Cutis laxa is a rare skin disorder, characterized by loose, redundant, hypoelastic skin. The aetiology of cutis laxa is unknown; the condition is associated with malignancies, medications, infections and other conditions (1). Some cases develop cardiac and pulmonary complications, such as emphysema and bronchiectasis. We describe here a patient with generalized acquired cutis laxa associated with IgA-λ monoclonal gammopathy of undetermined significance (MGUS) who developed severe emphysema. Successful treatment with diaminodiphenyl sulfone (dapsone) and immunohistochemical analysis indicate the possible contribution of neutrophil extracellular traps (NETs).
CASE REPORT
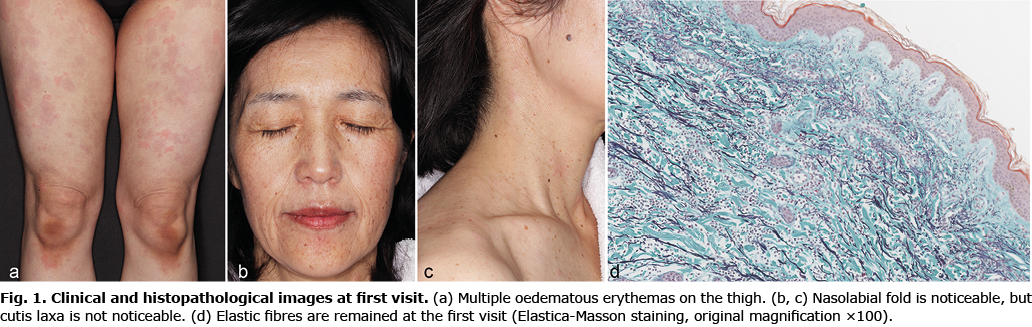
A 47-year-old woman, with a non-contributory medical history, presented with a 1-year history of urticaria-like rash that lasted for several days on both forearms, abdomen, and thighs, with no sign of skin ageing. The rash recurred once a month (Fig. 1a–b). The rash was accompanied by gradually developing skin pigmentation, tenderness, itch, and myalgia-like pain. Skin biopsy from the oedematous erythema of her right forearm revealed diffuse inflammatory cell infiltration, composed mainly of neutrophils in the entire dermis. Nuclear dust and slight extravasation of red blood cells were observed around the dermal blood vessels. Elastica-Masson staining showed no abnormalities in elastic fibres (Fig. 1d). Based on these findings, our first diagnosis was unspecified neutrophilic dermatosis, suspected of neutrophilic urticaria or urticarial vasculitis. The skin symptoms improved after oral treatment with olopatadine, doxycycline, and cimetidine. Although urticaria-like rash appeared approximately once a month, the treatment was continued because it effectively reduced tenderness, itch and myalgia-like pain. After 3 years, the patient developed a dry cough and respiratory distress during exertion, and severe emphysema and IgA-λ MGUS were diagnosed by detailed examination at our hospital. Because the progression of emphysema was rapid, lung transplantation was also considered. The patient was again referred to our department for evaluation of the relationship between her emphysema and skin condition. Compared with the appearance at the first visit, her skin showed sagging and wrinkles (Fig. 2a and b). A skin biopsy from the left forearm showed neutrophil infiltration very similar to the initial biopsy, although the elastic fibres had disappeared entirely (Fig. 2c). In addition, immunohistochemical analysis revealed diffuse IgG and IgA deposits in the dermis. Since this patient was planned to undergo lung transplantation, the whole-body screening tests, including computed tomography, endoscopy and echocardiography, were performed, and there were no abnormal findings. From the clinical and histopathological findings, the patient was diagnosed with generalized acquired cutis laxa. Because histopathological findings suggested neutrophil activation, treatment with diaminodiphenyl sulfone (50 mg/day) was started. After treatment, the progression of skin symptoms and emphysema stopped, and in the pulmonary function test, the vital capacity was improved, but the forced expiratory volume in 1 s as a percentage of forced vital capacity did not change. Furthermore, to date, the patient’s lung transplantation has been postponed for approximately 3 years. The same dosage of diaminodiphenyl sulfone was maintained because the symptoms relapsed when the dose was reduced.

DISCUSSION
It is speculated that cutis laxa is caused by increased decomposition or decreased production of elastic fibres, and the involvement of neutrophil elastase has been reported as one of the possible contributions (2). Maruani and others demonstrated that monoclonal paraprotein bound to elastic fibres in a case of generalized acquired cutis laxa with monoclonal light chain disease under the electron microscope (3). Their observation suggested that abnormal monoclonal immunoglobulin deposition triggers complement activation. Neutrophil activation would be induced by activation of the classical complement pathway by deposition of abnormal immunoglobulin in the current case, which supports the previous observation that monoclonal gammopathy may be involved in the development of cutis laxa (4, 5). In addition, a previous report suggested that NET might be involved in urticarial rash associated with systemic symptoms, such as Schnitzler’s syndrome, but not in chronic spontaneous urticaria (6). Thus, we investigated the mechanism of neutrophil activation and NET formation. Brinkmann and others first reported that neutrophils exposed to bacteria release intranuclear chromatin to extracellular space: this phenomenon is designated NETs (7). In the present case, immunostaining revealed citrullinated histone H3, a hallmark of NETs, among neutrophil nuclei (Fig. 2d), and diffuse dermal deposition of neutrophil elastase (Fig. 2e), indicating that NET formation was promoted in the dermis. Recently, it has been demonstrated that NETs are related to the pathophysiology of systemic lupus erythematosus, rheumatoid arthritis, and anti-neutrophil cytoplasmic antibody-associated vasculitis, in addition to infectious diseases (8). This case suggests the contribution of NET formation to the pathogenesis of cutis laxa and possibly associated emphysema by degrading elastic fibres of skin and lung tissue. Considering the progression from an unspecified neutrophilic dermatosis to cutis laxa possibly caused by neutrophilic elastase, we retrospectively considered the neutrophilic dermatosis seen at the first visit as the initial sign of generalized acquired cutis laxa (9).
In this case, diaminodiphenyl sulfone suppressed urticarial rash as well as the progression of cutis laxa and emphysema, which may be due to its suppressive effects on neutrophil functions, such as migration and myeloperoxidase activity.
ACKNOWLEDGEMENTS
Setsuya Aiba had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. The authors thank the patient for granting permission to publish this information.
The authors have no conflicts of interest to declare.
REFERENCES
- Berk DR, Bentley DD, Bayliss SJ, Lind A, Urban Z. Cutis laxa: a review. J Am Acad Dermatol 2012; 66: 842.e841–817.
- O’Malley JT, D’Agati VD, Sherman WH, Grossman ME. Acquired cutis laxa associated with heavy chain deposition disease involving dermal elastic fibers. JAMA Dermatol 2014; 150: 1192–1196.
- Maruani A, Arbeille B, Machet MC, Barbet C, Laure B, Martin L, et al. Ultrastructural demonstration of a relationship between acquired cutis laxa and monoclonal gammopathy. Acta Derm Venereol 2010; 90: 406–408.
- Jachiet M, Harel S, Saussine A, Battistella M, Rybojad M, Asli B, et al. Cutis laxa associated with monoclonal gammopathy: 14 new cases and review of the literature. J Am Acad Dermatol 2018; 79: 945–947.
- New HD, Callen JP. Generalized acquired cutis laxa associated with multiple myeloma with biphenotypic IgG-λ and IgA-κ gammopathy following treatment of a nodal plasmacytoma. Arch Dermatol 2011; 147: 323–328.
- Bonnekoh H, Scheffel J, Wu J, Hoffmann S, Maurer M, Krause K. Skin and systemic inflammation in schnitzler’s syndrome are associated with neutrophil extracellular trap formation. Front Immunol 2019; 10: 546.
- Brinkmann V, Reichard U, Goosmann C, Fauler B, Uhlemann Y, Weiss DS, et al. Neutrophil extracellular traps kill bacteria. Science 2004; 303: 1532–1535.
- Jorch SK, Kubes P. An emerging role for neutrophil extracellular traps in noninfectious disease. Nat Med 2017; 23: 279–287.
- Gusdorf L, Lipsker D. Neutrophilic urticarial dermatosis: an entity bridging monogenic and polygenic autoinflammatory disorders, and beyond. J Eur Acad Dermatol Venereol 2020; 34: 685–690.