A 6-year-old boy presented with cutaneous papules and nodules on his left ear and left upper arm, of 1 year’s duration. The patient had no pain or itching from the nodules and no systemic symptoms, such as night sweat, fever or weight loss. He had also recently developed an uncharacteristic rash on his cheeks, with occasional itching. There was no family history of other dermatological diseases and no known allergies. The patient was referred for further dermatological examination.
Clinical examination revealed 3 small, elevated papules on the helix of the left ear, each around 3-mm diameter (Fig. 1). The papules had a blue-violet colour and soft consistency. A larger purple nodule was present on the left upper arm and a blue-violet maculopapular rash was visible on the cheeks. No cervical or inguinal lymphadenopathy was detected.

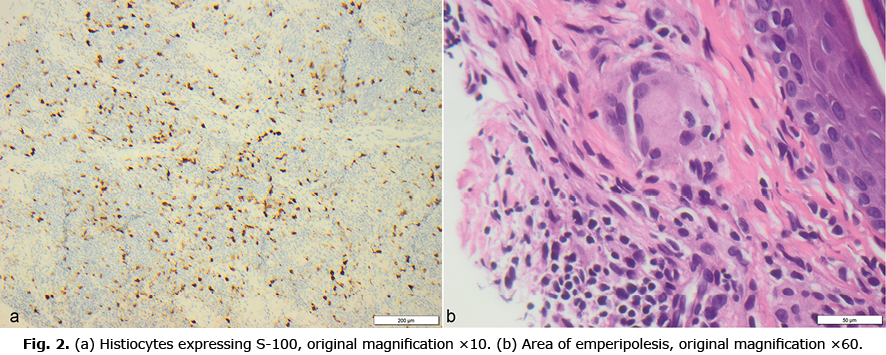
A punch biopsy was obtained from the nodule on the left upper arm, and histopathological evaluation demonstrated a dermis with diffuse infiltration of lymphocytes admixed with histiocytes and plasma cells. The histiocytes expressed S-100, but not CD1A or langerin (Fig. 2a). Areas of emperipolesis were identified (Fig. 2b).
What is your diagnosis? See next page for answer.
Persistent Cutaneous Papules and Nodules in a Six-year-old Child: A Commentary
Acta Derm Venereol 2022; 102: adv00725.
DOI: 10.2340/actadv.v102.2170
Diagnosis: Cutaneous Rosai-Dorfman Disease
The patient presented papules and nodules on the helix of the ear and the upper arm. To rule out potential systemic involvement, he was referred to the Department of Paediatrics. Laboratory findings revealed normal leucocytes, erythrocyte sedimentation rate, C-reactive protein, and immunoglobulin G, and an ultrasound examination of the abdomen did not reveal any abnormalities or enlarged lymph nodes. The patient was diagnosed with cutaneous Rosai-Dorfman disease (RDD) due to the characteristic histopathological findings and no systemic involvement. The histopathological hallmarks of RDD are S-100 expression of histiocytes without CD1A expression and detection of emperipolesis, which is phagocytosis of intact leucocytes especially lymphocytes (1).
RDD is a benign histiocytic proliferative disease, also called sinus histiocytosis with massive lymphadenopathy. Classic RDD manifests with cervical painless lymphadenopathy and systemic symptoms, such as fever, loss of weight, and night sweats, often accompanied by laboratory changes, such as leukocytosis, neutrophilia, polyclonal hypergammaglobulinaemia and elevated erythrocyte sedimentation rate (2, 3). In addition, RDD can involve extranodal sites, such as the skin, nasal cavity, orbital tissue, bone, and central nervous system (3). The skin is the most common extranodal site (4). However, a cutaneous form also exists, in which the manifestations are present exclusively in the skin, as was the case in the current patient.
In the current case, the histopathological hallmarks, S-100 expression of histiocytes without CD1A expression and detection of emperipolesis, were crucial to obtain the correct diagnosis. Differential diagnoses, such as juvenile spring eruption, lymphocytoma cutis, and cutaneous marginal zone lymphoma were considered before histological report. A correct clinical diagnosis of cutaneous RDD can be challenging as the manifestations can range from solitary or numerous papules, nodules or plaques, or a combination of these. Typically, the lesions are asymptomatic, but tenderness, pruritus or ulceration can occur (5, 6). The lesions are mostly localized to the extremities, followed by the trunk and face (5).
The aetiology of RDD is unknown. However, infections such as Epstein-Barr virus, human immunodeficiency virus, human herpesvirus-6, herpes simplex virus, and abnormalities of the immune system have been suggested to be associated with RDD (5).
RDD affects younger patients, with a median age of approximately 20 years, whereas patients with cutaneous RDD have an older age at onset (median age 43.5 years) (3, 4). However, the current patient was only 6 years old. Cutaneous RDD in children is thus extremely rare, and, to our knowledge, only 6 cases have been reported previously (7).
The indication for treatment in cutaneous RDD is often due to symptomatic lesions or systemic progression. Different treatment options have been reported, such as excision of lesions, topical steroids, retinoids, thalidomide, alkylating agents, radiotherapy or “wait-and-watch” therapy (6, 7). The response to treatment is variable, but most patients experience resolution of their lesions (7, 8). This patient was treated symptomatically with topical steroid (group 3) and frequent follow-up visits, and the parents were informed about the likely benign nature of the diagnosis of cutaneous RDD.
This case adds further to the limited literature on cutaneous RDD in children. The case highlights the importance of punch biopsies in the elucidation of cutaneous RDD, as the clinical manifestations may mimic other dermatological disorders. Indeed, more potential malignant skin disorders, such as lymphomatoid papulosis, may have clinical similarities with cutaneous RDD. Although cutaneous RDD usually affects adults, this case illustrates that cutaneous RDD should also be considered in children.
ACKNOWLEDGEMENTS
This research was conducted in accordance with the principles of the Declaration of Helsinki.
Written informed consent was obtained from the parents of the patient for publication of this case report and any accompanying images.
The authors have no conflicts of interest to declare.
REFERENCES
- Fayne R, Rengifo SS, Gonzalez I, Solorzano JL, Gonzalez D, Vega F, et al. Primary cutaneous Rosai-Dorfman disease; a case-based review of a diagnostically and therapeutically challenging rare variant. Ann Diagn Pathol 2020; 45: 151446.
- Dalia S, Sagatys E, Sokol L, Kubal T. Rosai-Dorfman disease: tumor biology, clinical features, pathology, and treatment. Cancer Control 2014; 21: 322–327.
- Bruce-Brand C, Schneider JW, Schubert P. Rosai-Dorfman disease: an overview. J Clin Pathol 2020; 73: 697–705.
- Fang S, Chen AJ. Facial cutaneous Rosai-Dorfman disease: a case report and literature review. Exp Ther Med 2015; 9: 1389–1392.
- Ahmed A, Crowson N, Magro CM. A comprehensive assessment of cutaneous Rosai-Dorfman disease. Ann Diagn Pathol 2019; 40: 166–173.
- Frater JL, Maddox JS, Obadiah JM, Hurley MY. Cutaneous Rosai-Dorfman disease: comprehensive review of cases reported in the medical literature since 1990 and presentation of an illustrative case. J Cutan Med Surg 2006; 10: 281–290.
- Gupta A, Arora P, Batrani M, Sharma PK. Multifocal cutaneous Rosai-Dorfman disease masquerading as lupus vulgaris in a child. An Bras Dermatol 2018; 93: 764–774.
- Toledo Del Castillo B, Mata-Fernández C, Rodríguez Soria VJ, Parra Blanco V, Loughlin G, Campos-Domínguez M. Self-healing extranodal cutaneous Rosai-Dorfman in a child. Pediatr Dermatol 2015; 32: e249–250.