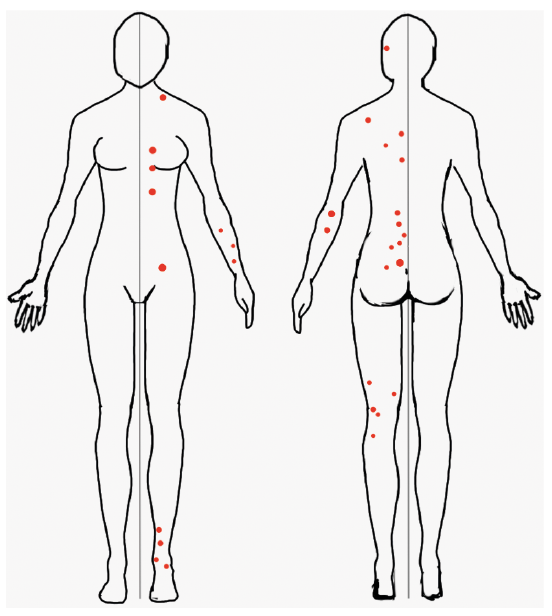
Fig. 1. Localization of basal cell carcinomas on patient’s body.
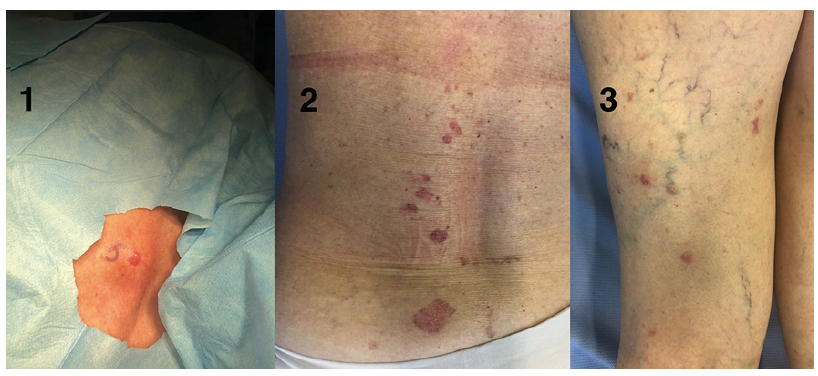
Fig. 2. (1) Nodular lesion on the patient’s calf. (2) Multiple superficial basal cell carcinomas (BCCs) on the patients’ back. (3) Multiple superficial and nodular BCCs on the patients’ leg.
BCC is the most common human malignancy. It usually affects people over the age of 50 years, and is more frequent in men than women. However, its incidence has been increasing recently among pale-skinned, young individuals with episodic sun exposure. The main cause is not yet known, but the main risk factor for developing BCC is excessive exposure to UV. Light skin, tendency to burn, use of tanning beds, radiation exposure and immunosuppressive therapy also play an important role in the pathogenesis of BCC (1). BCC does not present a unique characteristic lesion due to multiple clinical manifestations. Although BCC does not metastasize or cause death, possible local infiltration can lead to pain, disfigurement and an increased morbidity rate. The most frequent localization is strongly connected with its risk factors: solitary tumours are primarily localized on sun-exposed areas. Multiple BCCs are usually connected with underlying gene mutation (e.g. NBCCS and PTCH1 gene) and accompanied by other disturbances (jaw cysts, skeletal defects, other neoplasms) (3). The diagnosis of BCC can be made by experienced dermatologists on clinical examination with the use of dermatoscope. However, skin biopsy is usually performed to confirm the clinical diagnosis and to establish histological type and its aggressiveness (4).
First-line therapy for BCC is surgical excision. The methods consist of standard excision with a 4–5-mm margin (5) and Mohs micrographic surgery. Other therapies include the use of cryotherapy, topical use of imiquimod and 5-fluorouracil, photodynamic therapy (PTD) and radiation therapy. For the rare, metastatic or advanced BCC where surgery is no longer an option, treatment with vismodegib has beneficial effects (6). In the current case it was decided to use 2 different methods to remove patients’ lesions. The nodular ones were surgically removed, and the multiple, superficial ones were treated with cryotherapy. At the first follow-up, 1 month after surgery, all treated areas had healed properly.
A MEDLINE search of the literature in English was conducted for the cases of non-syndromic multiple unilateral BCC using the words and phrases “multiple basal cell carcinomas” and “unilateral”. A total of 280 articles was found, from which we have chosen only those related to non-syndromic presentation. Finally, we analysed 5 case reports concerning unilateral multiple BCC without syndrome association (Table I).
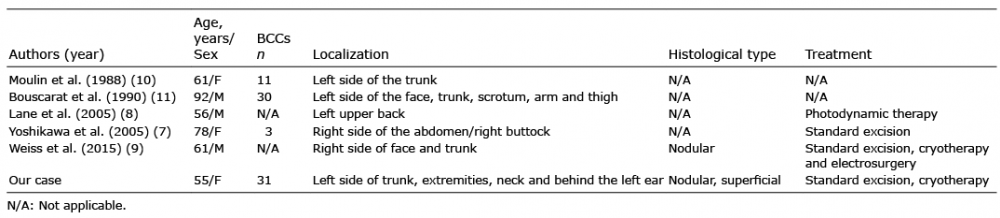
Table I. Literature review
Yoshikawa et al. (7) described a 78-year-old patient with 3 BCCs on the right side of her trunk. There were no associated comorbidities or anomalies indicating NBCCS or other syndromes. The patient was treated successfully with standard surgical excision. Even more pronounced case of unilateral localization of multiple BCCs was described by Lane et al. (8), where a 56-year-old Caucasian male presented with 14 BCCs on the left side of his body. As in the previous report, Lane et al. (8) did not find any associated lesions or abnormalities. Treatment with photodynamic therapy (PDT) was effective. Weiss et al. (9) described a 61-year old Cuban man with a 33-year history of numerous nodular BCCs on the right side of his body. The patient denied any extensive exposure to sun, radiation or chemicals. During all follow-ups he was treated with cryosurgery, electrosurgery and standard surgery. The researchers did not find any association with known syndromes. Moulin et al. (10) described a case of a 61-year-old woman with 11 BCCs on the left side of her trunk, but no additional anomalies were found. Moreover, Bouscarat et al. (11) described a 91-year-old patient with 70 years’ history of BCCs of the left side of the body.
Based on the above-mentioned case reports, one may conclude that a case of non-syndromic multiple unilateral BCCs is an extremely rare finding. We decided to publish this case report because our patient had the highest number of unilateral BCCs ever reported. In addition, such a manifestation can be a difficult diagnostic case, even for experienced dermatologists. The literature review of similar case reports will improve insight into the aetiology, possible heritance traits and management of this disorder. However, it is important to emphasize that the literature does not present indisputable proof of the existence of a separate syndrome.