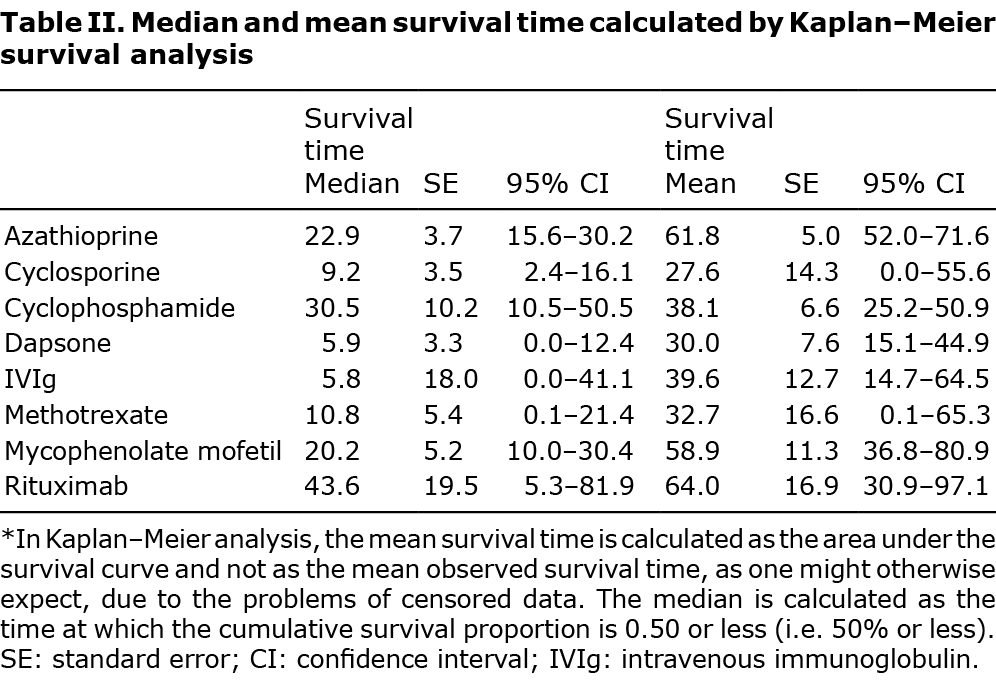
Drug survival reflects the real-life efficacy and safety of therapeutic agents. Evidence regarding the durability of adjuvant agents in the treatment of pemphigus is sparse. The aims of this study were to investigate the survival of adjuvant agents used to manage patients with pemphigus, and to identify predictors of treatment dropout. A retrospective population-based cohort study was designed to follow patients with pemphigus managed by adjuvant agents. The study population included 436 patients with pemphigus managed by 608 adjuvant agent courses. The highest median drug survival time was observed for rituximab (43.6 months, 95% confidence interval (95% CI) 5.3–81.9), followed by cyclophosphamide (30.5 months; 95% CI 10.5–50.5), azathioprine (22.9 months; 95% CI 15.6–30.2), and mycophenolate mofetil (20.2 months; 95% CI 10.0–30.4). Compared with azathioprine, cyclosporine (adjusted hazard ratio 2.98; 95% CI 1.57–5.62; p = 0.005) and dapsone (adjusted hazard ratio 1.83; 95% CI 1.07–3.15; p = 0.027) were associated with a significantly increased risk of drug discontinuation. To conclude, rituximab, azathioprine, and mycophenolate mofetil demonstrated better durability, whilst dapsone and cyclosporine were associated with low drug survival and high dropout.
Key words: adjuvant drugs; drug survival; rituximab; azathioprine; mycophenolate mofetil; cyclophosphamide; dapsone; cyclosporine; intravenous immunoglobulin; methotrexate.
Accepted May 10, 2021; Epub ahead of print May 18, 2021
Acta Derm Venereol 2021; 101: adv00535.
doi: 10.2340/00015555-3831
Corr: Khalaf Kridin, Lübeck Institute of Experimental Dermatology, University of Lübeck, Ratzeburger Allee 160, DE-23562 Lübeck, Germany. E-mail: dr_kridin@hotmail.com
SIGNIFICANCE
This large-scale population-based cohort study found that rituximab had the highest median drug survival time compared with the remaining adjuvant agents used to treat patients with pemphigus. Dapsone and cyclosporine were associated with increased risk of adjuvant drug dropout. This study provides evidence in favour of the efficacy and safety of azathioprine, mycophenolate mofetil, and rituximab in pemphigus, and implies that the use of dapsone and cyclosporine in pemphigus should be abandoned.
INTRODUCTION
Prior to the advent of systemic corticosteroids, pemphigus was fatal within the initial 2 years following presentation (1). More recently, the rapid tapering of corticosteroids after consolidation, as well as the introduction of novel adjuvant immunosuppressants with a better safety profile, have decreased both the morbidity and the mortality of patients with pemphigus (2, 3). Currently, the 1-year mortality rate of pemphigus has been reduced drastically with proper management, but is still increased relative to the general population (2–5).
One of the main unmet objectives in the management of patients with pemphigus is to maintain long-term remission and prevent recurrences, using the smallest cumulative dose of systemic corticosteroids for the shortest time possible. The introduction of adjuvant agents has demonstrated a favourable steroid-sparing effect and contributed, at least in part, to the accomplishment of this target (1, 6–8). These agents are commonly used in combination with corticosteroids, particularly in recalcitrant disease, when complications due to prolonged use of corticosteroids occur, or in dose-dependency above minimal therapy (> 10 mg/day prednisolone) (1). However, evidence that the addition of adjuvants is superior to treatment with corticosteroid monotherapy has only recently been found for rituximab (9). The long-term risk-benefit analysis of adjuvant agents in pemphigus remains to be firmly established.
Drug survival is a newly introduced term in the field of chronic inflammatory skin diseases, signifying the time-period of treatment with a certain drug until its cessation. While this term reflects several pivotal features of the drug used, such as its long-term efficacy and safety, it may also account for aspects such as patient compliance, expenditure, and local healthcare regulations (10). Drug survival analysis has emerged as a reliable real-life measurement of drug success in psoriasis and atopic dermatitis (11, 12). However, this analysis is yet to be performed in pemphigus, leaving the literature inconclusive with regard to the comparison between the durability, efficacy, and safety profile of adjuvant drugs in pemphigus.
The aim of the current study is to compare the drug survival of the available adjuvant agents used to manage patients with pemphigus. An additional aim is to identify predictors for adjuvant drug cessation during the course of pemphigus.
METHODS
Study design and database
This study was designed as a historical retrospective cohort study following patients with pemphigus managed by adjuvant agents between the years 2000 and 2019. The study was approved by the institutional review board of Ben-Gurion University.
The computerized dataset of Clalit Health Services (CHS) was the origin of the current study. CHS is the main healthcare organization in Israel, providing a wide array of private and public healthcare services for 4,927,000 enrolees as of October 2018 (58% of the general Israeli population). CHS possesses a multitude of primary, secondary, and tertiary referral centres, inpatient and community-based clinics, pharmacies, and imaging facilities across the whole country, with inclusive computerized documentation. As such, the computerized database of CHS is typified by a prominent comprehensiveness, since it retrieves data from a multitude of sources. Loss to follow-up is minimal, and access to CHS services is free, rendering this dataset highly compatible with performing epidemiological studies (13).
Study population and definition of main covariates
The computerized dataset of CHS was systematically checked for incident cases with a diagnosis of pemphigus between the years 2000 and 2019. The definition of pemphigus was based on 1 of the following eligibility criteria: (i) documented diagnosis of pemphigus registered by a community-based board-certified dermatologist; or (ii) diagnosis of pemphigus in discharge letters of patients admitted to dermatological wards.
Patients fulfilling the definition of pemphigus were subject to inclusion if they were prescribed systemic corticosteroids in conjunction with one of the following adjuvant agents: azathioprine, cyclosporine, cyclophosphamide, dapsone, intravenous immunoglobulin (IVIg), methotrexate, mycophenolate mofetil (MMF), and rituximab. A patient was considered under active treatment when there was a continuity of treatment with at least 2 claims per medication in the absence of treatment termination (event, as defined below). Since a patient could have received 2 or more adjuvant agents within the study duration, it is likely that the same patient could have been included more than once in the analysis, each time for a different treatment series with a different adjuvant agent.
An event of drug termination or drug dropout was defined in any of the following cases: (i) in adjuvant agent switch; (ii) cessation of an adjuvant drug during the initial 6 months following its initial administration (cessation was determined if no prescription for oral adjuvant drugs was claimed for more than 270 days). The latter timeframe was adopted to account for temporary breaks in treatment due to pregnancy and other non-medical reasons (i.e. financial reasons and logistic limitations). Discontinuation was defined as occurring during only the first 6 months following drug initiation, to enable differentiation between cases in which the drug was efficient and those in which it was stopped due to remission off-therapy.
Analysis of the risk of dropout included only oral agents administered on a daily basis, thus rituximab and IVIg were excluded from this analysis given their different therapeutic life. Death, emigration from Israel, or the end of the follow-up period were defined as censored. The survival period for each adjuvant agent per patient was calculated.
Statistical analysis
Baseline characteristics were described by means and standard deviations (SDs) for continuous variables, whilst categorical values were indicated by percentages. Continuous variables were compared using analysis of variance (ANOVA) and the non-parametric Kruskal–Wallis H test (based on the homogeneity of variance in each comparison as determined by Levene’s test). Dichotomous variables were compared by Pearson χ2 test.
Survival analyses were conducted using the Kaplan–Meier method. A log-rank test was run to determine if there were differences in the survival distribution for the different adjuvant agents. Pairwise log-rank comparisons were conducted to determine which intervention groups had different survival distributions. A Bonferroni correction was made with statistical significance accepted at the p < 0.006 (0.05/8 (regular level of significance/ number of compared subgroups)) level. Hazard ratios (HRs) for the risk of termination of each of the adjuvant drugs were obtained by the use of the Cox regression model, which was additionally adjusted for putative confounders. When presenting the HR of the adjuvant drug variable, the reference group was the agent with the longest median and mean survival (rituximab). Two-tailed p-values < 0.05 were considered statistically significant. All statistical analyses were performed using SPSS software, version 25 (SPSS, IBM Corp., Armonk, NY, USA).
RESULTS
Study population
The study population included 436 patients with pemphigus managed by systemic corticosteroids in conjunction with 608 adjuvant treatment courses. The mean age (SD) of presentation with pemphigus was 57.8 (15.6) years, 165 (37.8%) patients were male, and 363 (83.3%) were of Jewish ethnicity. The mean (SD) length of exposure to systemic corticosteroids among these patients was 144.4 (80.5) months, with 347 (79.6%) patients being treated for more than 60 months. Eligible patients were managed by a mean of 1.2 (0.7) adjuvant agents per patient, with 92 patients (21.1%) being managed by more than one single adjuvant agent. The demographic and clinical characteristics of the study population are shown in Table I.

The most frequently prescribed adjuvant agent was azathioprine, which has been administered in 331 patients, followed by MMF (n = 86), dapsone (n = 60), cyclophosphamide (n = 45), rituximab (n = 33), cyclosporine (n = 22), IVIg (n = 20), and methotrexate (n = 11). Patients managed by methotrexate and intravenous immunoglobulin were older at the initiation of treatment, whilst patients managed by azathioprine and cyclophosphamide were less frequently exposed to additional adjuvant agents (Table I).
Kaplan-Meier analysis
Fig. 1 presents the drug survival of each of the 8 adjuvant agents investigated using Kaplan–Meier methodology. The survival distributions for the 8 interventions were statistically significantly different (χ2(7)=17.32; p = 0.015). When a Bonferroni correction was made with statistical significance accepted at the p < 0.006 level, there was a statistically significant superiority in survival distributions for azathioprine over dapsone (χ2(1)=11.56; p = 0.001) as well as a near-significant superiority for MMF over dapsone (χ2(1)=6.83; p = 0.009) and for rituximab over dapsone (χ2(1)=6.20; p = 0.013). Log-rank pairwise comparisons did not reveal significant differences in the survival distribution between other agents.

Patients who underwent rituximab treatment had the highest median (43.6 (95% CI 5.3–81.9) months) and mean (64.0 (95% CI 30.9–97.1) months) drug survival time. The medians and means of drug survival time per adjuvant agent are shown in Table II.
Predictors and risk factors of treatment termination
During the study period, 294 cases of oral daily-administered drug termination were encountered. To identify risk factors that precipitate drug dropout, a Cox regression analysis was performed (Table III). Relative to azathioprine, cyclosporine (adjusted HR, 2.98; 95% CI 1.57–5.62; p = 0.005) and dapsone (adjusted HR, 1.83; 95% CI 1.07–3.15; p = 0.027) were associated with a significantly increased risk of drug dropout. Age, sex, ethnicity, body mass index (BMI), smoking, and the administration of systemic corticosteroids for more than 12 months did not demonstrate a statistically significant effect on oral adjuvant drug dropout (Table III).

The study then explored whether the sequence in which the adjuvant agents were administered had an effect on drug survival (Table IV). For MMF, there was a near-significant increased risk of dropout when the drug was given as a second-line adjuvant agent (adjusted HR, 1.84; 95% CI 0.94–3.63; p = 0.077) compared with its first-line use. Drug survival was not influenced whether azathioprine and cyclophosphamide were administered as first-line or second-line treatments (Table IV).

DISCUSSION
This study demonstrates that adjuvant agents in pemphigus have differential drug survival over time. Azathioprine was found to be significantly more persistent than dapsone in a real-time setting. The drug survival of MMF and rituximab was also increased relative to dapsone, although with only marginal statistical significance. The highest mean and median drug survival times were attributed to rituximab. Compared with rituximab, dapsone and cyclosporine were associated with a significantly increased risk of drug discontinuation. An extended systemic corticosteroid therapy exceeding 5 years confers protection against adjuvant drug dropout.
Although adjuvant agents are frequently prescribed for patients with pemphigus, there is a sparsity of high-quality randomized controlled studies evidencing the benefits of adjuvant agents in pemphigus. Most studies have demonstrated that oral adjuvants imposed a steroid-sparing effect and led to steroid-free remission, but did not cause differences in the main disease outcome measures (1, 14–19) A meta-analysis summarizing studies evaluating azathioprine, MMF, cyclophosphamide, cyclosporine, IVIg, plasmapheresis, and infliximab in patients with pemphigus vulgaris (PV) concluded that these adjuvants did not increase remission rates, but reduced the risk of relapse by 29% compared with prednisolone monotherapy (20). It was not until 2017 that the first randomized controlled trial (RCT) confirmed that an adjuvant drug was superior to corticosteroid monotherapy; Joly et al. (9) demonstrated that rituximab in combination with short-term prednisone (0.5–1.0 mg/kg/day) led to a higher frequency of complete remission off-therapy, compared with patients treated with prednisone (1.0–1.5 mg/kg/day) alone at 24 months of follow-up (89% vs 34%, respectively). Moreover, patients in the rituximab arm experienced fewer major adverse events.
It is still to be decisively determined which agents should be invariably preferred. This question is influenced by multiple determinants related to the disease (severity, duration, subtype), to the patient (age, sex, fertility potential, and comorbidities (21)), as well as to other logistic considerations (domestic healthcare regulation, expenditure, availability of the drug). To complicate matters further, there is a lack of robust published evidence regarding the long-term efficacy and safety of these agents in pemphigus, principally owing to the scarcity of RCTs (6). Therefore, utilization of survival analysis, reflecting safety and efficacy measures in real-life practice, may provide physicians with a reference for administering adjuvant therapy in pemphigus.
The current study found that azathioprine, MMF, and rituximab demonstrated higher retention rates, whilst dapsone and cyclosporine had lower rates. These findings align with the majority of the published guidelines, which place azathioprine, MMF, and rituximab as the preferred adjuvant agents in combination with systemic corticosteroids. The European Dermatology Forum (EDF) guidelines, published in 2015, recommended the administration of azathioprine or MMF in conjunction with corticosteroids as a second-line treatment in patients failing treatment on corticosteroids monotherapy. The 2017 guidelines of the British Association of Dermatologists (BAD) advocated administration of azathioprine, MMF, and rituximab as first-line therapy in combination with corticosteroids. In the Delphi consensus of a panel of experts published in 2018 (7), rituximab was designated as first-line therapy (in combination with low-dose systemic corticosteroids) in new-onset moderate to severe pemphigus and/or for patients who do not achieve clinical remission with systemic corticosteroids and/or immunosuppressive adjuvants (7), while azathioprine and MMF were defined as first-line corticosteroid-sparing agents. Correspondingly, the S2K (22) guidelines in 2020 incorporated rituximab as first-line therapy in moderate-to-severe PV (in combination with 1.0 mg/kg prednisolone). In the same guidelines, the combination of azathioprine and MMF with 1.5 mg/kg prednisolone was defined as first-line therapy for these patients (22).
The lower persistence rate of dapsone and cyclosporine accords with the low evidence regarding their utility in the management of pemphigus. Although dapsone was recently recommended as an adjuvant drug for mild pemphigus foliaceus (22), the efficacy of this agent in pemphigus was based on case reports (in part of which the drug was started either with or shortly after prednisolone, thus hindering with revealing its independent role) (23, 24), and one RCT of 9 patients (25). The latter failed to show a significant superiority for adjuvant dapsone over placebo in tapering prednisone under 7.5 mg/day (25). Aligning with our results, the evaluation of cyclosporine in 2 RCTs did not delineate any advantage of cyclosporine in PV. In contrast, higher adverse events and toxicity were detected in the cyclosporine treatment arm (26, 27).
The current study represents the initial survival analysis of adjuvant drugs used in the management of patients with pemphigus. It throws light on the efficacy and safety of a wide array of drugs in a real-life setting and may provide physicians with a reference that may assist in choosing an adjuvant agent in pemphigus. The study population is relatively large, and the follow-up duration is extended, thus substantiating the validity of the findings. However, the current study has several limitations. The direct cause of drug cessation could not be retrieved, and the sample size of patients managed by methotrexate, cyclosporine, and IVIg was small. Unlike RCTs, in which the basal characteristics of eligible patients are comparable at enrolment, the current study is limited by imperfect age matching between treatment subgroups. In addition, the number of additional adjuvant agents was distributed differentially between different subgroups. While all investigated drugs were indicated by pemphigus, the study could not adjust for severity and natural course of the disease, which may embody significant determinants in tailoring the treatment regimen. In addition, the absence of data about morphological characteristics and basal severity of the disease interfered with an optimal comparison between used drugs.
In conclusion, significant differences in the persistence of adjuvant drugs in pemphigus were found in this large-scale population-based study. Rituximab was distinguished by the highest mean and median drug survival times, and the drug survival of dapsone was significantly inferior to azathioprine and near significantly inferior to MMF and rituximab. Relative to rituximab, cyclosporine and dapsone were associated with an increased risk of adjuvant drug discontinuation. Prolonged systemic corticosteroid for more than 5 years was associated with a lower risk of adjuvant drug dropout.
ACKNOWLEDGEMENTS
Conflicts of interest. ADC served as an advisor, investigator, or speaker for Abbvie, BI, Dexcel Pharma, Janssen, Novartis, Perrigo, Pfizer, and Rafa. DTB received a research grant from Pfizer.
The authors have no conflicts of interest to declare.
REFERENCES
- Hertl M, Jedlickova H, Karpati S, Marinovic B, Uzun S, Yayli S, et al. Pemphigus. S2 guideline for diagnosis and treatment – guided by the European Dermatology Forum (EDF) in cooperation with the European Academy of Dermatology and Venereology (EADV). J Eur Acad Dermatol Venereol 2015; 29: 405–414.
- Bystryn JC, Steinman NM. The adjuvant therapy of pemphigus. An update. Arch Dermatol 1996; 132: 203–212.
- Schmidt E, Kasperkiewicz M, Joly P. Pemphigus. Lancet 2019; 394: 882–894.
- Kridin K, Zelber-Sagi S, Bergman R. Pemphigus vulgaris and pemphigus foliaceus: Differences in epidemiology and mortality. Acta Derm Venereol 2017; 97: 1095–1099.
- Kridin K, Zelber-Sagi S, Bergman R. Mortality and cause of death in patients with pemphigus. Acta Derm Venereol 2017; 97: 607–611.
- Kridin K. Emerging treatment options for the management of pemphigus vulgaris. Ther Clin Risk Manag 2018; 14: 757–778.
- Murrell DF, Peña S, Joly P, Marinovic B, Hashimoto T, Diaz LA, et al. Diagnosis and management of pemphigus: recommendations of an international panel of experts. J Am Acad Dermatol 2020; 82: 575–585.e1.
- Harman KE, Brown D, Exton LS, Groves RW, Hampton PJ, Mohd Mustapa MF, et al. British Association of Dermatologists’ guidelines for the management of pemphigus vulgaris 2017. Br J Dermatol 2017; 177: 1170–1201.
- Joly P, Maho-Vaillant M, Prost-Squarcioni C, Hebert V, Houivet E, Calbo S, et al. First-line rituximab combined with short-term prednisone versus prednisone alone for the treatment of pemphigus (Ritux 3): a prospective, multicentre, parallel-group, open-label randomised trial. Lancet 2017; 389: 2031–2040.
- Shalom G, Cohen AD, Ziv M, Eran CB, Feldhamer I, Freud T, et al. Biologic drug survival in Israeli psoriasis patients. J Am Acad Dermatol 2017; 76: 662–669.e1.
- Lin PT, Wang SH, Chi CC. Drug survival of biologics in treating psoriasis: a meta-analysis of real-world evidence. Sci Rep 2018; 8: 16068.
- Law Ping Man S, Bouzillé G, Beneton N, Safa G, Dupuy A, Droitcourt C. Drug survival and postdrug survival of first-line immunosuppressive treatments for atopic dermatitis: comparison between methotrexate and cyclosporine. J Eur Acad Dermatology Venereol 2018; 32: 1327–1335.
- Cohen AD, Dreiher J, Regev-Rosenberg S, Yakovson O, Lieberman N, Goldfracht M, et al. [The quality indigators program in Clalit Health Services: the first decade.] Harefuah 2010; 149: 204–209, 265 (in Hebrew).
- Martin LK, Werth VP, Villaneuva E V, Murrell DF. A systematic review of randomized controlled trials for pemphigus vulgaris and pemphigus foliaceus. J Am Acad Dermatol 2011; 64: 903–908.
- Chams-Davatchi C, Mortazavizadeh A, Daneshpazhooh M, Davatchi F, Balighi K, Esmaili N, et al. Randomized double blind trial of prednisolone and azathioprine, vs. prednisolone and placebo, in the treatment of pemphigus vulgaris. J Eur Acad Dermatology Venereol 2013; 27: 1285–1292.
- Beissert S, Werfel T, Frieling U, Böhm M, Sticherling M, Stadler R, et al. A comparison of oral methylprednisolone plus azathioprine or mycophenolate mofetil for the treatment of pemphigus. Arch Dermatol 2006; 142: 1447–1454.
- Beissert S, Mimouni D, Kanwar AJ, Solomons N, Kalia V, Anhalt GJ. Treating pemphigus vulgaris with prednisone and mycophenolate mofetil: a multicenter, randomized, placebo-controlled trial. J Invest Dermatol 2010; 130: 2041–2048.
- Ioannides D, Apalla Z, Lazaridou E, Rigopoulos D. Evaluation of mycophenolate mofetil as a steroid-sparing agent in pemphigus: a randomized, prospective study. J Eur Acad Dermatol Venereol 2012; 26: 855–860.
- Chams-Davatchi C, Esmaili N, Daneshpazhooh M, Valikhani M, Balighi K, Hallaji Z, et al. Randomized controlled open-label trial of four treatment regimens for pemphigus vulgaris. J Am Acad Dermatol 2007; 57: 622–628.
- Atzmony L, Hodak E, Leshem YA, Rosenbaum O, Gdalevich M, Anhalt GJ, et al. The role of adjuvant therapy in pemphigus: a systematic review and meta-analysis. J Am Acad Dermatol 2015; 73: 264–271.
- Kridin K, Jones VA, Patel PM, Zelber-Sagi S, Hammers CM, Damiani G, et al. Patients with pemphigus are at an increased risk of developing rheumatoid arthritis: a large-scale cohort study. Immunol Res 2020; 68: 373–378.
- Schmidt E, Sticherling M, Sárdy M, Eming R, Goebeler M, Hertl M, et al. S2k guidelines for the treatment of pemphigus vulgaris/foliaceus and bullous pemphigoid: 2019 update. J Dtsch Dermatol Ges 2020; 18: 516–526.
- Piamphongsant T. Pemphigus controlled by dapsone. Br J Dermatol 1976; 94: 681–686.
- Haim S, Friedman-Birnbaum R. Dapsone in the treatment of pemphigus vulgaris. Dermatologica 1978; 156: 120–123.
- Werth VP, Fivenson D, Pandya AG, Chen D, Rico MJ, Albrecht J, et al. Multicenter randomized, double-blind, placebo-controlled, clinical trial of dapsone as a glucocorticoid-sparing agent in maintenance-phase pemphigus vulgaris. Arch Dermatol 2008; 144: 25–32.
- Ioannides D, Chrysomallis F, Bystryn JC. Ineffectiveness of cyclosporine as an adjuvant to corticosteroids in the treatment of pemphigus. Arch Dermatol 2000; 136: 868–872.
- Chrysomallis F, Ioannides D, Teknetzis A, Panagiotidou D, Minas A. Treatment of oral pemphigus vulgaris. Int J Dermatol 1994; 33: 803–807.