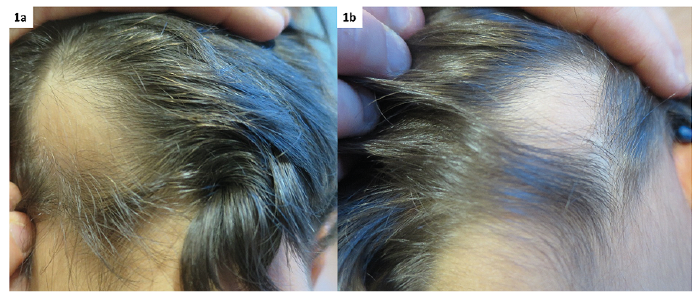
Fig. 1. Bald smooth skin colour area. (a) Right occipital, (b) left occipital.
1Pediatric Dermatology Unit, Departments of Dermatology & Venereology, and 2Pediatrics, University Hospital Lausanne, University of Lausanne, Chemin de Montétan 16, CH-1004 Lausanne, Switzerland. E-mail: stephanie.christen@chuv.ch
A 6-year-old boy presented at our clinic with bilateral alopecia. The parents had noticed persistent, bilateral areas of alopecia covering a flat skin-coloured, subcutaneous nodule on the back of his head at the age of 3 months. His developmental evaluation was normal. The occipital nodules had grown progressively with the child, were soft on palpation, and covered with fuzzy hair (Fig. 1). No other skin lesion was noticed. Ultrasound examination revealed a poorly defined lipomatous thickening of the subcutaneous tissues. Histopathology revealed hypotrichosis with decreased anagen hair and immature hair follicles (Fig. 2a) overlying an abundant fatty tissue and isolated arrector pili muscle (Fig. 2b). Magnetic resonance imaging (MRI) of the head and brain confirmed the presence of bilateral, excessive subcutaneous fatty tissue of the occipital areas, but no cerebral abnormalities (Fig. 3).
What is your diagnosis? See next page for answer.
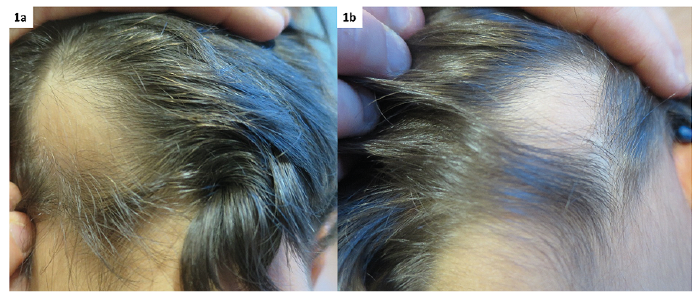
Fig. 1. Bald smooth skin colour area. (a) Right occipital, (b) left occipital.
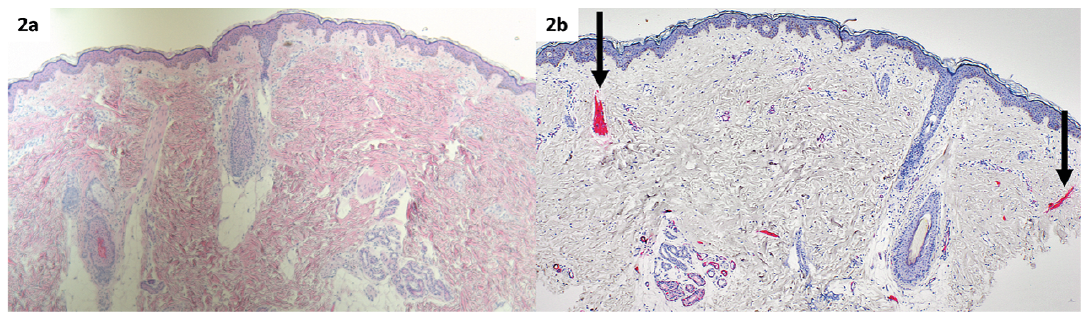
Fig. 2. (a) Haematoxylin and eosin staining (HES) ×40: decreased hair follicles surrounded by fatty tissue and absence of mature hair follicles. (b) Immunohistochemistry (IHC) smooth-muscle actin ×40, arrows: isolated arrector pili muscles.
Fig. 3. Cerebral magnetic resonance imaging (MRI), arrows: excess of subcutaneous fatty tissue.
Acta Derm Venereol 2020; 100: adv00104.
Diagnosis: Bilateral occipital naevus psiloliparus with-out encephalo-cranio-cutaneous lipomatosis
Naevus psiloliparus (NP) was first described by Happle & Küster in 1998 as a fatty tissue naevus (1). Clinically it presents as a flat patch with smooth surface and absence of, or few, hair follicles on the scalp. Histopathologically it is characterized by excess of fatty tissue associated with an absence or few hair follicles and isolated arrector pili muscles (1). It has to be differentiated from naevus lipomatosus superficialis, which has an irregular surface, rarely associated with hypotrichosis, usually located on the trunk or thighs (1). So far, only one paediatric case of naevus lipomatosus superficialis of the scalp has been published (2), prior to Happle’s description of NP.
It has long been postulated that NP is a pathognomonic sign for encephalo-cranio-cutaneous lipomatosis (ECCL). ECCL is a syndrome associating skin, ocular and central nervous system anomalies. However, 2 cases of isolated unilateral NP were published in 2004 (3). It was notable that the 2 girls did not have any cerebral imaging. In 2009, a review of 54 patients with ECCL showed that only 44 of them had a NP, 12 of them bilateral. In this review, 53/54 patients had dermatological signs. The other dermatological signs associated with ECCL were: patchy or linear alopecia without fatty tissue (sometimes resulting from focal skin aplasia), subcutaneous lipoma in fronto-temporal region and small nodular skin tags on the eyelids or following a line from the outer canthus to tragus (4). To the best of our knowledge, this is the first case of bilateral NP without ECCL. It is obvious that in patient with a NP, ECCL has to be excluded by brain imaging. NP is, however, not considered pathognomonic for ECCL.