The burden of atopic dermatitis (AD) appears to be increasing in adult and elderly patients. The aim of this study was to analyse the nationwide database of the Finnish Institute for Health and Welfare regarding the number of patients with AD and of general practitioner consultations in Finland during 2018. The database comprised the main diagnoses of all visits to public primary healthcare. There were 2,094,673 primary care patients (males/females 43.19/56.81%) and 20,905 patients with AD (1.00%) and 24,180 consultations due to AD (0.45%). The highest numbers of patients with AD were in the age groups 0–14 years (9,922 patients, 47.46%) and 15–65 years (9,144 patients, 43.74%). A substantial proportion of patients with AD were aged > 50 years (3,515 patients, 16.81%) or >65 years (1,947 patients, 9.31%). Regression analysis indicated a statistically significant association of age group with patient numbers (p = 0.032) and number of consultations (p = 0.030). There were no differences between direct age group comparisons (p = 0.303), sex (p = 0.389), or number of consultations/patient (p = 0.235). Patients with AD are prevalent in all age groups in Finnish primary care. Patient numbers were also relatively high in groups other than childhood, indicating that age-related distribution in primary care may be shifting to older ages.
Key words: atopic dermatitis; age group; primary care; Finland.
Accepted Jun 7, 2022; Epub ahead of print Jun 7, 2022
Acta Derm Venereol 2022; 102: adv00738.
DOI: 10.2340/actadv.v102.2287
Corr: Alexander Salava, Department of Dermatology and Allergology, Helsinki University Hospital, Meilahdentie 2, FIN-00250 Helsinki, Finland. E-mail: alexander.salava@hus.fi
SIGNIFICANCE
The aim of this study was to explore the occurrence of atopic dermatitis in different age groups of Finnish primary care. A nationwide database was analysed regarding the number of patients and of general practitioner consultations during 2018. Atopic dermatitis was a frequent reason to consult general practitioners (1.00% of all patients) and was seen in all age groups in Finnish primary care. The number of patients with atopic dermatitis was also relatively high in groups other than childhood, suggesting that the burden in primary care may be shifting to older ages.
INTRODUCTION
As one of the most frequent chronic skin diseases, atopic dermatitis (AD) causes a significant health and socio-economic burden (1). Its peak prevalence is in early childhood, but recent studies have shown that prevalence in older patient groups may be increasing (2). While worldwide incidences differ considerably, with the highest prevalence noted in developed countries, there is a body of data indicating a plateauing of incidence in younger patient groups (3). Many children experience remission until early adulthood, but, in subgroups of patients, AD follows a chronic-intermittent or relapsing course (4). Although incidence seems to decrease during the individual life-span, there have been reports of a relatively high frequency of AD in older age groups, indicating that the disease burden is not limited to childhood and may be shifting to older patient groups (5). In addition, there have been recent studies indicating that disease severity might be higher in older patients with AD (6).
Finland has one of the highest prevalence in the world (lifetime prevalence 21.9%, 12-month prevalence 10.1%) (7). Kiiski et al. (7) showed, in a population-based study, that the highest prevalence of AD in Finland is in persons aged 30–39 years (lifetime prevalence 28.6%, 12-month prevalence 15.4%), and subsequently decreases with age. Chan et al. (8) reported that, in the UK, the highest prevalence of AD was in children (18.3%) and adults older than 75 years (11.6%) concluding that the prevalence of AD in older age groups has increased during the last decades. Due to the centralized healthcare system, mild and moderate AD patients are treated mainly by general practitioners in Finland, making the primary care burden very relevant. AD is a frequent cause of consultations in children, but age-dependent profiles and the extent of AD in different age groups have been largely uncharacterized (9–11). The aim of this study was to investigate the age-dependent distribution of AD in Finnish primary care.
MATERIALS AND METHODS
A nationwide population-based study was carried out by analysing the database of the Finnish Institute for Health and Welfare (12). The number of patients with AD and of consultations due to AD in Finnish primary care during 1 calendar year (1 January to 31 December 2018) was assessed. Finnish healthcare is based on a decentralized state-funded system and a smaller private sector. The main components are primary care in local health centres and specialist care in central and university hospitals. In Finland, general practitioners (GPs) may consult specialist healthcare, but the diagnosis and management of mild to moderate AD is carried out mainly in primary care (13).
The Finnish Institute for Health and Welfare database comprised the main diagnoses of all GP visits in Finnish public primary healthcare. In addition, the number of consultations related to AD was analysed. Inclusion criteria were: physician-conducted diagnosis of AD (International Classification of Diseases 10th Revision (ICD-10) category L20), outpatient visit (all relevant practices in primary care), all age groups (0–99 years) and both sexes. The results for all municipalities in Finland were included. Finland’s population in 2018 was estimated to be 5.516 million (14). The database did not include subgroup diagnoses, disease onset or other patient characteristics, such as severity or associated diseases. The presented numbers are absolute numbers of patients with AD and number of GP visits (consultations) in which AD was the main diagnosis. From this information, the mean number of consultations per patient was calculated. The following age groups were discriminated in the database: 1 year and younger, 1–6 years, 7–14 years, 15–24 years, 25–49 years, 50–64 years, 65–74 years, 75–84 years, and 85 years and older. For comparisons, age groups were additionally clustered into 3 groups: 14 years and younger, 15–64 years and 65 years and older. In addition, there was a separate clustering of the age group 50 years and older to represent middle-aged and older adults. For each given age group, the database provided the absolute number of patients and number of consultations, but did not include the age distribution inside the group.
The results are presented with descriptive statistics, and statistical analysis was carried out with IBM SPSS version 28.0, IBM, USA. Age group comparisons were calculated with the Pearson’s χ2 test and statistical significance was set at p < 0.05 with a 95% confidence interval (CI). Linear regression analysis was performed to ascertain the relationship of the predictor variables (age groups) with the number of patients and number of consultations (dependent variables).
RESULTS
General characteristics of the database
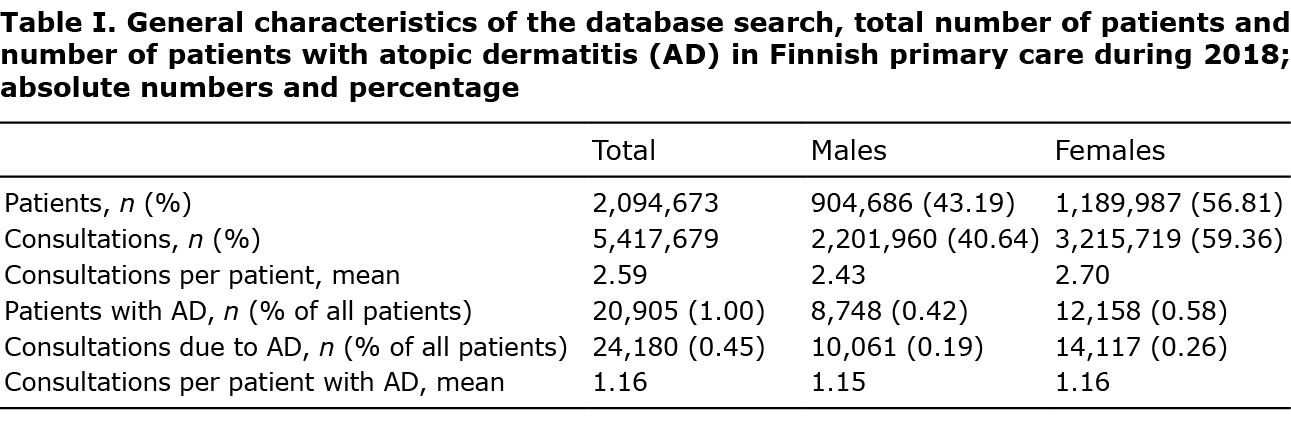
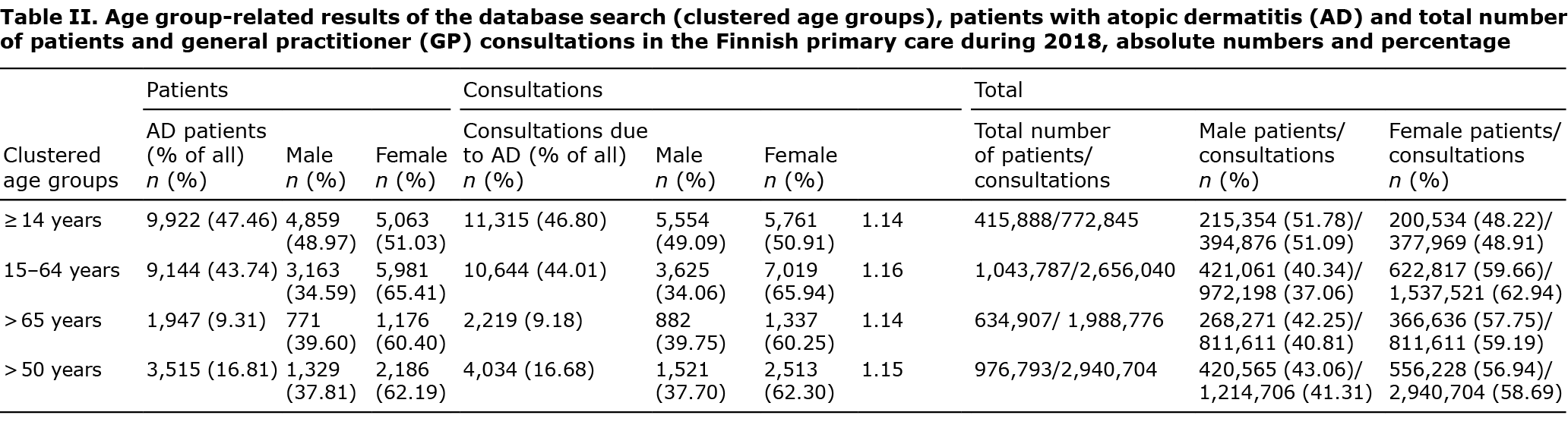
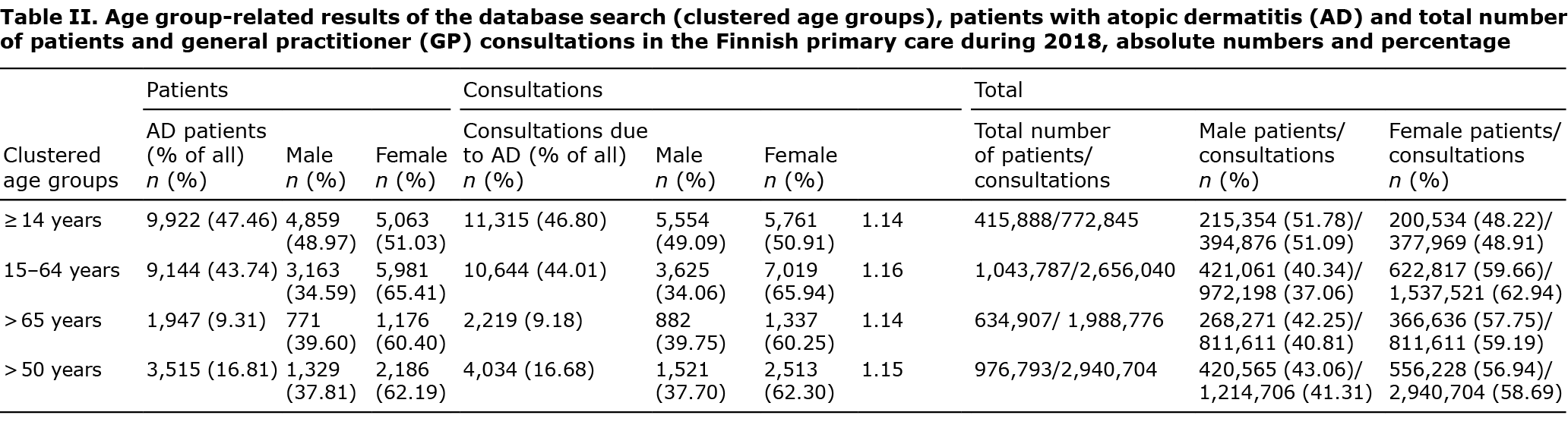
During 2018 there were 2,094,673 patients (males 904,686; 43.19%, females 1,189,987; 56.81%) in the Finnish primary care (Table I). The highest number of patients were in the age group 15–64 years (1,043,878 patients, 49.83%). Patient numbers were smaller in the age groups over 65 years (634,907 patients, 30.31%) and 0–14 years (415,888 patients, 19.86%). Almost half of primary care patients were aged over 50 years (976,793 patients, 46.63%) (Table II).
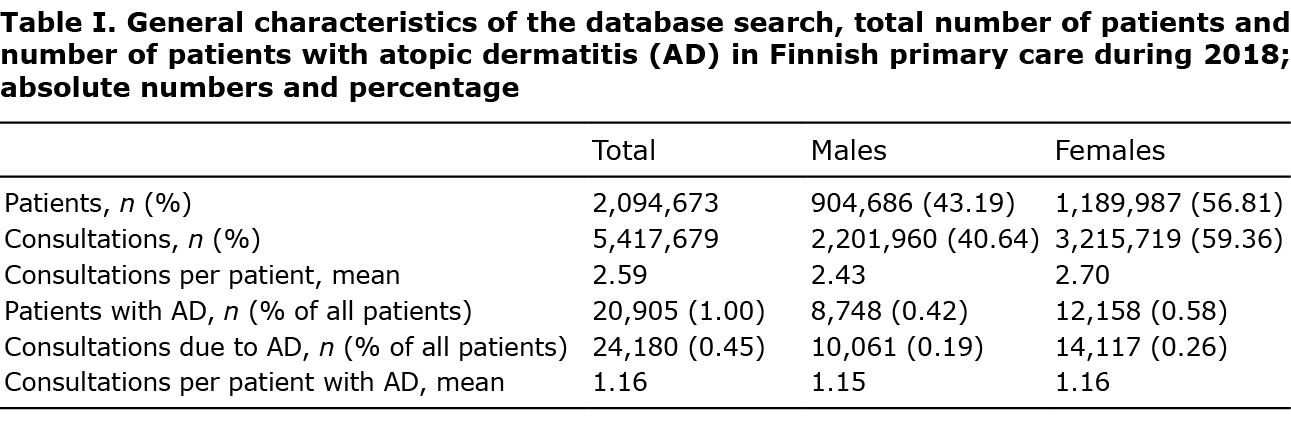
There were 5,417,679 doctors’ outpatient consultations (males 2,201,960; 40.64%, females 3,215,719; 59.36%) corresponding to a mean of 2.59 consultations per patient (males 2.43, females 2.70).
Atopic dermatitis in different age groups
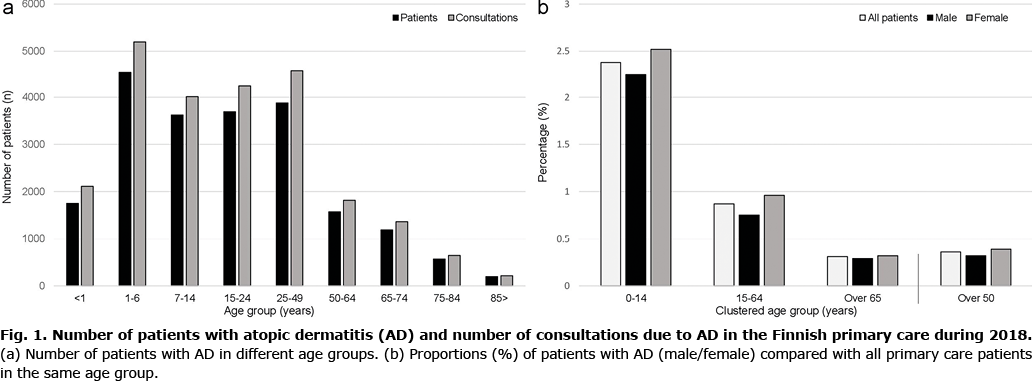
The total number of patients with AD was 20,905 (1.00% of all patients) and there were 24,180 consultations due to AD (0.45% of all consultations). There were considerable age group-dependent differences (Fig. 1a). Numbers of patients with AD were highest in children and decreased stepwise with age. The highest number of patients was in the age group 1–6 years (4,549 patients, 21.76%). However, relatively high numbers of patients were also observed in the age groups 25–49 years (3,883 patients, 18.57%), 15–24 years (3,693 patients, 17.66%) and 7–14 years (3,622 patients, 17.33%). In very small children, aged under 1 year, there were 1,751 patients (8.38%) (Table SI).
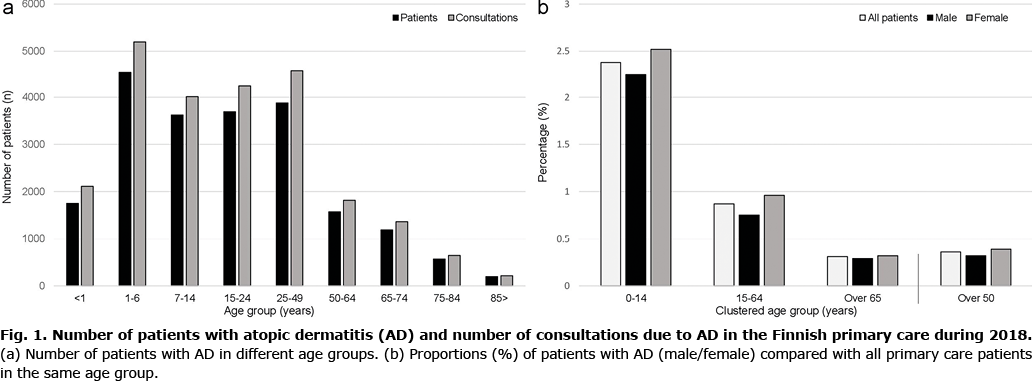
There was a decrease in absolute and proportional patient numbers with increasing age; however, AD was observed in all age groups in primary care. There were 1,568 patients (7.50%) in the age group 50–64 years, 1,183 patients (5.66%) in the age group 65–74 years, 567 patients (2.71%) in the age group 75–84 years, and 197 patients (0.94%) in the age group over 85 years of age. Compared with all patients, the mean number of consultations due to AD per patient was relatively small in all age groups (1.09–1.20) (Table SI).
The clustered age groups showed that there were comparable numbers of patients with AD, both in the age group under 14 years (9.922, 47.46%) and in the age group 15–64 years (9.144, 43.74%). In addition, the data showed that there were 3,515 patients (16.81%) aged over 50 years The lowest numbers of patients were in the age group over 65 years (1,947, 9.31%).
Group comparisons
Compared with all primary care patients, AD accounted for 2.39% in the age group 0–14 years (9,922 patients), for 0.88% in the age group 15–64 years (9,144 patients) and 0.31% in the age group over 65 years (1,947 patients) (Fig. 1b and Fig. S1). Direct comparisons between the groups were not statistically significant regarding the number of patients and number of consultations (p = 0.303, 95% CI 0.847–1.000). In addition, patient numbers compared with consultations was similar in all groups (p = 0.235, 95% CI 0.847–1.000). There were more female patients in all groups, except in the age group under 1 year, but differences were not significant (p = 0.389, 95% CI 0.847–1.000).
In the clustered age groups, there were no significant differences between number of patients (p = 0.199, 95% CI 0.368–1.000) or consultations due to AD (p = 0.224, 95% CI 0.368–1.000). The sex distribution was balanced in the clustered age groups (p = 0.306, 95% CI 0.368–1.000).
Assessing the effects of age groups (predictor variables) the regression analysis indicated a statistically significant association of different age groups with the number of patients with AD (p = 0.032, regression coefficient (standard error of coefficient) –452.75 (170.19), 95% CI –855.18 to –50.32) and number of consultations (p = 0.030, regression coefficient –482.62 (177.55), 95% CI –902.45 to –62.79). This explains the observed relationship of patient numbers with age groups and the decrease with increasing age. There were no differences in age group-related sex distribution in the regression analysis (p = 0.588, regression coefficient –0.002 (0.001), 95% CI –0.004–0.000).
DISCUSSION
The database of the Finnish Institute for Health and Welfare provided a comprehensive and nationwide picture of age-related distribution of AD in Finnish primary care. These observations are important, because the prevalence of AD in Finland is among the highest worldwide and the database of a centralized healthcare system may offer representative data concerning the burden of AD in primary care and in different age groups. Reasons for the relatively high prevalence of AD in Finland and other industrialized countries (10–20%) have remained unclear, but the strong genetic background makes environmental factors most likely responsible for the increase over recent decades (7). In this respect, factors such as reduced childhood infections (drugs, vaccination programmes), immunological stimulation and dysfunctional development (Th2 shift, changes in innate immunity), increased hygiene (skin and gut microbiome) and other environmental factors (allergen exposures, breastfeeding, humidity, pollutants, urban vs rural living, diet, etc.) have been investigated (1, 3).
The results of the current study show that, concerning outpatient visits in the Finnish primary care, AD is not limited to children or younger patients, but is prevalent in all age groups although it decreases proportionally with age. For example, a high number of patients with AD (7,576 patients, 36.24%) were in the age groups of adults and younger adults (15–50 years). Of note was that 16.81% of all patients with AD were aged 50 years or older, also indicating a relevant burden in older patients. The results of the current study also show that AD represents a frequent diagnosis in primary care, corresponding to 1.00% of all Finnish GP’s patients. The proportion of patients with AD was even higher in the clustered age group of 0–14 years (2.39%). Regarding skin-related conditions, AD was the most frequent diagnosis recorded by GPs; however, compared with the most frequent consultation causes, arterial hypertension (8.24%), acute respiratory infection (7.96%) and lower back pain (5.81%), the proportion of patients with AD was considerably lower (12). The number of consultations due to AD per patient was similar in all patient groups (1.09–1.20), and was noticeably smaller than in all diagnoses of primary care (2.43–2.70). This might be explained by the fact that, in Finland, mild and moderate AD is mostly managed in primary care and cases of moderate to severe AD are referred to specialist care (13).
Al-Naqeeb et al. (15) found a large childhood AD burden in primary care in the USA. The authors observed a prevalence rate of 24% in children aged 0–5 years. Abuabara et al. (16) showed, in a population-based study of primary care in the UK, that the cumulative lifetime prevalence of AD was 9.9% and that active disease was highest among children and older adults. The current study made similar observations, that the absolute patient numbers are highest in children and young adults, but there were also relatively high numbers in older age groups. For example, there were 1,947 patients with AD (9.31% of all patients with AD) aged > 65 years, accounting for 0.31% of all primary care patients in this age group. De Lusignan et al. (17) found in a population-based cohort study from the UK that AD burden in primary care increased during the years 2009–2018. The authors discussed whether primary care resources have been adequately modified to address a growing burden of AD in primary care and in age groups other than children. The study also showed that AD-associated specialist referrals were greatest in the age group > 50 years and lowest in individuals of lower socioeconomic status, regardless of a higher rate of primary care consultations. We could not retrieve information about AD patient characteristics in Finnish primary care based on the current database study. However, recent reports of the increasing prevalence and number of AD-related consultations in primary care show similar results to the current study observations, and may increase the need in educational measures and treatment resources regarding AD (18).
In many cases, AD develops in adults, and recent studies have shown that the main burden of AD maybe shifting from childhood towards young adulthood (19). Lee et al. carried out a systematic meta-analysis of AD prevalence in the USA and showed a 26.1% adult-onset rate with distinct clinical characteristics compared with child-onset AD (20). The current study results show, in a similar manner, that a relatively high proportion of patients with AD (36.23% of all patients with AD) in Finnish primary care were in the age group 15–49 years. Many of these patients are likely to experience adult-onset AD, which has a high population-based prevalence (7). Vakharia et al. (21) estimated the prevalence of adult-onset AD in the USA to be approximately 7%, comprising 20–25% of all patients with AD.
The current study did not find statistically significant sex differences, but the number of female patients was higher in all age groups, except for patients <1 year of age. This could have been explained by the generally higher number of female patients in primary care. Recent epidemiological studies have indicated a relatively balanced sex distribution in AD and different age groups (22). Chiesa Fuxench et al. (23) showed, in a cross-sectional study from the USA, a high prevalence of AD in adults (7.3%), but there were no sex differences. However, there have been studies of concomitant psychiatric diseases, which have shown a female dominance regarding depression and anxiety and other psychiatric comorbidities (24–26). In children < 1 year of age, a predominance of the male sex has been reported, as well as an early-onset, severe disease course and an association with asthma (27). Similar results were found regarding the number of patients in Finnish primary care. There were more male patients in the age group < 1 year of age (males/females 58.77/41.23%). In all other age groups, there were higher proportions of females. Dezoteux et al. (28) retrospectively studied the clinical pattern and phenotype of AD in adults > 45 years of age and showed that demographic characteristics were similar to younger adults, and that the sex distribution was balanced, which is in line with the observations of the current study.
In patients > 65 years, there was a relatively high percentage of females (males/females 39.60/60.40%) in the database. There is only a limited amount of data regarding demographic characteristics of AD in the elderly population in primary care (29, 30). The current results showed a considerable number of patients with AD in older age groups, and since there have been indications of a shift of AD burden to older age, the current results are important in understanding the age-related distribution in primary care (31).
Study limitations
The main limitation of this study is that the results are based on database information and that AD diagnosis could not be verified from patient records. This could have led to underestimation or overestimation of distribution of AD due to information bias. Other limitations are linked to classification, because non-specialists recorded the diagnosis, and the database did not include subgroup diagnoses. For example, patients with AD could have been classified under eczematous eruptions (ICD-10 code L30). In addition, the database comprised only information about GP visits, but not visits to nurses or other healthcare specialists, which are essential in primary care (32). Another limitation was that the database discriminated explicit age groups and thus subgroups could not be analysed. For example, there have been reports of specific differences in age-related subgroups of adult AD, and thus it would have been interesting to further subdivide the groups of young adults (25–49 years) and older adults (50–64 years) (7). The database did not include information about the age distribution in specified AD age groups, and thus some parameters of descriptive statistics (e.g. standard deviation (SD)) could not be calculated.
Conclusion
AD is a frequent diagnosis in Finnish primary care and the most common skin-related cause of consultation (33, 34). While AD was previously regarded as a skin disease of childhood or of younger age, recent studies have also shown high prevalence rates in adults (35). Based on nationwide database information, the current study observed that AD is prevalent in all age groups of Finnish primary care and relatively frequent in older age groups (e.g. over 50 years of age). Thus, the burden is not limited to children and young adults and may be shifting to older age groups. More studies are needed to investigate the demographic and phenotypic characteristics of AD in adults and elderly populations in primary care.
ACKNOWLEDGEMENTS
The authors thank medical statisticians Olavi Koivisto and Ville Kinnula, University of Helsinki, Finland, for their very valuable support.
The authors have no conflicts of interest to declare.
REFERENCES
- Weidinger S, Novak N. Atopic dermatitis. Lancet 2016; 387: 1109–1122.
- Landis ET, Davis SA, Taheri A, Feldman SR. Top dermatologic diagnoses by age. Dermatol Online J 2014; 20: 22368.
- Hadi HA, Tarmizi AI, Khalid KA, Gajdács M, Aslam A, Jamshed S. The epidemiology and global burden of atopic dermatitis: a narrative review. Life (Basel) 2021; 11: 936.
- Pols DHJ, Nielen MMJ, Korevaar JC, Bindels PJE, Bohnen AM. Reliably estimating prevalences of atopic children: an epidemiological study in an extensive and representative primary care database. NPJ Prim Care Respir Med 2017; 27: 23.
- Deo MS, Kerse N, Vandal AC, Jarret P. Dermatological disease in the older age group: a cross-sectional study in aged care facilities. BMJ Open 2015; 5: e009941.
- Blume-Peytavi U, Kottner J, Sterry W, Hodin MW, Griffiths TW, Watson RE et al. Age-associated skin conditions and diseases: current perspectives and future options. Gerontologist 2016; 56: S230–S242.
- Kiiski V, Salava A, Susitaival P, Barnhill S, Remitz A, Heliovaara M. Atopic dermatitis in adults: a population-based study in Finland. Int J Dermatol 2022; 61: 324–330.
- Chan LN, Magyari A, Ye M, Al-Alusi NA, Langan SM, Margolis D et al. The epidemiology of atopic dermatitis in older adults: a population-based study in the United Kingdom. PLoS One 2021; 16: e0258219.
- Croce EA, Lopes FCPS, Ruth J. Interventions to improve primary care provider management of atopic dermatitis: a systematic review. Pediatr Dermatol 2021; 38: 1004–1011.
- Benton EC, Kerr OA, Fisher A, Fraser SJ, McCormack SK, Tidman MJ. The changing face of dermatological practice: 25 years’ experience. Br J Dermatol 2008; 159: 413–418.
- Kerr OA, Tidman MJ, Walker JJ, Aldridge RD, Benton EC. The profile of dermatological problems in primary care. Clin Exp Dermatol 2010; 35: 380–383.
- Database of the Finnish Institute for Health and Welfare (THL). Avohilmo: ICD-10. 2020. [accessed April 1, 2021]. Available from: https://sampo.thl.fi/pivot/prod/fi/avo/perus06/summary_icd1001.
- Antti A, Salava A, Perälä M, Pelkonen AS, Mäkelä MJ, Remitz A. Are infants and toddlers with moderate-to-severe atopic dermatitis undertreated? Experiences of a Finnish Tertiary Care Hospital. Acta Derm Venereol 2021; 101: adv00368.
- World Bank Open Data; population of Finland 2018. [accessed April 1, 2021] Available from: https://data.worldbank.org/indicator/SP.POP.TOTL?locations=FI.
- Al-Naqeeb J, Danner S, Fagnan LJ, Ramsey K, Michaels L, Mitchell J et al. The burden of childhood atopic dermatitis in the primary care setting: a report from the Meta-LARC consortium. J Am Board Fam Med 2019; 32: 191–200.
- Abuabara K, Magyari A, McCulloch CE, Linos E, Margolis DJ, Langan SM. Prevalence of atopic eczema among patients seen in primary care: data from the health improvement network. Ann Intern Med 2019; 170: 354–356.
- de Lusignan S, Alexander H, Broderick C, Dennis J, McGovern A, Feeney C et al. Patterns and trends in eczema management in UK primary care (2009–2018): a population-based cohort study. Clin Exp Allergy 2021; 51: 483–494.
- Fleming P, Yang YB, Lynde C, O’Neill B, Lee KO. Diagnosis and management of atopic dermatitis for primary care providers. J Am Board Fam Med 2020; 33: 626–635.
- Kim JP, Chao LX, Simpson EL, Silverberg JI. Persistence of atopic dermatitis (AD): a systematic review and meta-analysis. J Am Acad Dermatol 2016; 75: 681–687.e11.
- Lee HH, Patel KR, Singam V, Rastogi S, Silverberg JI. A systematic review and meta-analysis of the prevalence and phenotype of adult-onset atopic dermatitis. J Am Acad Dermatol 2019; 80: 1526–1532.e7.
- Vakharia PP, Silverberg JI. Adult-onset atopic dermatitis: characteristics and management. Am J Clin Dermatol 2019; 20: 771–779.
- Mathiesen SM, Thomsen SF. The prevalence of atopic dermatitis in adults: systematic review on population studies. Dermatol Online J 2019; 25: 13030/qt6nj0x5k0.
- Chiesa Fuxench ZC, Block JK, Boguniewicz M, Boyle J, Fonacier L, Gelfand JM. Atopic dermatitis in America study: a cross-sectional study examining the prevalence and disease burden of atopic dermatitis in the US adult population. J Invest Dermatol 2019; 139: 583–590.
- Hsu DY, Smith B, Silverberg JI. Atopic dermatitis and hospitalization for mental health disorders in the United States. Dermatitis 2019; 30: 54–61.
- Mina S, Jabeen M, Singh S, Verma R. Gender differences in depression and anxiety among atopic dermatitis patients. Indian J Dermatol 2015; 60: 211.
- Sandhu JK, Wu KK, Bui TL, Armstrong AW. Association between atopic dermatitis and suicidality: a systematic review and meta-analysis. JAMA Dermatol 2019; 155: 178–187.
- Amat F, Soria A, Tallon P, Bourgoin-Heck M, Lambert N, Deschildre A. New insights into the phenotypes of atopic dermatitis linked with allergies and asthma in children: an overview. Clin Exp Allergy 2018; 48: 919–934.
- Dezoteux F, Astrid B, Chuffard M, Drumez E, Azib S, Staumont-Sallé D. Atopic dermatitis in elderly adults. Eur J Dermatol 2019; 29: 371–374.
- Bylund S, Kobyletzki LB, Svalstedt M, Svensson Å. Prevalence and incidence of atopic dermatitis: a systematic review. Acta Derm Venereol 2020; 100: adv00160.
- Williamson S, Merritt J, De Benedetto A. Atopic dermatitis in the elderly: a review of clinical and pathophysiological hallmarks. Br J Dermatol 2020; 182: 47–54.
- Chan AR, Sandhu VK, Drucker AM, Fleming P, Lynde CW. Adult-onset atopic dermatitis: presentations and progress. J Cutan Med Surg 2020; 24: 267–272.
- Ersser SJ, Lattimer V, Surridge H, Brooke S. An analysis of the skin care patient mix attending a primary care-based nurse-led NHS walk-in centre. Br J Dermatol 2005; 153: 992–996.
- Schofield JK, Fleming D, Grindlay D, Williams H. Skin conditions are the commonest new reason people present to general practitioners in England and Wales. Br J Dermatol 2011; 165: 1044–1050.
- Salava A, Oker-Blom A, Remitz A. The spectrum of skin-related conditions in primary care during 2015–2019 – a Finnish nationwide database study. Skin Health Dis 2021; 1: e53.
- Silverberg JI. Public health burden and epidemiology of atopic dermatitis. Dermatol Clin 2017; 35: 283–289.
![]() , Ruut Rieppo, Antti Lauerma and Ville Salo
, Ruut Rieppo, Antti Lauerma and Ville Salo