ORIGINAL REPORT
Exploring Patient Pain Experiences during and after Conventional Red Light and Simulated Daylight Photodynamic Therapy for Actinic Keratosis: A Qualitative Interview Study
Alexandra SJÖHOLM1,2, Magdalena CLAESON1,2, John PAOLI1,2 and Birgit HECKEMANN3,4
1Department of Dermatology and Venereology, Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Gothenburg, 2Region Västra Götaland, Sahlgrenska University Hospital, Department of Dermatology and Venereology, Gothenburg, 3Institute of Health and Care Sciences, Sahlgrenska Academy, University of Gothenburg, Gothenburg, and 4Region Västra Götaland, Sahlgrenska University Hospital, Department of Anaesthetics and Intensive Care, Gothenburg, Sweden
Simulated daylight photodynamic therapy is a relatively new and potentially less painful alternative to conventional red light photodynamic therapy for actinic keratosis. Qualitative research exploring patient experiences of pain and skin reactions during these treatments is scarce. To address this, semi-structured interviews were conducted of 10 patients aged 60–81 years with symmetrically distributed actinic keratoses 4 weeks after split-face treatment with conventional red light photodynamic therapy and simulated daylight photodynamic therapy. The participants were recruited from an ongoing clinical randomized trial. Interviews (median length 35 min) were conducted between June 2022 and January 2023, audio-recorded, transcribed verbatim, and analysed qualitatively using content analysis, as described by Graneheim and Lundman. Participants reported that conventional red light photodynamic therapy was very painful during illumination and transiently painful in the post-treatment period, while simulated daylight photodynamic therapy was almost painless during illumination and led to minor post-treatment pain. Also, skin reactions were more intense and longer-lasting with conventional red light photodynamic therapy than with simulated daylight photodynamic therapy. Most participants expressed a treatment preference for simulated daylight photodynamic therapy but had reservations about its unestablished long-term effectiveness. This study underscores the considerable pain associated with conventional red light photodynamic therapy, and the pivotal importance of shared decision-making when selecting the most appropriate treatment.
Key words: interview; actinic keratosis; photodynamic therapy; person-centred care; qualitative research; pain.
SIGNIFICANCE
We conducted semi-structured interviews to document the experiences of patients with actinic keratosis who underwent split-face treatment with conventional red light photodynamic therapy and simulated daylight photodynamic therapy. Participants described more intense, almost unbearable, pain with red light photodynamic therapy as well as longer-lasting skin reactions that interfered with daily life activities. In contrast, simulated daylight photodynamic therapy was described as almost painless, led to fewer, milder skin reactions, and was the preferred treatment modality over red light photodynamic therapy. Participants would prefer simulated daylight photodynamic therapy given long-term effectivenes. Understanding patient experiences during photodynamic therapy can promote person-centred care.
Citation: Acta Derm Venereol 2024; 104: adv19459. DOI https://doi.org/10.2340/actadv.v104.19459.
Copyright: © Published by Medical Journals Sweden, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/)
Submitted: Sep 18, 2023; Accepted: Mar 8, 2024; Published: Apr 10, 2024
Corr: Alexandra Sjöholm, Department of Dermatology and Venereology, Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, SE-413 45 Gothenburg, Sweden. E-mail: alexandra.sjoholm@gu.se
Competing interests and funding: AS has acted as a consultant for Galenica AB, developing patient information leaflets regarding PDT and DL-PDT (2021-2022). AS has also participated in educational activities concerning PDT directed to nurses and dermatology residents (2023). JP, MC, and BH have no conflicts of interest to declare.
INTRODUCTION
Topical photodynamic therapy (PDT) with red visible light, also called conventional PDT (C-PDT), is an effective and widely used treatment for actinic keratosis (AK) (1). As C-PDT is often very painful for patients, several methods have been used to reduce pain during illumination including: cold air (2), nerve blocks (3), infiltration anesthesia (4), and water spray (5). Daylight PDT is a potentially less painful alternative to C-PDT that uses sunlight as a light source; however, it is weather-dependent (6) and requires the patient to tolerate treatment outdoors (6). Illumination devices providing simulated daylight PDT (SDL-PDT) have been developed to overcome these limitations and avoid exposure to harmful ultraviolet radiation (7, 8).
Indoor Lux© (Gerdes Medical AG, Meckenheim, Germany) is a device for SDL-PDT to treat mild to moderate AK. Studies show that this system can be a valid alternative, but only short-term data on effectiveness (3 months) are available (9, 10). Treatment takes place in a controlled setting with 8 ceiling lights generating white light (570–630 nm) directed towards the target skin area (11). We recently published a technical validation study on this specific light source, showing that patient positioning was important to ensure that the targeted skin received adequate illumination (12).
Previous studies on pain perception during illumination with PDT have used quantitative measures such as the numeric rating scale (NRS) (2, 13) and the visual analogue scale (VAS) (2, 14, 15). However, qualitative research on the human experiences during PDT is scarce. To date, only one qualitative study has reported on patient perceptions of C-PDT with and without nerve blocks (16). In the present interview study, we aimed to describe and explore patient pain experiences, skin reactions, and patient treatment preferences of C-PDT and SDL-PDT during illumination and 4 weeks after treatment.
MATERIALS AND METHODS
Study design
This study used qualitative content analysis (17) of semi-structured interviews and was reported according to the consolidated criteria for reporting qualitative research (COREQ) guidelines (18).
Context and intervention
This interview study is part of a larger, single-center, randomized controlled trial (RCT) comparing clinical clearance rates for symmetrically distributed mild to moderate non-pigmented AK with C-PDT and SDL-PDT, conducted at the Department of Dermatology, Sahlgrenska University Hospital, Gothenburg, Sweden (www.researchweb.org project number 264721). For illumination during C-PDT, we used an Actilite® Cl 128 lamp (Galderma Nordic AB, Uppsala, Sweden) emitting red light at 635 ± 9 nm and an overall light dose of 37 J/cm2. SDL-PDT was carried out with the Indoor-Lux© light system (Gerdes Medical AG, Meckenheim, Germany). The intervention consisted of split-face treatment comparing C-PDT with SDL-PDT on opposing anatomical sites (e.g. right and left cheeks). Both treatments were performed on the same day. Before treatment, the area was wiped with chlorhexidine alcohol (5 mg/ml), followed by a light curettage to remove hyperkeratosis before the topical gel Ameluz® (Biofrontera Pharma GmbH, Leverkusen, Germany) containing the prodrug 5-aminolevulinic acid (ALA) was applied. For C-PDT, a light-blocking dressing was placed over the treatment area for 2.5–3 h before illumination, which took approximately 8 minutes. In SDL-PDT, the treatment area was not occluded, and illumination was started within 30 min after the application of topical medication as per European guidelines (1). Before the treatment, the nurse gave patients written and oral information on the expected pain and how to manage the treatment site afterwards. Patients were made aware that pain may persist for up to 10–12 hours after the treatment and were recommended to take paracetamol as needed.
Ethics
This study was designed, implemented, and reported in accordance with the principles of the Declaration of Helsinki. It was approved by the Regional Ethical Review Board in Gothenburg (approval number 729-17, T544-18) and by the Swedish Ethical Review Authority (approval numbers 2020-01775, 2022-01836-02). All participants provided written informed consent prior to inclusion.
Participants
Patients were recruited to the interview study at the time of inclusion in a larger RCT, comparing the effectiveness of C-PDT and SDL-PDT. We intended to interview up to 20 patients, but after having consecutively included and single-interviewed 10 patients, we concluded the enrollment. This decision was based on deeming the depth and breadth of information gathered from the sample as sufficiently comprehensive in addressing the research questions (19). One potential participant faced scheduling issues and was not included, but all invited patients agreed to participate.
The participants received information on the study’s aim verbally as well as through the written patient information and the consent form. Recruitment and treatment were carried out by AS (a female registered nurse and doctoral student trained in qualitative content analysis. AS is experienced in PDT using different light sources). On completion of treatment, all study participants received a diary (Appendix S1) to record their experiences and support recall during the interview, which took place 4 weeks after treatment. The use of the diaries was voluntary.
Data collection
The individual interviews were semi-structured, following an interview guide developed by authors AS and BH (a female qualified nurse and expert in qualitative interview studies and qualitative data analysis). AS tested the interview guide (excluded from the analysis) with a volunteer. The interview guide comprised the topic areas described in Appendix S1. No changes were made following the pilot interview. Between 1 June 2022, and 31 January 2023, AS interviewed each participant once in Swedish. The interviews were audio recorded with an Olympus WS-852 voice recorder (Olympus Corporation, Tokyo, Japan) in a private room at the hospital. No field notes were taken. AS and the participant were alone during the interview, except for one interview with a non-native-speaking participant, who was supported by a relative. The duration of the interviews ranged from 21 to 38 min (median 35 min). At the end of each interview, AS summarized salient interview points to give the participant an opportunity to add details or clarification.
The interviews were transcribed verbatim by AS and a medical secretary with the f4transkript software tool (dr.dressing & pehl GmbH, Marburg, Germany) using a transcription guide (20). To ensure the transcript quality, all audio recordings were compared with the transcripts and any errors were corrected (AS). Transcripts were not returned to participants for comments.
Data analysis
The transcripts were analysed in a manifest qualitative content analysis according to Graneheim and Lundman (17, 21). Data were managed and processed with the software program Atlas.ti (Scientific Software Development GmbH, Berlin, Germany) and Excel spreadsheets (Microsoft Corp, Redmond, WA, USA). To ensure methodological rigor, AS received training in qualitative content analysis before collaborating with BH, MC, and JP to collectively design the study and the interview guide. AS and BH used the pilot interview to develop a coding scheme, a common understanding of the code definitions. AS and BH used deductive (structural) coding using the interview guide to identify all text units that were relevant to answering the research questions. Then, AS and BH conducted iterative cycles of comparing codes and identifying subcategories and categories of manifest content, through the following steps: (i) reading and re-reading the text to become familiar with it (AS, BH); (ii) identifying meaning units (AS); (iii) condensing meaning units (AS); and (iv) coding: abstraction of meaning units (AS, BH). During the coding phase, AS and BH met regularly to discuss the analysis and to solve any discrepancies. The meetings were also used to critically reflect on the potential bias and ethical considerations associated with AS’s dual role as a healthcare professional and researcher. BH has no experience in dermatology and could thus provide a neutral perspective and act as sounding board and challenge preconceived assumptions. Participants did not provide feedback on the findings after the analysis.
Rigor
Demonstrating trustworthiness according to the criteria credibility, transferability, dependability, and confirmability is a hallmark of rigor in qualitative research (22). The authors ensured credibility through all phases of this study by choosing an appropriate study design using interviews to gather in-depth information regarding patient experiences with PDT. Moreover, the team comprised members with extensive clinical and research experience. The sampling of the participants was consecutive, but the participants had been recruited randomly to the intervention group of the overarching RCT. The study benefits from investigator triangulation, i.e. the team consisted of multiple researchers with various professional backgrounds who discussed the findings and their interpretation through their specific lenses, at regular meetings. The participants used diaries to log their experience, which ensured that recall bias concerning their experience was reduced. Finally, the authors provided quotes and detailed (thick) descriptions of the participants’ experiences. While transferability of qualitative research can be problematic, the authors consider the transferability of this study as high because the results regarding the pain experience with the two light sources are unambiguous. However, the authors appreciate that recommendations in favour of SDL-PDT cannot be made because this method is costly and may not be affordable in every setting and context. The authors’ systematic approach to the data analysis, as described by Graneheim and Lundman, ensure the dependability (17, 21). Finally, the results are based on the participants’ narrative, which ensures confirmability of the results. The authors stayed close to the data without deep interpretation (23). AS reflected on the pre-existing relationship with the participants during the interview process. To enable participants to share their experiences openly, she consciously tried to create a safe atmosphere. As a researcher, AS had to be curious about the patient experience and aware of the need to remain open-minded. Through observations during treatment, AS gained detailed insights into the patients’ pain experiences, allowing her to ask targeted questions and explore the treatment journey from the patients’ perspective.
RESULTS
Ten participants (7 men, 3 women) aged 60–81 years were interviewed 4 weeks after treatment with C-PDT and SDL-PDT. The treated locations varied: forehead (n = 6), cheeks (n = 4), temples (n = 4), nose (n = 3), scalp (n = 2), forearms (n = 1), and dorsum of the hand (n = 1), with some participants receiving treatment on multiple sites. In the content analysis of the interviews, we identified 4 main categories and 4 subcategories (Fig. 1), as detailed below.
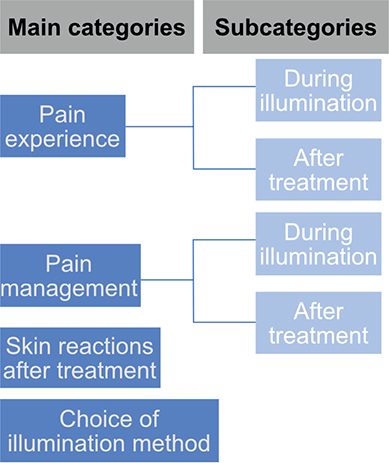
Fig. 1. Main categories and subcategories identified in the content analysis of the interviews.
Pain experience
All participants stated that being cared for, and to be seen, listened to, and well treated were important irrespective of the treatment modality (C-PDT or SDL-PDT). However, depending on the type of illumination administered, participants experienced different pain levels during and after treatment.
Pain experience during illumination
Fewer participants reported a need for healthcare professionals to be physically present in the room during illumination with SDL-PDT relative to C-PDT. Nevertheless, it was important for participants to have staff available nearby to answer potential questions. Some participants expressed no expectations of pain prior to treatment despite having previously received oral and written information. Most participants expected C-PDT to be painful, given that they had experienced prior treatment with C-PDT or cryosurgery. Some participants searched online for further information about PDT.
Despite previous treatment sessions, some participants stated that the pain of C-PDT was surprisingly intense. During illumination with C-PDT, all participants experienced transient pain, and the majority reported having strong pain. The participants described the sensation as “stinging”, “burning”, or “piercing”. Participant 7 declared: “It burned and stung. You could … have heated a small stick, an iron bar, and then driven it into my forehead…. That’s what I felt. It hurt that much. / / It hurt terribly. // It just can’t be described, it…. Torture.”
The quality of the pain was described with quotes like “surprisingly strong”, “nasty”, “terrible”, “worst ever”, and “shocking”. Some felt that the pain was so intense that they were “on the verge of not making it [through the illumination]”. In contrast, participants did not experience any pain during illumination with SDL-PDT and generally expressed that the 2-hour illumination period was comfortable and relaxing. Participant 3 described the illumination period as tedious: “And there were big differences. I mean sitting in a sunroom where you could even sit and read…. It was nothing. Sitting there for 2 hours was just nice”.
Pain experience after treatment
Most participants experienced pain during the first 24 h following treatment and the pain sensation of stinging and itching lasted throughout the first week independent of the illumination method. However, the pain sensation in the area treated with C-PDT remained during the first week while it diminished in the area treated with SDL-PDT. The quality of the pain perceived in the skin areas treated with C-PDT and SDL-PDT is summarized in Table I.
Pain management
C-PDT required the participants to employ active pain management strategies during illumination, while SDL-PDT did not. Nonetheless, both treatment modalities resulted in skin reactions that warranted some degree of pain management post-treatment.
Managing pain during illumination
During illumination with C-PDT, the majority used mental distraction to try to endure the pain throughout illumination and then to try and move on from the experience. One respondent required short illumination pauses during the treatment. Eight participants accepted water spray provided by the nurse during illumination, which relieved the pain for 5 of them. One respondent (Participant 5) prematurely interrupted illumination with C-PDT after one short pause, explaining: “I tried to concentrate and count and see how long I could endure it, but in the end it hurt so much.”
In contrast, the absence of pain during the SDL-PDT illumination allowed the participants to try and focus on something pleasant as they waited 2 hours, for example by reading, relaxing, talking to another patient, or having a coffee. Participant 10 said: “Then I sat there reading and had a good time. // Mm (affirmative) // (laughs). No, it went very smoothly.”
Managing pain after treatment
Irrespective of treatment modality, the majority of participants adhered to the recommendations to take paracetamol as needed to alleviate pain after treatment. Some participants reported various other strategies to manage pain after treatment including cold air, wet cold towels applied to the treatment area, rinsing with cold water, and even mentally enduring the pain and “simply trusting the medical professionals”.
Skin reactions after treatment
Participants described experiencing skin reactions after C-PDT, which were more intense and had a longer duration of crusting, redness, and swelling compared with those caused by SDL-PDT. Moreover, participants reported that their skin surface without visible AK was also more scaly and red in the area treated with C-PDT as compared with SDL-PDT. Participants also expressed that it took longer for all crusts to disappear from the C-PDT-treated areas. Several participants were retired and had reduced social contact, but most participants reported some influence of skin reactions on their daily social lives. It was common for participants to avoid social contacts for a few days after treatment due to soreness, scaling, and redness. Nevertheless, one respondent attended social dancing and had dinner with friends the day after the treatment.
Choice of illumination method
Almost all (9 of 10) participants preferred illumination with SDL-PDT over C-PDT. However, participants had reservations regarding their preference given that the long-term effectiveness of SDL-PDT versus C-PDT has not been established. Five participants expressed that they would prefer 2 treatments with SDL-PDT rather than 1 treatment with C-PDT, if SDL-PDT was found to be less effective than C-PDT but could be repeated to achieve similar effectiveness. One participant stated their preference might change depending on which anatomical location was being treated.
DISCUSSION
This study explores patient pain experiences in C-PDT and SDL-PDT treatments for mild to moderate non-pigmented AK. Our findings show that C-PDT’s illumination phase is very painful, lasting days post-treatment. Consequently, participants employed distraction techniques and other pain relief methods to cope with the discomfort. SDL-PDT illumination, on the other hand, is almost pain-free with milder skin reactions and quicker healing. Most participants preferred SDL-PDT, though some were concerned about its long-term effectiveness.
The majority of participants were treated in the head and neck region, where C-PDT is most painful (24). In line with other research, participants experienced that cold water spray and pauses during illumination could reduce pain during C-PDT (5) and they reported that mental distraction was important for pain management. Previous research has shown that mental distraction, for example listening to music, can reduce pain intensity (25). Participants also used pain management strategies in the hours and days after treatment, including painkillers and wet cold facecloths. Such strategies have also been described elsewhere (26). Pain during SDL-PDT was barely an issue for the interviewed participants as observed in an earlier prospective study on SDL-PDT for AK (9). We are not aware of studies describing skin reactions after SDL-PDT, but intense skin reactions to C-PDT were consistent with previous findings (16, 26).
The majority of study participants preferred SDL-PDT to C-PDT. Half of them would have preferred 2 sessions with SDL-PDT if needed to achieve similar effectiveness to C-PDT. A previous discrete choice experiment to elicit patient preferences on topical treatments for AK showed that patients may reject a treatment if the negative experiences outweigh the expected therapeutic benefits (27).
Strength and limitations
This study explored patient experiences, which is important but rarely investigated. Furthermore, interviews had standardized timing after 4 weeks and participants used treatment diaries to ensure recall. The diaries also enabled participants to describe complex issues that cannot be captured on a simple numerical pain severity scale like VAS. However, the diaries were not analysed, something that could be regarded as a limitation. We abstained from including these as data sources because participants might have withheld writing entries they desired to keep concealed. Another limitation is that the interviewer was the same person who treated the participants. Moreover, both C-PDT and SDL-PDT were performed on the same day, always starting with SDL-PDT, which may have made it difficult for participants to differentiate between the pain perceived during and after illumination. As the interview study was part of a larger prospective RCT, the study protocol did not allow for treatments to be performed on separate occasions. To validate our results, patient interviews could be replicated with new participants ensuring a time gap between the two PDT sessions. The participants were also of a relatively small age range (60–81 years), which is, however, typical for patients receiving PDT for AK (9, 28, 29). Finally, we did not seek participants’ feedback on the results. However, the main focus of this enquiry was on the patients’ experience of pain, and those results were unambiguous.
The clinical implications from this study underscore the importance of deciding together with the patient which PDT treatment, the painful C-PDT or the pain-free SDL-PDT, is suitable for a particular person, provided both options are available. A recent consensus statement recommended that “patient perspective on effectiveness” and “patient-reported future treatment preference” should be reported in all AK treatment studies, but did not indicate guidance on how to standardize measurement or handle the outcomes (30). Qualitative research is one way to report the patient’s perspective on C-PDT and SDL-PDT. Finally, nurses may play an important role in the treatment decision-making process as they are centrally involved in treatment implementation evaluation and safety (26). However, to date, there are no national or international guidelines for advising patients on post-treatment self-care after PDT.
ACKNOWLEDGEMENTS
The authors would like to thank Gabriella Lisengård, medical secretary at the Department of Dermatology and Venereology, Sahlgrenska University Hospital, for providing help with transcribing some of the interviews. They would also like to thank Nesrin Vurgun, scientific editor, Institute of Clinical Sciences at Sahlgrenska Academy at University of Gothenburg, for carefully proofreading the manuscript.
Funding sources: AS and JP were supported by a grant from the Swedish state under the agreement between the Swedish government and the county councils, the ALF agreement (ALFGBG-728261). MC was supported by a research fellowship (ALFGBG-942629) from the Swedish state under the agreement between the Swedish government and the county councils, the ALF agreement. BH had no external funding.
IRB approval status: The Regional Ethical Review Board in Gothenburg (Approval number 729-17, T544-18) and the Swedish Ethical Review Authority (Approval numbers 2020-01775 and 2022-01836-02).
REFERENCES
- Morton CA, Szeimies RM, Basset-Seguin N, Calzavara-Pinton P, Gilaberte Y, Haedersdal M, et al. European Dermatology Forum guidelines on topical photodynamic therapy 2019 Part 1: treatment delivery and established indications – actinic keratoses, Bowen’s disease and basal cell carcinomas. J Eur Acad Dermatol Venereol 2019; 33: 2225–2238.
- Stangeland KZ, Kroon S. Cold air analgesia as pain reduction during photodynamic therapy of actinic keratoses. J Eur Acad Dermatol Venereol 2012; 26: 849–854.
- Halldin CB, Paoli J, Sandberg C, Gonzalez H, Wennberg AM. Nerve blocks enable adequate pain relief during topical photodynamic therapy of field cancerization on the forehead and scalp. Br J Dermatol 2009; 160: 795–800.
- Borelli C, Herzinger T, Merk K, Berking C, Kunte C, Plewig G, et al. Effect of subcutaneous infiltration anesthesia on pain in photodynamic therapy: a controlled open pilot trial. Dermatol Surg 2007; 33: 314–318.
- Wiegell SR, Haedersdal M, Wulf HC. Cold water and pauses in illumination reduces pain during photodynamic therapy: a randomized clinical study. Acta Derm Venereol 2009; 89: 145–149.
- Wiegell SR, Wulf HC, Szeimies RM, Basset-Seguin N, Bissonnette R, Gerritsen MJ, et al. Daylight photodynamic therapy for actinic keratosis: an international consensus: International Society for Photodynamic Therapy in Dermatology. J Eur Acad Dermatol Venereol 2012; 26: 673–679.
- O’Mahoney P, Haigh N, Wood K, Brown CTA, Ibbotson S, Eadie E. A novel light source with tuneable uniformity of light distribution for artificial daylight photodynamic therapy. Photodiagnosis Photodyn Ther 2018; 23: 144–150.
- O’Gorman SM, Clowry J, Manley M, McCavana J, Gray L, Kavanagh A, et al. Artificial white light vs daylight photodynamic therapy for actinic keratoses: a randomized clinical trial. JAMA Dermatol 2016; 152: 638–644.
- Bai-Habelski JC, Medrano K, Palacio A, Reinhold U. No room for pain: a prospective study showing effective and nearly pain-free treatment of actinic keratosis with simulated daylight photodynamic therapy (SDL-PDT) using the IndoorLux® System in combination with BF-200 ALA (Ameluz®). Photodiagnosis Photodyn Ther 2022; 37: 102692.
- Kellner C, Bauriedl S, Hollstein S, Reinhold U. Simulated-daylight photodynamic therapy with BF-200 aminolaevulinic acid for actinic keratosis: assessment of the efficacy and tolerability in a retrospective study. Br J Dermatol 2015; 172: 1146–1148.
- Gerdes Medical AG. A new concept: simulated daylight PDT (SDL-PDT) with IndoorLux©. [cited 2023 December 12]. Available from: https://gerdesmedical.de/#concept.
- Sjöholm A, Claeson M, Paoli J. Measurements of illuminance in simulated daylight photodynamic therapy. Photodermatol Photoimmunol Photomed 2022; 38: 564–570.
- Arits AH, van de Weert MM, Nelemans PJ, Kelleners-Smeets NW. Pain during topical photodynamic therapy: uncomfortable and unpredictable. J Eur Acad Dermatol Venereol 2010; 24: 1452–1457.
- Sandberg C, Stenquist B, Rosdahl I, Ros AM, Synnerstad I, Karlsson M, et al. Important factors for pain during photodynamic therapy for actinic keratosis. Acta Derm Venereol 2006; 86: 404–408.
- Gholam P, Denk K, Sehr T, Enk A, Hartmann M. Factors influencing pain intensity during topical photodynamic therapy of complete cosmetic units for actinic keratoses. J Am Acad Dermatol 2010; 63: 213–218.
- Halldin CB, Gonzalez H, Wennberg AM, Lepp M. Patients’ experiences of pain and pain relief during photodynamic therapy on actinic keratoses: an interview study. Acta Derm Venereol 2013; 93: 433–437.
- Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today 2004; 24: 105–112.
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007; 19: 349–357.
- Sandelowski M. Sample size in qualitative research. Res Nurs Health 1995; 18: 179–183.
- Dresing TP, Thorsten/Schmieder, Christian Manual (on) Transcription. Transcription conventions, software guides and practical hints for qualitative researchers. 3rd English ed. online] 2015 [cited 2023 April 1]. Available from: https://www.audiotranskription.de/wp-content/uploads/2020/11/manual-on-transcription.pdf.
- Lindgren BM, Lundman B, Graneheim UH. Abstraction and interpretation during the qualitative content analysis process. Int J Nurs Stud 2020; 108: 103632.
- Shenton AK. Strategies for ensuring trustworthiness in qualitative research projects. Education for Information 2004; 22: 63–75.
- Sandelowski M. Whatever happened to qualitative description? Res Nurs Health 2000; 23: 334–340.
- Halldin CB, Gillstedt M, Paoli J, Wennberg AM, Gonzalez H. Predictors of pain associated with photodynamic therapy: a retrospective study of 658 treatments. Acta Derm Venereol 2011; 91: 545–551.
- Nguyen TN, Nilsson S, Hellström AL, Bengtson A. Music therapy to reduce pain and anxiety in children with cancer undergoing lumbar puncture: a randomized clinical trial. J Pediatr Oncol Nurs 2010; 27: 146–155.
- Harvie SE. Aminolevulinic acid and photodynamic combination therapy in the treatment of actinic keratoses: caring for the patient. Dermatol Nurs 2007; 19: 31–39.
- Kopasker D, Kwiatkowski A, Matin RN, Harwood CA, Ismail F, Lear JT, et al. Patient preferences for topical treatment of actinic keratoses: a discrete-choice experiment. Br J Dermatol 2019; 180: 902–909.
- George CD, Tokez S, Hollestein L, Pardo LM, Keurentjes AJ, Wakkee M, et al. Longitudinal assessment of the prevalence of actinic keratosis and extensive risk factor evaluation: an update from the Rotterdam Study. J Invest Dermatol 2023; 143: 2193–2203.e12.
- Lacour JP, Ulrich C, Gilaberte Y, Von Felbert V, Basset-Seguin N, Dreno B, et al. Daylight photodynamic therapy with methyl aminolevulinate cream is effective and nearly painless in treating actinic keratoses: a randomised, investigator-blinded, controlled, phase III study throughout Europe. J Eur Acad Dermatol Venereol 2015; 29: 2342–2348.
- Reynolds KA, Schlessinger DI, Vasic J, Iyengar S, Qaseem Y, Behshad R, et al. Core outcome set for actinic keratosis clinical trials. JAMA Dermatol 2020; 156: 326–333.