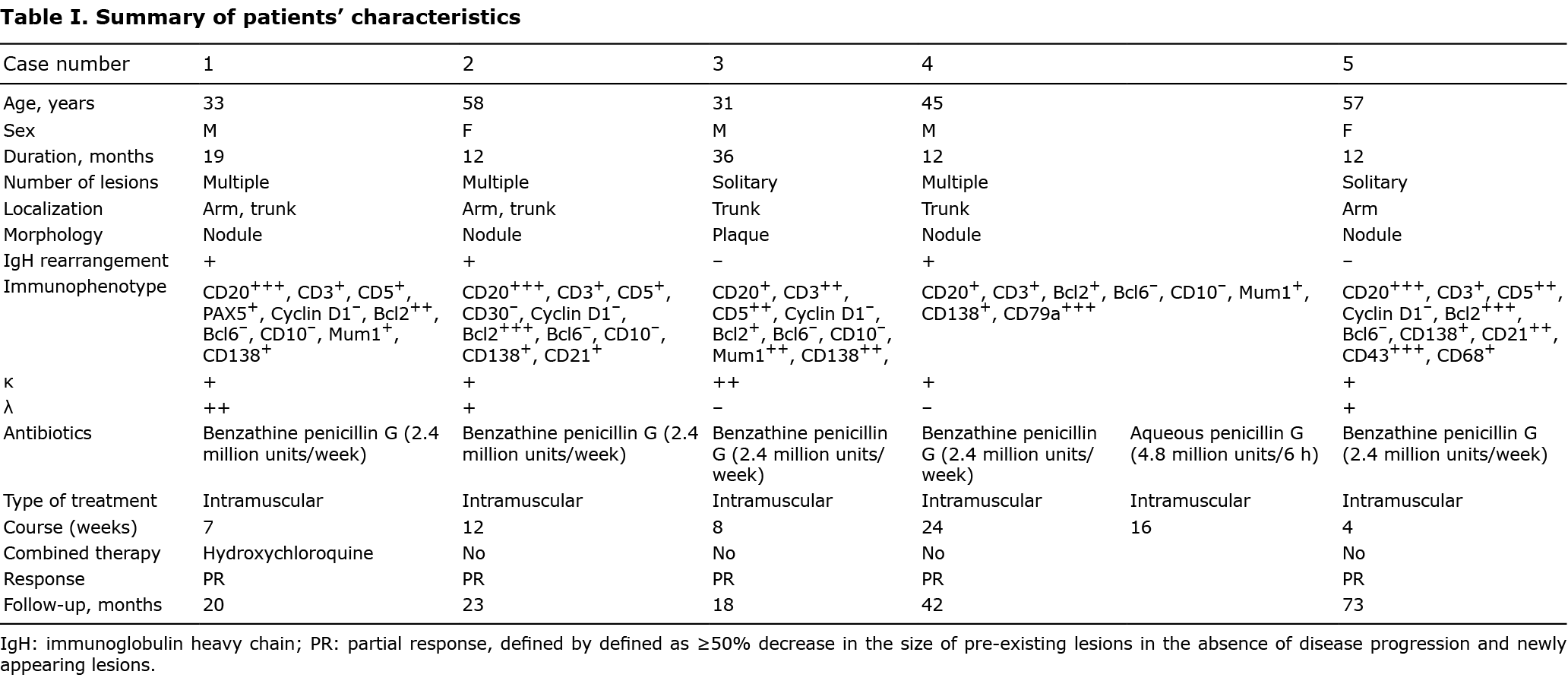
Primary cutaneous marginal zone lymphoma (PCMZL) is the most common type of cutaneous B cell lymphoma (CBCL) with an indolent clinical course (1). Despite a favourable prognosis and good initial treatment response, clinical relapse is common, especially in patients with multiple lesions (1). Although a relationship between Borrelia burgdorferi (Bb) and PCMZL is not conclusive, antibiotics have been suggested for treatment of Bb-positive patients with PCMZL, and have shown variable efficacy (1). This study retrospectively reviewed 705 patients from the skin lymphoma cohort in our department between January 2012 and August 2020. Six patients with Bb-negative PCMZL were found, 5 of whom had been treated with systemic benzathine penicillin G, all of whom achieved remarkable and durable response. Detailed patient information is listed in Table I.
CASE REPORTS
Case 1. A 33-year-old man presented with multiple red nodules, 1–2 cm in diameter on his upper extremities and back for 19 months. Oral hydroxychloroquine resulted in decreased numbers of skin nodules, but the condition soon progressed. Skin biopsy confirmed a diagnosis of PCMZL. Weekly intramuscular benzathine penicillin, 2.4 million IU, was initiated for 7 weeks, and the skin nodules showed markedly reduced size and number. He continued oral hydroxychloroquine for 1.5 years. The disease remained stable.
Case 2. A 58-year-old woman with PCMZL, manifesting with multiple dark-red nodules, 1–2 cm in size on her left arm and back with severe pruritus for 1 year (Fig. 1a). Intramuscular benzathine penicillin was initiated as first-line therapy for 3 months. The skin nodules began to regress remarkably from the first month and partial response was achieved at 3 months (Fig. 1b). Maintenance treatment included oral hydroxychloroquine in combination with thalidomide for 2 weeks, and then with methotrexate for 14 months. She achieved complete regression without relapse during follow-up.

Case 3. A man in his 30s with a 1.5-cm solitary red plaque on his back, diagnosed as PCMZL nearly 3 years previously (Fig. 1c). The skin lesion regressed gradually after 2 months’ intramuscular benzathine penicillin, followed by complete disappearance of the plaque after oral thalidomide for 2 months (Fig. 1d). No local recurrence occurred during 18 months’ follow-up.
Case 4. A 45-year-old male with multiple purplish-red nodules, 2–3 cm in diameter on the back for 1 year, was diagnosed with PCMZL. He received intramuscular aqueous penicillin G for 1 month. Clinical response occurred as early as 2 weeks, and some nodules regressed. Benzathine penicillin was then initiated for 6 months, and most nodules subsided. The remaining skin nodules were treated with oral hydroxychloroquine, intralesional betamethasone, and surgical excision, and complete response was achieved without recurrence during 3.5-years’ follow-up.
Case 5. A 57-year-old woman presented with a solitary egg-sized nodule on her arm for 1 year. The histology features and the immunophenotype of this patient were highly consistent with the diagnosis of PCMZL. However, the IGH and IGK gene arrangements showed polyclonal results. She was treated with benzathine penicillin for 4 months. The skin nodule gradually subsided and atrophied. Oral hydroxychloroquine, low-dose thalidomide, and methotrexate were used for 1 year. The disease achieved a partial response without progression during 6 years’ follow-up.
DISCUSSION
Collectively, all 5 patients experienced rapid and substantial improvements upon penicillin treatment, with duration from 4 to 24 weeks, although the single agent did not achieve a complete response. PCR analyses of Bb DNA on paraffin-embedded tissue sections of all 5 cases were negative (Fig. 1e). The serology of Bb was not investigated.
Responses to antibiotics in patients with PCMZL have been reported previously in the literature. The current review analysed 15 articles, with a total of 30 cases of PCMZL treated with antibiotics, ranging from 1997 to 2020 (2–8). Their characteristics are shown in Table SI. Most patients came from Europe, except for 3 patients, who were American. At least 11 out of 30 patients were prescribed doxycycline. The overall response rate to antibiotics was 40% (12/30), and complete response rate was 23.3% (7/30). Four out of 17 (23.5%) Bb-negative patients responded to antibiotics, which was even lower. The only patient who was treated with penicillin was Bb-positive, but underwent disease progression. Overall, antibiotics showed considerable efficacy. But for Bb-negative PCMZL, the response rate was low. Two possible reasons are suggested: firstly, most patients were treated with antibiotics for not more than 1 month. Treatment duration was prolonged appropriately, mainly in accordance with disease severity and observed promising outcomes. Secondly, ceftriaxone and doxycycline were the most commonly used antibiotics, while the role of penicillin has been ignored.
Penicillin is a common, safe β-lactam antibiotic. β-lactam derivatives have been shown to inhibit the proliferation of cancerous B lymphocytes by inducing apoptosis (9). Penicillin has demonstrated a concentration-dependent, antiproliferative effect on human bone marrow cells and mouse B-cell lymphoma BCL-1 cells in vitro (10, 11). These findings support the anti-lymphoma efficacy of penicillin seen in the current patients. Meanwhile, the risk of developing penicillin-resistant strains after weeks or months of antibiotic therapy should be taken into consideration. In addition, a previous study showed that hydroxychloroquine had antineoplastic effects and was a safe and fast-acting drug for localized low-grade B-cell lymphomas (12). Hydroxychloroquine is a commonly used drug for PCMZL in our department. In conclusion, the findings of this study suggest that a prolonged course of penicillin can be a cost-effective first-line therapy for patients with Bb-negative PCMZL.
The authors have no conflicts of interest to declare.
REFERENCES
- Hristov AC, Tejasvi T, Wilcox RA. Cutaneous B-cell lymphomas: 2021 update on diagnosis, risk-stratification, and management. Am J Hematol 2020; 95: 1209–1213.
- Ponzoni M, Ferreri AJM, Mappa S, Pasini E, Govi S, Facchetti F, et al. Prevalence of Borrelia burgdorferi infection in a series of 98 primary cutaneous lymphomas. Oncologist 2011; 16: 1582–1588.
- Monari P, Farisoglio C, Calzavara Pinton PG. Borrelia burgdorferi-associated primary cutaneous marginal-zone B-cell lymphoma: a case report. Dermatology 2007; 215: 229–232.
- Yildirim FE, Karaduman A, Hürmüz P, Ozyar E, Barişta I, Sağlam A. Symmetrical primary cutaneous marginal zone lymphoma associated with rheumatoid arthritis. J Cutan Pathol 2010; 37: 600–604.
- Ghatalia P, Porter J, Wroblewski D, Carlson JA. Primary cutaneous marginal zone lymphoma associated with juxta-articular fibrotic nodules in a teenager. J Cutan Pathol 2013; 40: 477–484.
- Bonin S, Stinco G, Patriarca MM, Trevisini S, di Meo N, Trevisan G. Could co-infection with anaplasma play a role in Borrelia-associated primary cutaneous marginal zone B-cell lymphomas? Indian J Dermatol Venereol Leprol 2016; 82: 81–84.
- Jothishankar B, Di Raimondo C, Mueller L, Zain J, Parekh V, Abdulla F. Primary cutaneous marginal zone lymphoma treated with doxycycline in a pediatric patient. Pediatr Dermatol 2020; 37: 759–761.
- Golling P, Cozzio A, Dummer R, French L, Kempf W. Primary cutaneous B-cell lymphomas – clinicopathological, prognostic and therapeutic characterisation of 54 cases according to the WHO-EORTC classification and the ISCL/EORTC TNM classification system for primary cutaneous lymphomas other than mycosis fungoides and Sezary syndrome. Leuk Lymphoma 2008; 49: 1094–1103.
- Pirahmadi N, Zarghi A, Salimi A, Arefi H, Pourahmad J. β-lactam Structured, 4-(4-(Methylsulfonyl)phenyl)-1-pentyl-3-phenoxyazetidin-2-one: Selectively Targets Cancerous B Lymphocyte Mitochondria. Anticancer Agents Med Chem 2017; 17: 1292–1301.
- Kuhlmann I. The prophylactic use of antibiotics in cell culture. Cytotechnology 1995; 19: 95–105.
- Neftel KA, Müller MR, Widmer U, Hügin AW. Beta-lactam antibiotics inhibit human in vitro granulopoiesis and proliferation of some other cell types. Cell Biol Toxicol 1986; 2: 513–521.
- Lim M, Bradshaw S, Kirchhof MG. Primary cutaneous low-grade B-cell lymphoma treated with hydroxychloroquine. JAAD Case Rep 2020; 6: 1048–1050.