SHORT COMMUNICATION
Treatment of Vulvar Angiolymphoid Hyperplasia with Eosinophilia with Topical Corticosteroids
Nor FAZIL JABER1, Britta KRYNITZ2,3 and Philip CURMAN1,4,5*
1Dermato-Venereology Clinic, Karolinska University Hospital, Eugeniavägen 3, SE-171 64 Stockholm, 2Division of Pathology, Department of Oncology-Pathology (Solna), Karolinska Institutet, 3Department of Pathology and Cancer Diagnostics (Solna), Karolinska University Laboratories, 4Dermatology and Venereology Division, Department of Medicine (Solna), Karolinska Institutet, and 5Department of Medical Epidemiology and Biostatistics, Karolinska Institutet, Stockholm, Sweden. *E-mail: philip.curman@ki.se
Citation: Acta Derm Venereol 2023; 103: adv19659. DOI https://doi.org/10.2340/actadv.v103.19659.
Copyright: © Published by Medical Journals Sweden, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution International License (https://creativecommons.org/licenses/by/4.0/)
Accepted: Oct 24, 2023; Published: Nov 20, 2023
Competing interests and funding: The authors have no conflicts of interest to declare.
INTRODUCTION
Angiolymphoid hyperplasia with eosinophilia (ALHE), a rare, benign vasoproliferative disease, typically presents clinically as single or multiple, intradermal or subcutaneous papules or nodules, purple-pink in colour (1, 2). We report here an uncommon clinical presentation of ALHE, mimicking clinically subcutaneous lipomatous masses in the vulva, which was ultimately treated successfully with topical corticosteroids. The aim of this report is to raise awareness of this rare disorder, which potentially greatly impairs the quality of life of affected individuals, especially when located on the vulva.
CASE REPORT
A 21-year-old nulligravida woman with a history of polycystic ovary syndrom, type 1 diabetes, and anxiety, presented to the Dermatology Department, Karolinska University Hospital (Stockholm, Sweden) with a 10-year history of pruritus and recurrent swollen papular lesions in the vulva. The lesions ranged in size between 2 and 5 mm and located superiorly on both the labia minora and majora (Fig. 1A). These would bleed, ulcerate, and periodically reappear several times monthly, with individual lesions lasting for several weeks. Treatment attempts with emollients and fluconazole tablets were unsuccessful. The vagina and cervix appeared normal. Tests for herpes, chlamydia, and gonorrhea were negative. Several inconclusive histopathological examinations had been performed during the previous years. Reassessment revealed an increased presence of small, partially dilated capillaries with plump endothelium surrounded by a superficial and deep intradermal mixed infiltrate with numerous eosinophils (Fig. 2A). Ample vessels were visualized with erythroblast transformation-specific regulated gene-1 (ERG) nuclear staining antibody (Fig. 2B). A diagnosis of ALHE was assigned based on both the histopathological and clinical appearance. Unexpectedly, only 3 weeks after commencing treatment with group II topical corticosteroids complete remission was seen, lasting for at least 6 months on follow-up (Fig. 1B).
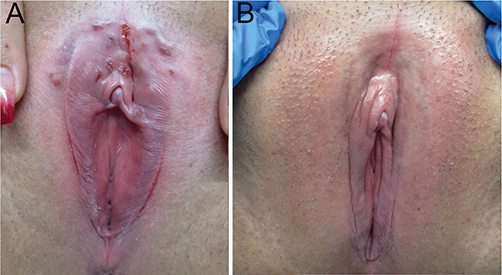
Fig. 1. Clinical photographs. (A) Clinical picture before treatment showing numerous papules, nodules, and fissures. (B) Complete clinical remission following treatment with topical corticosteroid.
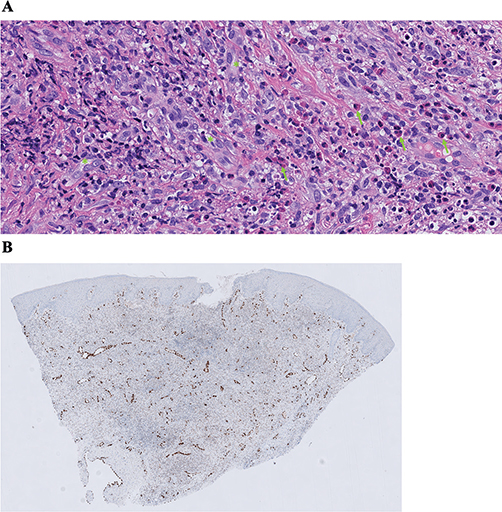
Fig. 2. Histopathology. (A) Haematoxylin and eosin stain, showing multiple vessels with plump, epithelioid endothelium (green asterisks) and an eosinophil-rich infiltrate (green arrows). Original magnification 40×. (B) Immune histochemistry marker erythroblast transformation specific regulated gene-1 (ERG), nuclear staining of endothelium, highlighting the well vascularized stroma. Original magnification 4×.
DISCUSSION
This report describes the third known case of ALHE with vulvar engagement (3, 4), treated successfully with topical corticosteroids. Being an exceedingly rare, benign, and idiopathic vasoproliferative skin condition, a combination of clinical and histopathological features is required for accurate diagnosis. The lesions are predominantly located in the head and neck region, and rarely on the trunk, extremities, or oral mucosa (1, 2). Young adults most frequently develop ALHE, but all ethnicities and age groups can be affected. Due to the vascular nature of the lesions, tenderness, pulsation, pruritus, or bleeding may occur in some patients (1, 5). Histologically, the characteristic features are proliferation of blood vessels lined by plump endothelial cells, admixed with a dense inflammatory infiltrate rich in eosinophils and lymphocytes (1).
The pathogenesis of ALHE is still debated. Several reports have shown an association to trauma, pregnancy, infection, and arteriovenous shunting (1–3). Histologically, ALHE may be differentiated from other vascular neoplasms, such as angiokeratomas and atypical vascular lesions, as well as inflammatory and infectious diseases, such as granulomatous lesions, adenoid hyperplasia, and eosinophilic histiocytosis or granuloma of the vulva.
Many treatments, including surgery, pulsed-dye laser, carbon dioxide laser, cryosurgery, topical imiquimod, tacrolimus, isotretinoin, and intralesional corticosteroids have been reported (1). Surgical excision is considered the treatment of choice and when completely excised, individual lesions rarely recur. One-third of incompletely excised lesions recur, typically along the course of the affected vessel (1, 3). However, because of the oftentimes numerous and chronically recurring nature of the lesions, complete excision may be unfeasible. In the current case, topical therapy was preferred because of multiple, scattered, and recurring lesions, and only 3 weeks after commencing treatment with group II topical corticosteroids complete remission was seen.
The diagnostic difficulty and importance in recognizing ALHE as a differential diagnosis when faced with unspecific genital dermatoses is illustrated in the long-standing duration of this case. Early suspicion, thorough diagnostic evaluation including histopathology, and timely initiation of treatment is crucial in ensuring optimal patient outcomes and improving the management of this rare, chronic, and debilitating condition.
REFERENCES
- Guo R, Gavino AC. Angiolymphoid hyperplasia with eosinophilia. Arch Pathol Lab Med 2015; 139: 683–686.
- Olsen TG, Helwig EB. Angiolymphoid hyperplasia with eosinophilia. A clinicopathologic study of 116 patients. J Am Acad Dermatol 1985; 12: 781–796.
- Scurry J, Dennerstein G, Brenan J. Angiolymphoid hyperplasia with eosinophilia of the vulva. Aust N Z J Obstet Gynaecol 1995; 35: 347–348.
- Aguilar A, Ambrojo P, Requena L, Olmos L, Sánchez Yus E. Angiolymphoid hyperplasia with eosinophilia limited to the vulva. Clin Exp Dermatol 1990; 15: 65–67.
- Wells GC, Whimster IW. Subcutaneous angiolymphoid hyperplasia with eosinophilia. Br J Dermatol 1969; 81: 1–15.