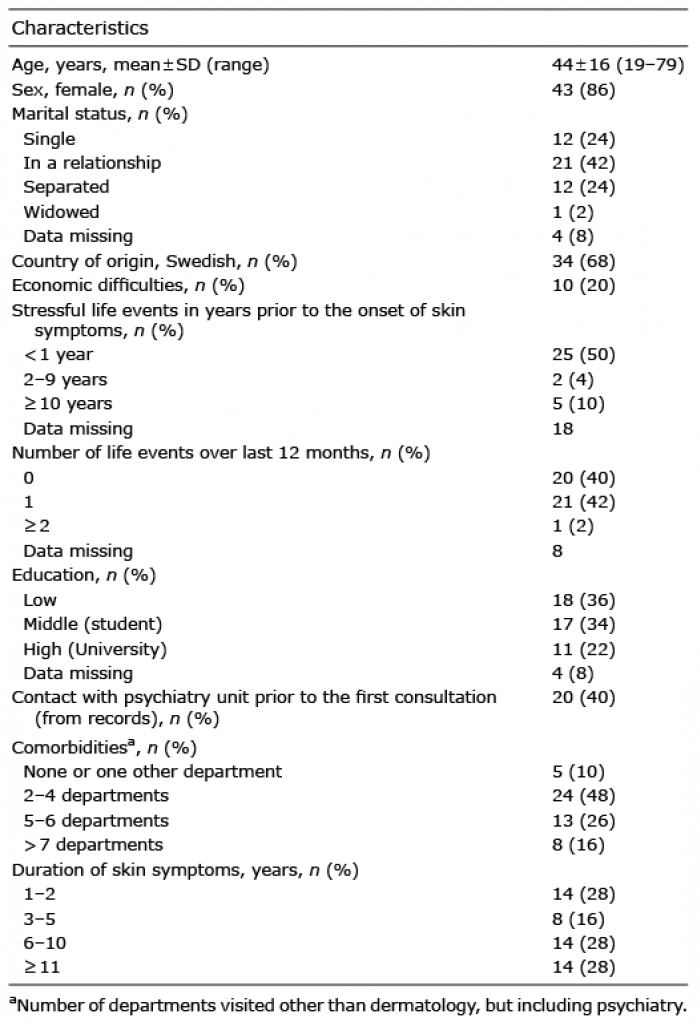
Table I. Characteristics of patients seen at the psychodermatology unit over a period of 1 year (n = 50)
Department of Dermatology and Venereology, Skåne University Hospital, Malmö, Sweden
Clinical epidemiological knowledge concerning psychodermatology patients is scarce. The objective of this study was to assess morbidity in a new psychodermatology service. Information was gathered from patient records at the psychodermatology unit in Skåne University Hospital, Malmö, Sweden, from 1 February 2017 to 31 January 2018. All patients were screened with the Hospital Anxiety and Depression Scale (HADS) and the Dermatology Life Quality Index (DLQI) at baseline and after 12 months. Additional information was collated from the patient records. A total of 50 patients were treated during the 12 months, 86% were women, mean age 44 years (standard deviation (SD) 16 years). Itch was present in 72% of patients. Forty-two percent of patients were diagnosed with mood disorders, 30% with personality disorders, and 16% with delusional disorders. At baseline 40% of patients had a DLQI score >11, clinical depression was present in 14%, and clinical anxiety in 28%. These data emphasize the need for access to a multidisciplinary unit for dermatology patients.
Key words: psychodermatology; symptoms; signs; healthcare services.
Accepted Mar 12, 2020; Epub ahead of print Mar 17, 2020
Acta Derm Venereol 2020; 100: adv00126.
Corr: Florence J. Dalgard, Department of Dermatology and Venereology, Skåne University Hospital, Jan Waldenströms gata 7, SE-214 21 Malmö, Sweden. E-mail: florikje@gmail.com
The aim of this study was to describe the characteristics of patients seen at a psychodermatology unit. Information was gathered from patient records at the psychodermatology unit of Skåne University Hospital, Malmö, Sweden. All patients were screened for mood disorders and quality of life. A total of 50 patients were treated during a 1-year period, 86% women, mean age 44 years. Itch was present in 72% of patients, 42% had mood disorders, 30% personality disorders, and 16% delusional disorders. Forty percent of the patients had a very large impact on their quality of life. These findings highlight the importance of psychodermatology services.
The significant psychological and psychiatric comorbidity of dermatological patients across Europe has been demonstrated in a large sample of dermatological patients (1). Dermatological patients with psychiatric comorbidity can be challenging for dermatologists, and there is a need for multidisciplinary care to offer treatment to patients with concomitant dermatological and psychiatric conditions (2). There are no established specialized units in most hospitals in Europe (3–6), despite evidence of the cost-effectiveness of such units (4, 7, 8).
The morbidity of psychodermatology patients has been described in case studies, mostly recording diag-noses (5) or by recording skin symptoms and signs (9, 10). Psychodermatology conditions have been classified with respect to aetiology, and categorized into 3 groups: primary psychiatry patients with secondary skin complaints, patients with primary skin diseases and secondary psychological complaints, and, lastly, a mixed group (11). However, there has been very little clinical epidemiological research in psychodermatology.
The primary aim of this study was to describe the characteristics of patients in a new multidisciplinary clinic, from its inception for a period of 12 months, with a focus on demographic factors, patient-reported outcomes and clinical outcomes.
This is a retrospective study based on routinely collected health data. Information for the study was gathered from patient records held in Melior by the investigators (FD, IA, KS). Melior is an electronic patient record system that supports both inpatient and outpatient care in many hospitals in Sweden. This program enables access to records kept by other departments in the hospital. All healthcare providers in the study had access to Melior through a personal code.
The study included all new patients who were seen in the psychodermatology unit during the 1 year from the inception of the unit on 1st February 2017 until 31st January 2018. All patients were referred from the Department of Dermatology and Venereology, Skåne University Hospital and examined by a dermatologist prior to their first visit to the psychodermatology unit.
Key features of the psychodermatology service
The healthcare providers at the psychodermatology unit include 2 dermatologists, one trained as a psychodynamic psychotherapist and the other in training in psychodermatology, one psychiatrist trained as a psychodynamic psychotherapist and one social counsellor trained as a short-term psychodynamic psychotherapist. This team structure was adapted from experience published by colleagues in other countries (12).
The consultations in psychodermatology encompass standard pharmacological treatment combined with a psychiatric or psycho-therapeutic intervention. Meeting the patients without judging them, validating their experience of symptoms, and having a comfortable time-frame for the first meeting are all part of the establishment of a secure alliance between patient and healthcare providers (13).
The first consultation for all patients is a team consultation with a dermatologist, psychiatrist and a social counsellor. The duration of the first consultation is 45 min and a plan for follow-up is made. Prior to the consultation each patient completes validated questionnaires assessing mood disorders and quality of life. After the first consultation an evaluation is made by the team. Some patients are offered short-term psychotherapy by the social counsellor, some are offered psychiatric consultations with the psychiatrist including psychotherapy, some patients are provided with counselling with the social counsellor and, finally, some patients are referred to external psychological help in the primary care unit. A 30-min follow-up team consultation is usually offered to patients. Patients are routinely screened at follow-up, after 6 months, after 12 months, and at discharge, with the same questionnaires that were completed at baseline.
Definitions, criteria and descriptions of data collected
Sociodemographic data collected included age, sex, whether of Swedish or non-Swedish origin, marital status and education level: low (without upper secondary education), middle (with upper secondary education) or high (higher education). Every patient was asked about stressful life events, especially traumatic events or bereavements. The number of years that these events occurred prior to the onset of skin symptoms were categorized as: 1 year or less, 2–9 years, or 10 or more years. The number of these negative life events during the last year were categorized as: none, 1, or 2 or more.
If a patient had previously had any consultation with the psychiatric service they were categorized as “primary psychiatric”. Comorbidities were inferred from the number of hospital departments, other than dermatology, attended by patents since 2013. This was recorded as “none or 1 other department”, “2–4 departments”, “5–6 departments” or “more than 7 departments”.
Duration of skin symptoms was extracted from patient records and categorized as: “less than 1 year”, “3–5 years”, “6–10 years” or “11 or more years”. The number of consultations that each patient had with the psychodermatology team and with psychotherapy was counted over the 1-year period. All cancellations are routinely registered in Melior, and these were also counted for each patient.
The presenting complaints and objective signs recorded at the first consultation of each patient were analysed, along with the International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10) dermatological and psychiatric diagnoses, based on the dermatologist’s and psychiatrist’s opinions. All patients were seen at least once by the psychiatrist, and so personality disorders and delusional disorders were described or confirmed by the psychiatrist.
The Hospital Anxiety and Depression Scale (HADS) was used to identify mood disorders; however, this instrument is a screening tool, not a diagnostic tool. A score above the cut-off point of 11 indicates that the patient needs to be seen by a mental health specialist to confirm the diagnosis (14, 15). All patients completed the Dermatology Life Quality Index (DLQI) (16), a 10-item dermatology-specific instrument that evaluates the impact of skin disease on patient’s lives over the last week. Item number 9 concerns sexual difficulties. The total scoring of the DLQI is 0–30: values from 0 to 1 indicate no effect, 2–5 a small effect, 6–10 moderate effect, 11–20 very large effect, and 21–30 an extremely large effect on a patient’s life.
Topical treatment, systemic dermatological treatment, and psychopharmacological treatment were extracted from the record of prescriptions. Ultraviolet (UV) treatment was included, but only if a patient had attended at least 3 times. Psychoeducation (an important non-pharmacological treatment) was often part of the consultation, but was not recorded.
Statistical analysis
SPSS version 24 software (IBM Corp, Armonk, NY, USA, released 2016). IBM SPSS Statistics for Windows was used to analyse the data. Continuous variables were categorized and other variables were dichotomized when convenient. The analyses were descriptive, calculating frequencies. The data are presented in raw form as numbers and percentages.
The number of consultations and associated patient identities were obtained by the research nurse (EW) by finding through the Melior software a list of the consultations in the psychodermatology unit. Relevant variables for this manuscript were computed by FD and IH from the patient records in Melior.
Data cleaning was performed twice by FD alone and then twice together with IH, by systematically double-checking variables in SPSS against the patient records, thereby reducing missing variables. One investigator worked with the data-set, while the other worked at another computer with the patient records, swopping roles regularly during several sessions.
Ethics
The study was approved by the regional ethics committee in Southern Sweden (Darie number 2018/543).
During the 1-year study timeframe, 50 patients were referred to the psychodermatology unit. Reasons for referral included: difficult encounter, treatment adherence problems, clinical depression or anxiety, or complex psychosocial situation. The mean age was 44 years (standard deviation (SD) 16 years) and 86% were females. Sixty-eight percent of the patients were of Swedish origin and half of the patients were not in a relationship. Forty percent had previously had advice from the psychiatry service. Forty-eight percent of the patients had been cared for in more than 2 departments, and 56% of the patients had had skin symptoms for more than 6 years (Table I). Forty-eight percent of the patients had between 2 and 5 consultations, 46% had psychotherapy, and 26% cancelled one or more appointments (Table II).
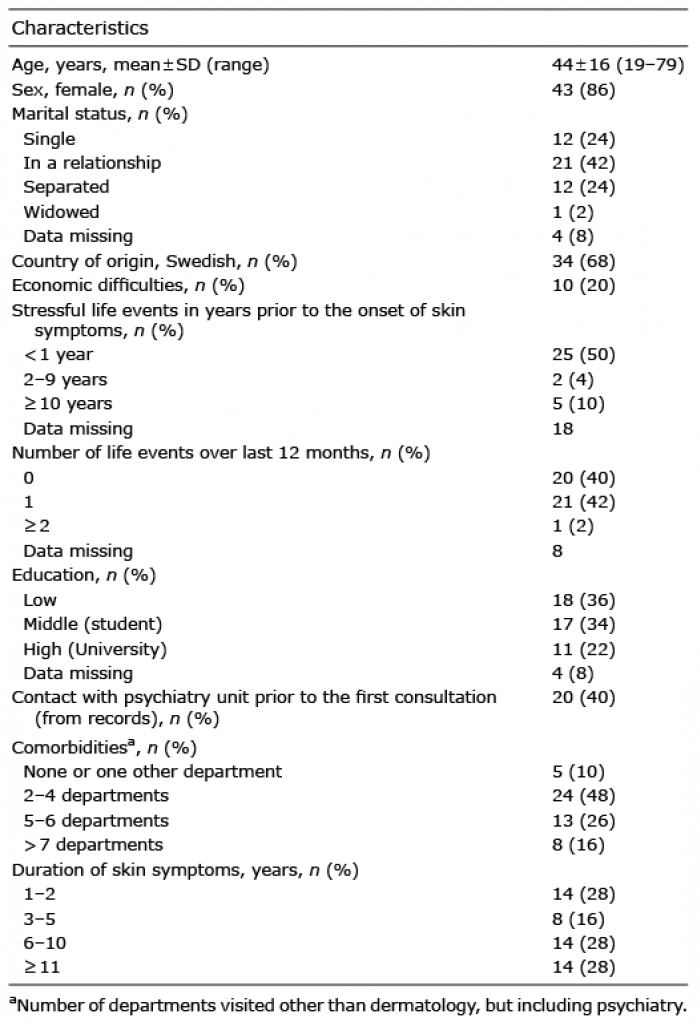
Table I. Characteristics of patients seen at the psychodermatology unit over a period of 1 year (n = 50)
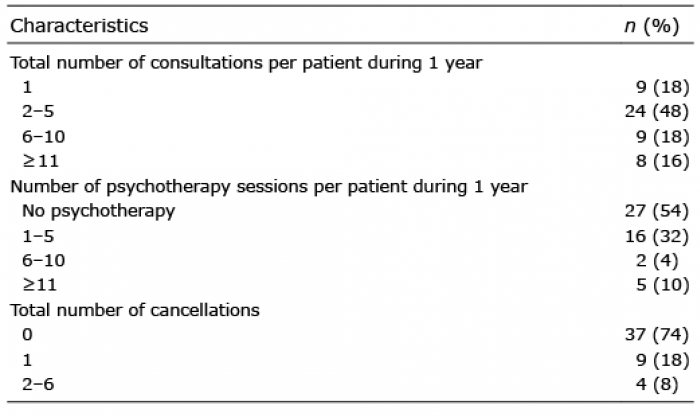
Table II. Distribution of number of team consultations (including follow-ups) per patient, psychotherapy (with the psychiatrist or the social worker) sessions per patient, cancellations in total during 12 months
Seventy-two percent of the patients reported itch, 50% had pain or sore skin, 42% had sleeping problems, and 6% had suicidal ideation (Table III). Forty-six percent of the patients had excoriations, and 24% showed no skin signs. The largest dermatology groups were pruritus, prurigo nodularis and prurigo (together 40%), and acne excoriée (14%) (Table IV). The largest psychiatry groups were mood disorders including depression and anxiety (42%), personality disorders (30%) and delusional disorders (16%) (Table IV).
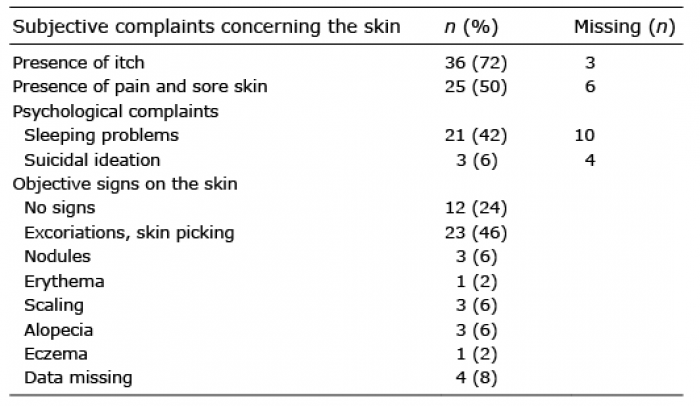
Table III. Presenting complaints from the patients and objective signs described by the dermatologist at first consultation at the psychodermatology unit (n = 50)
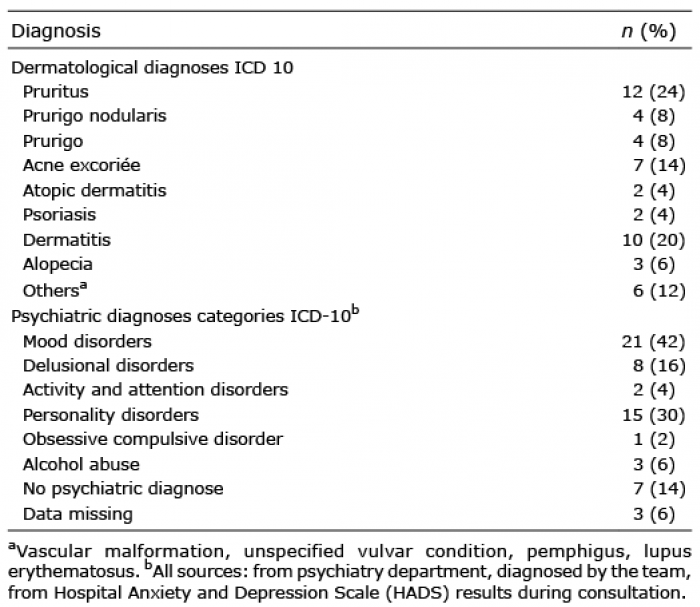
Table IV. International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10) diagnosis distribution in patients at the psychodermatology unit from 1 February 2017 to 31 January 2018
The DLQI and HADS scores at first consultation, at 6 and 12 months are shown in Table V. Forty percent of the patients initially experienced a very large effect on their lives, 10% of whom experienced an extremely large effect. However, by 12 months only 14% experienced a very large effect on their lives, of whom only 4% experienced an extremely large effect. Initially 22% of patients reported sexual difficulties (DLQI question 9), with 26% at 12 months. The proportion of patients with clinical depression decreased from 14% to 6% during 12 months, and the proportion of patients with clinical anxiety decreased from 28% to 10%.
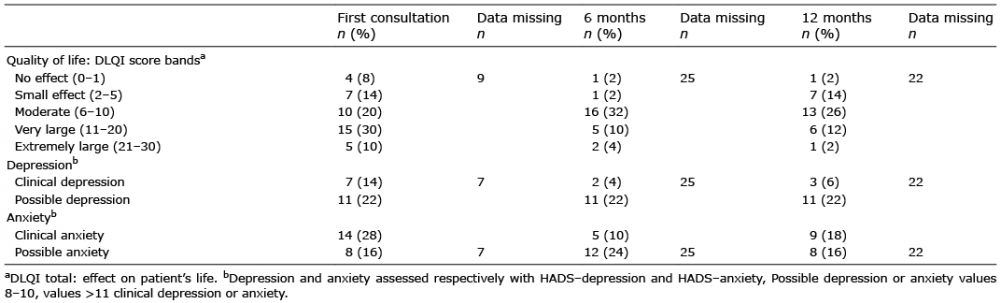
Table V. Dermatological quality of life (Dermatology Life Quality Index; DLQI) and mood disorders (Hospital Anxiety and Depression Scale (HADS) – depression and anxiety > 11) at first consultation, after 6 and 12 months among all patients seen at the psychodermatology unit during 12 months (n = 50)
Overall, 82% of patients received topical treatment, 46% with high-potency steroids. Twenty-two percent of patients received ultraviolet (UV) treatment. Dermatological systemic treatment was used in 54% of patients, including 26% who were prescribed antihistamines, 10% antibiotics, and 10% gabapentin (Table VI).
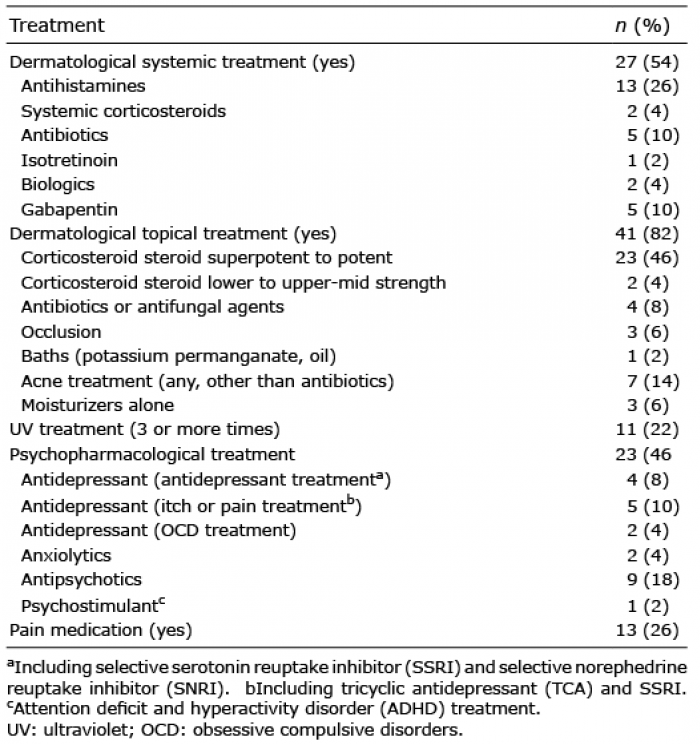
Table VI. Dermatological and psychopharmacological treatment given to 50 patients at the psychodermatology unit during 12 months
This descriptive study provides, for the first time, a detailed account of the reality of the clinical experiences likely to be encountered by healthcare professionals and planners considering developing a psychodermatology service. The modest improvement in both patient-reported and clinical outcomes provides justification for the development of such services, with continuing close audit of activities and outcomes.
The largest groups of psychiatric conditions were depression and anxiety, followed by personality disorders and delusional infestations. Difficulties arose in the classification of patients because of challenges in determining whether a patient was primarily psychiatric or primarily dermatological, as the symptoms were mostly concomitant. The only aspect of a patient’s history that could make it likely that a patient was primarily psychiatric was if the patient had previously attended the psychiatric unit, which was the case for 40% of patients. Nevertheless, a high percentage of patients had mood disorders at baseline that improved over 12 months, suggesting that, in many cases, depression or anxiety might be secondary to the skin condition.
Symptoms and signs
Most of the patients in this study (72%) reported itch, which is more than the 54% of patients attending general dermatology clinics across Europe who reported itch as a symptom (17). The range of somatic and psychiatric comorbidity described from such pruritus services is similar to that encountered in this report (18). This could be because dermatologists find that itchy patients are difficult to treat in a general out-patient clinic and, therefore, some are referred to a psychodermatology clinic. Furthermore, the number of attendances at other departments illustrates the high rate of comorbidities and the clinical complexity of many patients attending a psychodermatology unit.
It is likely that there is overlap between patients seen in psychodermatology units with patients encountered in pruritus units specializing in pruritus: indeed 40% of our patients had either pruritus, prurigo nodularis or prurigo (19, 20).
The distribution of dermatological ICD-10 diagnoses (Table IV) were in accordance with both symptoms and objective signs (Table III): the majority of patients were diagnosed with an itchy skin disease, including diagnoses of pruritus, prurigo nodularis, prurigo, acne excoriée and atopic dermatitis. There is little information about the relationship between objectively assessed and subjectively assessed skin morbidity, and this should be explored further (21, 22).
A high proportion of the patients in the current study had psychiatric morbidity, in parallel with findings from other clinical epidemiological studies of psychodermatology units (23, 24) and of dermatology out-patient clinics (25–27). In the current study mood disorders were the largest group, both from the ICD-10 diagnoses (Table IV), and when assessed with HADS (Table V). Overall, 14% of the patients had clinical depression, and 28% clinical anxiety, which is more than in a recent study of general dermatological patients, where 10% had clinical depression and 17% clinical anxiety (1).
The second largest group of patients with psychiatric morbidity was those with personality disorders (PD), with a significantly higher prevalence than in a primary care setting (30% vs. 6%) (28) and 10 times higher than in the general population (3%) (29). For practical reasons we were not able to examine the subgroups of personality disorders. Nevertheless, this high prevalence adds to the challenge that dermatologists face in a conventional dermatology consultation when meeting, unprepared, a patient with PD. The chances of receiving a major complaint from patients with PD may be high (30) and frequent encounters with patients with PD may increase the risk of dermatologist “burnout” (31).
The third largest group of psychiatric disorders were patients with delusional infestation (DI). When we created the psychodermatology unit we decided that all patients with clinical DI would be labelled in the hospital software Melior with a non-specific descriptive diagnosis such as “dermatitis” or “pruritus”, corresponding to the presenting complaint. In Sweden, patients have access to their records and therefore may easily become upset if they see a stigmatizing diagnosis. Patients with DI are strongly convinced about their disease and, in order to build up a good relationship, it is crucial that they experience being heard without judgement (32). The psychiatrist added a psychiatric ICD-10 diagnosis later in the psychotherapeutic journey when a good relationship had been established with the patient. Overall, this approach has been accepted by the patients.
Most patients attending the unit have chronic conditions, for which it is unrealistic to expect either a dermatological or psychiatric “cure”. However, aiming for some improvement in quality of life may be achievable for these complex patients. Therefore, the use of validated patient-reported outcome measures, such as the DLQI and the HADS, to guide clinical decisions, to assess improvement and to evaluate the effectiveness of the clinical service is appropriate, meaningful and feasible.
Our impression is that, overall, the cancellation frequency is low (8% cancelled more than once). Most of the cancellations were actively made by the patients. We consider the cancellation frequency to be similar to the frequency in the general dermatological clinics; however, this data is not available. Our policy at the psychodermatology unit is the same as in the dermatology department: patients who do not turn up are contacted by phone or by letter and given a new appointment.
This clinical epidemiological descriptive study attempted to standardize symptoms and signs, as well as clinical and other patient outcomes, in a heterogeneous group of patients. The findings are novel and provide valuable information to clinicians regarding the morbidity burden of a substantial group of dermatological patients.
Nevertheless, some limitations should be mentioned. The relatively small sample size makes more detailed statistical analysis impossible. This data-set is based on our first year of work in a multidisciplinary setting, and we continue to explore ways to standardize our approach. We intend to analyse the additional data that has accumulated over the last 2 years, and to define more clearly the patient pathways integral to our delivery of care.
Overall, this report shares our experience from the psychodermatology unit in Malmö concerning the dermatological and psychiatric morbidity of patients, by summarizing patients’ reported and clinical outcomes over 1 year. The findings illustrate the considerable symptomatology experienced by a substantial group of patients, and the challenges faced in a standard dermatology clinic setting by dermatologists who are not necessarily trained to handle psychiatric disease. Our data show the need for, and the meaningfulness of, multidisciplinary units as part of a dermatology service delivery.
We thank the staff at the department of dermatology in Malmö for practical help with patient management. A special thanks to Laura von Kobyletski for her input, and to Andrew Finlay for language corrections. We thank the Swedish Hudfonden for funding.