Diffuse Pruritic Papular and Nodular Skin Eruption in a Febrile Farmer: A Quiz
Mattia Fabio Molle1, Astrid Herzum1, Emanuele Cozzani1*, Marco Mora2 and Aurora Parodi1
1Department of Dermatology, Di.S.Sal., University of Genoa, San Martino Polyclinic Hospital IRCCS, Largo Rosanna Benzi 10, IT-16132 Genoa and 2Division of Pathology, AOU Policlinico San Martino, Genoa, Italy. *E-mail: emanuele.cozzani@unige.it
A 57-year-old Caucasian male farmer was admitted to our hospital with mild fever (37.5°C) lasting more than 10 days, combined with intense asthenia and fatigue while walking.
He presented with oedematous, erythematous swelling of the right ankle, resulting from traumatic local injury occurring in recent weeks, and a subsequently developed mildly pruritic, macular-papular cutaneous rash, generalized to the trunk, root of the limbs and neck, which was only just confluent (Fig. 1). He reported being in contact with cattle and sheep as a farmer, but did not report insect bites.

His medical history was unremarkable for notable pathologies. Blood tests revealed leukopaenia (0.03×109/l) with lymphocytopaenia (0.02×109/l) and neutropaenia (0×109/l) and normocytic anaemia (mean corpuscular volume (MCV) 81.3 fL; Hb 79 g/l), with low red blood cells count (2.7×1012/l) and elevation of serum levels of acute phase reactants of inflammation (C-reactive protein 502 mg/l; procalcitonin 73.60 µg/l; lactic dehydrogenase 492 U/l; D-dimer 5815.0 µg/l), gamma-glutamyltranspeptidase (83 U/l) and aspartate transaminase (54 U/l). Serology for HIV, hepatitis C virus (HCV), hepatitis B virus (HBV) and Epstein-Barr virus (EBV) infection was negative.
A total-body computed tomography (CT) scan revealed multiple lymphadenopathies in the lateral cervical, submandibular, hilar, mediastinal, peri-aortic and aorto-caval areas.
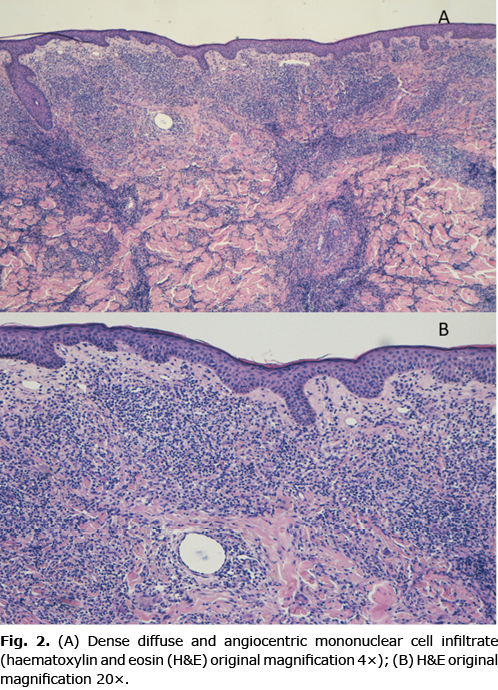
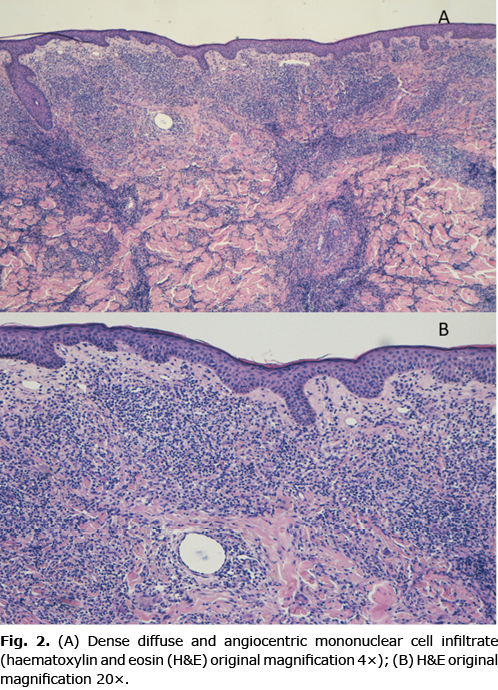
A biopsy specimen from the border of one trunk lesion was therefore performed. The histological findings are shown in Fig. 2.
What is your diagnosis? See next page for answer.
Diffuse Pruritic Papular and Nodular Skin Eruption in a Febrile Farmer: A Commentary
Acta Derm Venereol 2022; 102: adv00716.
DOI: 10.2340/actadv.v102.1996
Diagnosis: Leukaemia cutis
Leukaemia cutis (LC) defines an extramedullary cutaneous localization of leukaemic cells derived from a haematopoietic malignancy, namely leukaemia (1, 2). During leukaemia, after an initial phase of generalization in the bone marrow, leukaemic cells appear in the peripheral blood, and various organs may be infiltrated by extramedullary leukaemic cells (1). LC is a rare skin condition and no extensive epidemiological studies are available for LC. Nonetheless, it appears that acute myeloid leukaemia (AML) is the type of leukaemia most frequently associated with cutaneous localizations (1). Skin manifestations typically occur in patients who have already been diagnosed with leukaemia, following the onset of systemic symptoms, such as fever or asthenia (77%). However, in a minority of cases (23%), as in the current case, skin manifestations may be concomitant with or precede haematological detection of leukaemia. Although LC may be clinically polymorphic, the most commonly observed clinical manifestations are rubbery papules becoming firmer with increasing size (as in the current patient), or nodules (Fig. 1B) (3). Topographically, lesions observable in the course of LC may be localized or diffusely distributed, single or multiple. Typically, generalized diffusion and rapid progression of lesions, as presented by the current patient, are more frequently associated with acute forms of leukaemia (1). Due to its polymorphous clinical presentation and its rarity, in cases where a diagnosis of leukaemia is not already established, LC may be difficult to diagnose, and there are various possible differential diagnoses. The principal differential diagnoses, presenting with papules and nodules, mostly polymorphic, that must be ruled out, comprise infections, drug reactions, skin metastases of visceral malignancy, and primary cutaneous lymphomas (1).
In the current case, infections and especially bacterial zoonoses (brucellosis, Carrion’s disease) were the first suspected diagnosis due to the patient’s occupational risk, the fever and asthenia. However, serology and culture tests excluded these diagnoses. The patient reported no medication intake in the period before the onset of symptoms, and no peripheral eosinophilia, characteristic in most drug reactions, was detected from blood tests, ruling out a drug reaction.
Taking into consideration the fever and asthenia, lymphocytopaenic leukopaenia combined with normocytic anaemia on blood tests and multiple lymphadenopathies, an onco-haematological disease represented the main diagnostic option. Thus, a skin biopsy was performed to confirm the diagnostic suspicion of LC.
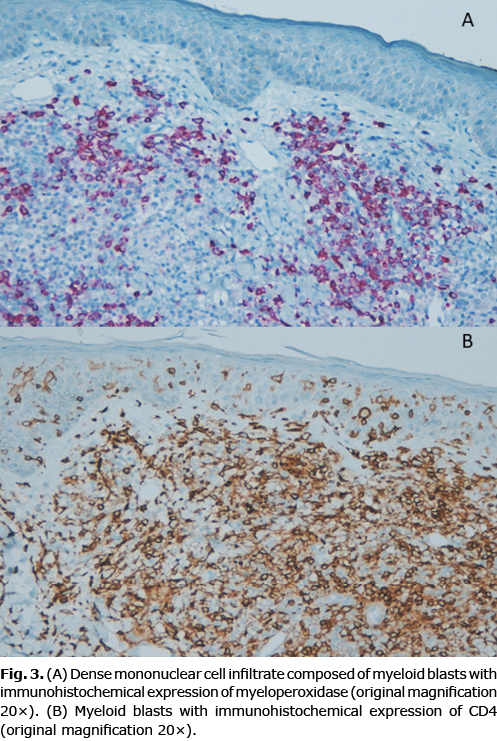
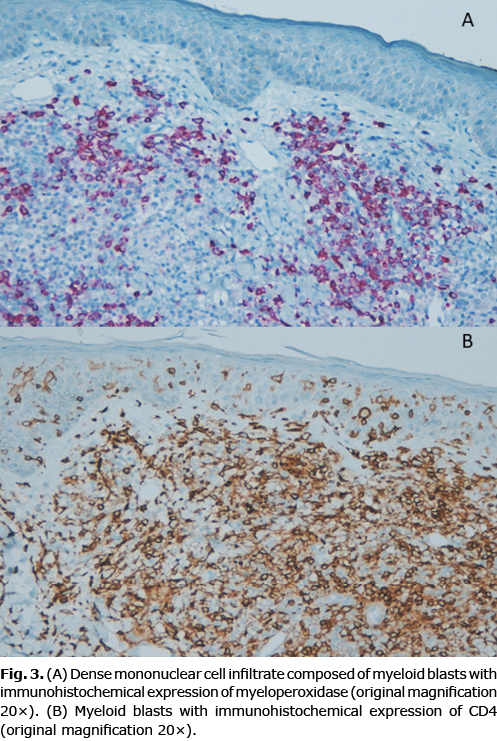
Histological examination revealed the presence of superficial and deep dermal infiltration by small- and medium-sized blasts. These elements displayed immunophenotype expression of myeloperoxidase (MPO), CD4 and weak expression of CD123, results consistent with extramedullary localization of AML (Fig. 3).
Although LC is a rare skin condition, dermatologists should be aware of this severe entity, in order to diagnose and address treatment of the underlying leukaemia.
Suspicion should be raised in particular in febrile patients who present with polymorphic skin rash including papules or nodules. Dermatologists will be confronted with the severest forms of LC, derived from AML, as this type of leukaemia is most frequently associated with cutaneous localizations, mostly generalized and with rapid onset. Medical dermatology practitioners must be aware of these entities, as the eye sees only what the mind is prepared to comprehend (1).
The authors have no conflicts of interest to declare.
REFERENCES
- Wagner G, Fenchel K, Back W, Schulz A, Sachse MM. Leukemia cutis – epidemiology, clinical presentation, and differential diagnoses. J Dtsch Dermatol Ges 2012; 10: 27–36.
- Cho-Vega JH, Medeiros LJ, Prieto VG, Vega F. Leukemia cutis. Am J Clin Pathol 2008; 129: 130–142.
- Su WP, Buechner SA, Li CY. Clinicopathologic correlations in leukemia cutis. J Am Acad Dermatol 1984; 11: 121–128.