Psoriasis is a chronic inflammatory skin disease imparting increased risk of cardiovascular diseases. Until now, few studies have reported an increased incidence of ophthalmological retinal vasculopathy in individuals with psoriasis. This study aimed to investigate the association between psoriasis and retinal vein occlusion in the Korean population. Data collected by the National Health Insurance Service between 2009 and 2015 in Korea were analysed. Participants who underwent national health examinations from 2009 to 2012 were enrolled in this study and were divided into either the psoriasis group (n = 3,088) or the control group (n = 465,205). All occurrences of retinal vein occlusion were observed, and the incidence rate of retinal vein occlusion was compared between the psoriasis and control groups. A Cox proportional hazards regression analysis was used to assess the association between psoriasis and newly developed retinal vein occlusion. During a mean 4.37-year follow-up period, 2,034 patients developed retinal vein occlusion. According to multivariable Cox proportional hazard models, individuals with psoriasis had a significantly higher risk of retinal vein occlusion compared with controls (hazard ratio 1.72, 95% confidence interval 1.18–2.51) after adjustments for covariates. This study found that psoriasis was positively associated with retinal vein occlusion.
Key words: epidemiology; incidence; psoriasis; retinal vein occlusion; risk.
Accepted Aug 11, 2022; Epub ahead of print Aug 11, 2022
Acta Derm Venereol 2022; 102: adv00767.
DOI: 10.2340/actadv.v102.2299
Corr: Young Bok Lee, Department of Dermatology, Uijeongbu St Mary’s Hospital, College of Medicine, The Catholic University of Korea, 271 Cheon Bo-ro, Uijeongbu, Gyeonggi-Do, 11765, Republic of Korea. E-mail: lyb80@catholic.ac.kr
SIGNIFICANCE
Psoriasis is a chronic inflammatory skin disease with various multi-systemic complications. This study investigated the association between psoriasis and retinal vein occlusion. Data collected by the National Health Insurance Service between 2009 and 2015 in Korea were analysed, dividing participants into either the psoriasis group or the control group. All occurrences of retinal vein occlusion were observed and the incidence rates between the 2 groups were compared. Statistical analysis showed that individuals with psoriasis had 1.72 times higher risk of retinal vein occlusion compared with controls.
INTRODUCTION
Psoriasis is considered a systemic disease and is associated with various comorbidities, such as cardiovascular disease, stroke, hypertension, dyslipidaemia, diabetes, and obesity (1–3). Therefore, cardiovascular complications are a problem in individuals with psoriasis. However, relatively few studies have focused on microvascular complications compared with macrovascular complications.
Retinal vein occlusion is a heterogeneous group of disorders that impairs venous return from the retinal circulation (4). Retinal vein occlusion causes visual impairment, with macular oedema and neovascularization of the retina and optic disc, which lead to vitreous haemorrhage, retinal detachment, and neovascular glaucoma (4). The worldwide prevalence of branch retinal vein occlusion is estimated at 0.4%, while that of central retinal vein occlusion is approximately 0.08% with an equal distribution between males and females and increased risk with older age (5). The mean incidence rate of retinal vein occlusion in Korea has been reported as 48.09 per 100,000 person-year, with a peak in the late 70s, and females showed a 1.24-times higher incidence rate compared with males (6). To date, the comorbidities of retinal vein occlusion have not been evaluated in any previous Korean study.
Retinal vein occlusion is known to develop at an elderly age and is associated with typical atherosclerosis risk factors (7). It is also caused by inflammation, vasospasm, or compression (8). Therefore, the chronic autoimmune inflammatory diseases are characterized in retinal vein occlusion. In branch retinal vein occlusion, major risk factors are arterial hypertension, arteriosclerosis, and diabetes mellitus (4). In addition, thrombophilia and homocystinuria are known to increase the risk of retinal vein occlusion (9). Considering that psoriasis is a chronic inflammatory disease and associated with metabolic syndrome, there is also the possibility of an association between psoriasis and retinal vein occlusion (10). Recently, a Taiwan study reported increased risk of retinal vascular (both arterial and venous) occlusion in individuals with psoriasis (11). Visual impairment or even blindness due to retinal vein occlusion is a very important complication, and more research on this association is needed to predict and educate patients about retinal vein occlusion in individuals with psoriasis.
The aim of this study was to investigate the association between psoriasis and retinal vein occlusion using Korean Health Insurance Review and Assessment Service data obtained from 2002 to 2015. Since Koreans are obliged to join the National Health Insurance Program, and information from their visits to health institutions and insurance claims is stored in this system, this database is suitable for obtaining a national level of epidemiological information on psoriasis and retinal vein occlusion.
MATERIALS AND METHODS
Data source and study population
This was a nationwide population-based retrospective cohort study using the Korean National Health Insurance Service (KNHIS) Claims Database (in which diagnoses are recorded using the International Classification of Diseases, Tenth Revision (ICD-10) code), which contains all claims data for the KNHIS programme, the Korean Medical Aid programme, and long-term care insurance from 1 January 2002 until 31 December 2015. The KNHIS is a universal healthcare system that provides almost 99% coverage for the entire Korean population. The computerized KNHIS database contains almost all patient medical data (12). The current study used a random sample of 1 million people (representing 2% of the total population) among the KNHIS database to gather data for analysis. KNHIS staff confirmed that multi-level sampling is a representative group of the Korean population from 2002 to 2015 (13). Each patient’s information was anonymized to protect individual privacy. The study was approved by the Institutional Review Board and the ethics committee of Uijeongbu St. Mary’s Hospital at The Catholic University of Korea (UC22ZISI0032). The Institutional Review Board at the Korea Centers for Disease Control and Prevention approved the protocol according to the principles of the Declaration of Helsinki. Anonymized and de-identified information was used for analysis, and informed consent was not required due to the retrospective nature of this study.
Study population and design
The study is designed as a nationwide population-based prospective cohort study. All participants who underwent health screening from January 2009 to December 2012 (n = 484,410) were included. Participants younger than 20 years (n = 1,555) were excluded. The year the participant underwent the health examination was considered the index year of the participant. To evaluate the association between retinal vein occlusion and psoriasis, patients who had been diagnosed with retinal vein occlusion prior to the index year were excluded (n = 2,187). Individuals who died within 1 year of the health examination were also excluded (n = 1,913). After excluding participants with missing values of any of the covariables (n = 10,462), our analysis was conducted on a total of 468,293 participants. Death of the participants was censored. The development of retinal vein occlusion was observed from the index year until 31 December 2015 (Fig. S1).
Definition of the psoriasis group
Of the 468,293 participants who underwent a national health examination from 2009 to 2012, individuals with psoriasis were defined as those who visited an outpatient clinic and received treatment under the diagnosis of psoriasis (ICD-10 code L40.0, L40.1, L40.2, L40.3, L40.4 L40.5, L40.8, and L40.9). In total, 3,088 participants were placed in the psoriasis group, and the other 465,205 individuals were classified in the control group.
Primary outcome of incidence of retinal vein occlusion
The incidence of retinal vein occlusion was observed from the index year to December 2015 in all participants (n = 468,293). Newly developed retinal vein occlusion was defined when a patient visited an ophthalmology clinic and was treated for a diagnosis of retinal vein occlusion (ICD-10 code H34.8) without a prior history of retinal vein occlusion before the index year. The primary endpoint was newly diagnosed retinal vein occlusion that occurred between the baseline visit and the follow-up visit until 31 December 2015.
Measurements from the health examination
Enrolees in the National Health Insurance Corporation are recommended to undergo a standardized medical examination every 2 years. These medical examinations include measurements of height, weight, waist circumference, and blood pressure and laboratory tests such as fasting glucose, total cholesterol, high-density lipoprotein cholesterol, and urinalysis. Health-related behaviours (such as smoking, drinking, and physical activity) were collected using standardized self-reporting questionnaires. Age and sex data were obtained for all participants. Anthropometric measurements were performed while the patients wore light clothing. Body mass index (BMI) was calculated as the participant’s weight (in kg) divided by the square of the participant’s height (in m). Blood pressure was measured while the individual was seated after resting for at least 5 min. Smoking status was categorized as never smoker, ex-smoker, or current smoker. Alcohol drinking status was defined as non-drinker, mild drinker, or heavy drinker based on a question regarding frequency of alcohol consumption per week. The participants’ income levels were dichotomized at the lowest 20%. Blood samples were drawn after an overnight fast and were assessed for serum levels of glucose and total cholesterol. The hospitals in which the health examinations were performed were certified by the KNHIS and are subject to regular quality control.
Baseline comorbidities and subgroup classifications
Baseline comorbidities were obtained from the health examination database and were assessed during the screening period from 2009 to 2012. Baseline characteristics of the comorbidities were extracted from the medical claims according to ICD-10 codes, prescription codes, and procedure codes. The study also included diabetes mellitus, hypertension, and dyslipidaemia diagnoses. A diagnosis of type 2 diabetes was confirmed by the ICD-10 codes E11–E14 and prescription of antidiabetic drugs (sulphonylureas, metformin, meglitinides, thiazolidinediones, dipeptidyl peptidase-4 inhibitors, α-glucosidase inhibitors, or insulin) or fasting blood sugar ≥126 mg/dl. Presence of hypertension was defined as at least 1 claim per year for prescription of an antihypertensive agent under ICD-10 codes I10–13 and I15 or systolic/diastolic BP ≥140/90 mmHg. The presence of dyslipidaemia was defined as at least 1 claim per year for prescription of an antihyperlipidaemic agent under ICD-10 code E78 or total cholesterol level ≥240 mg/dl.
Statistical analysis
When presenting the baseline characteristics, the continuous variable was marked as mean with SD and was compared between groups using Student’s t-test. The categorical variables were presented as numbers and percentages and were analysed using a χ2 test. The incidence rate of retinal vein occlusion was calculated by dividing the number of incident cases by the total follow-up period and was expressed as per 1,000 person-years. A Cox proportional hazards regression analysis was used to assess the association between psoriasis and newly developed retinal vein occlusion. The hazard ratio (HR) and 95% confidence interval (CI) values for retinal vein occlusion in individuals with psoriasis were calculated with a reference of non-psoriasis individuals. In Model 1, only 2 variables (psoriasis and retinal vein occlusion) were used for univariate analysis. In Model 2, age and sex were considered confounding variables. In addition, in Model 3, age, sex, BMI, smoking status, alcohol consumption, physical activity, income level, diabetes mellitus, hypertension, and dyslipidaemia were adjusted as confounding variables. Subgroup analysis was conducted on the underlying characteristics, and Cox proportional hazard regression analysis was conducted to analyse the occurrence rates of both psoriasis and retinal vein occlusion between the subgroups with adjustment for age, sex, BMI, smoking status, alcohol consumption, physical activity, income level, diabetes mellitus, hypertension, and dyslipidaemia.
The cumulative incidence of retinal vein occlusion in the presence of psoriasis was presented using a Kaplan–Meier curve. The proportional hazards assumption was tested through using Schoenfeld residuals. A log-rank test was also performed to analyse the differences between individuals with psoriasis and controls. Statistical significance was defined as a 2-sided p-value < 0.05. Tukey’s method was used for multiple mean comparisons of groups. All statistical analyses were performed using SAS software (ver. 9.4; SAS Institute, Cary, NC, USA) and R programming, version 3.1.0 (The R Foundation for Statistical Computing, Vienna, Austria; http://www.R-project.org).
RESULTS
Baseline characteristics of the study population
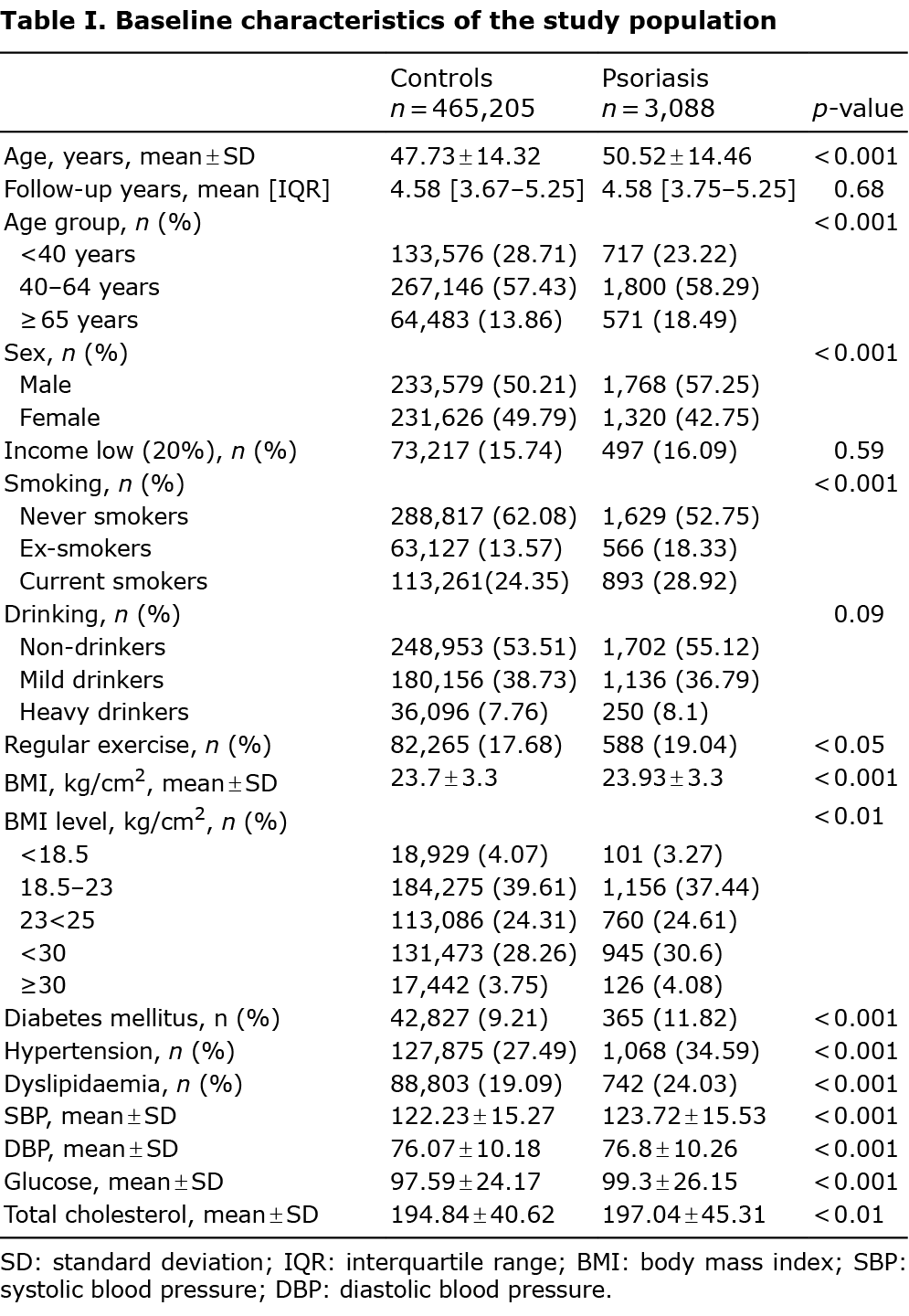
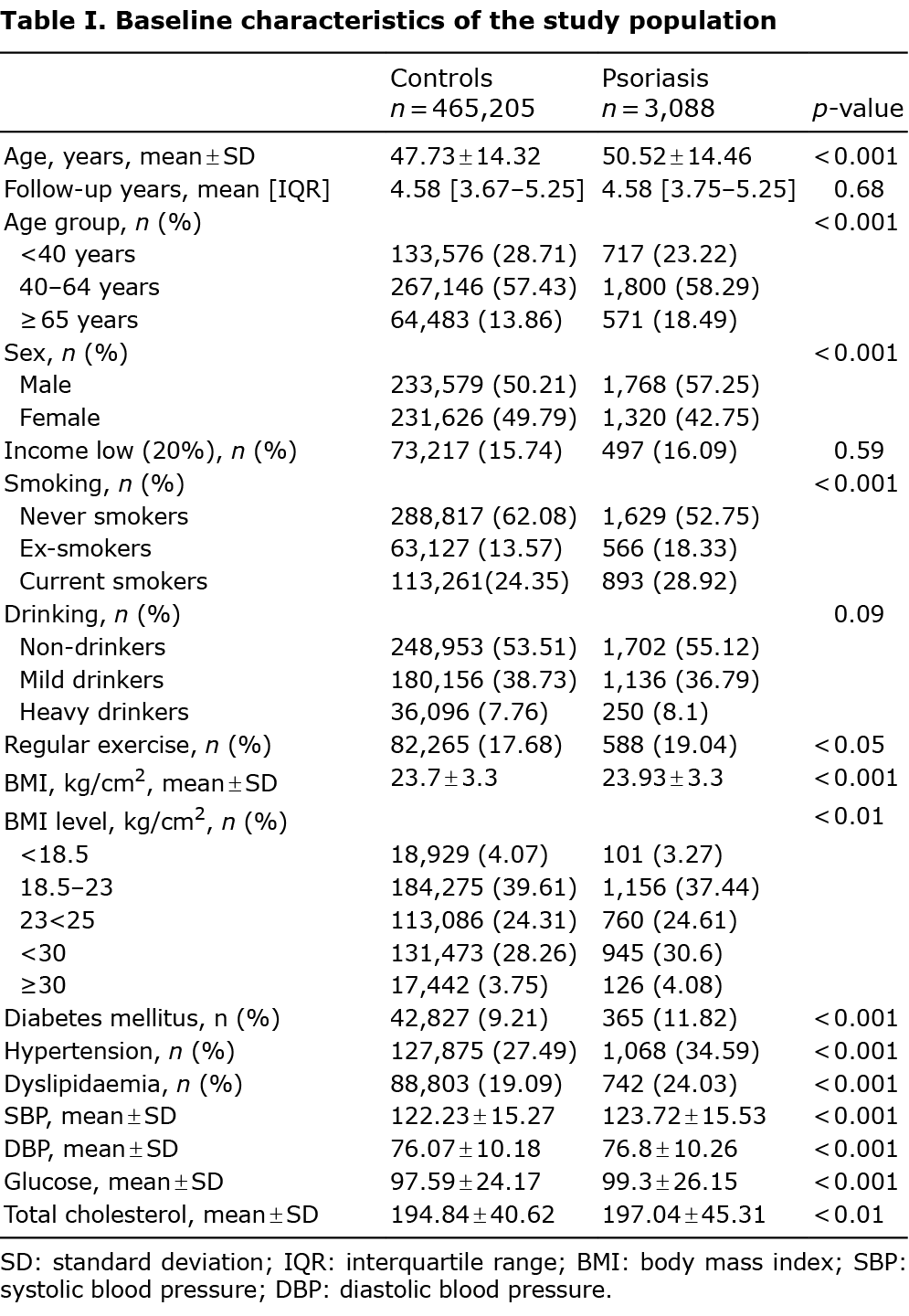
The participants (n = 468,293) were divided into a psoriasis group (n = 3,088) and a control group (n = 465,205). The baseline characteristics of the participants are shown in Table I. Patients with psoriasis were older (mean age 50.5 ± 14.5 years) with a higher proportion of males (57.3%) than in the non-psoriasis group. Patients with psoriasis were more likely to be current smokers (28.9%) and heavy drinkers (8.1%) than those without psoriasis. Individuals with psoriasis had greater proportions of comorbid diabetes mellitus (11.8%), hypertension (34.6%), and dyslipidaemia (24.0%) than those without psoriasis (all, p < 0.001).
Incidence rates and risks of retinal vein occlusion among the psoriasis group
During a mean follow-up of 4.37 ± 1.1 years, 2,034 patients developed retinal vein occlusion. Twenty-seven cases of retinal vein occlusion occurred in individuals with psoriasis. In addition, 2,007 participants in the control group developed retinal vein occlusion. The incidence rate of retinal vein occlusion per 1,000 person-years was 2.00 (95% CI 1.37, 2.92) in the psoriasis group and was higher than that of the control group, 0.99 (0.95, 1.03). In Model 1, the crude HR for retinal vein occlusion was 2.03 (95% CI 1.39–2.97) in the psoriasis group compared with the controls. After adjustments for age and sex in Model 2 and for age, sex, BMI, income level, smoking status, drinking status, regular exercise frequency, diabetes mellitus, hypertension, and dyslipidaemia in Model 3, the HR for retinal vein occlusion in the psoriasis group was significantly increased compared with that of the controls (HR 1.77, 95% CI 1.21–2.59 in Model 2 and HR 1.72, 95% CI 1.18–2.51 in Model 3, all p < 0.01, Table II) As shown in Fig. 1, the psoriasis group showed an increased incidence probability of retinal vein occlusion after 2 years compared with the controls (Fig. 1).


Subgroup analysis of risk of retinal vein occlusion in individuals with psoriasis
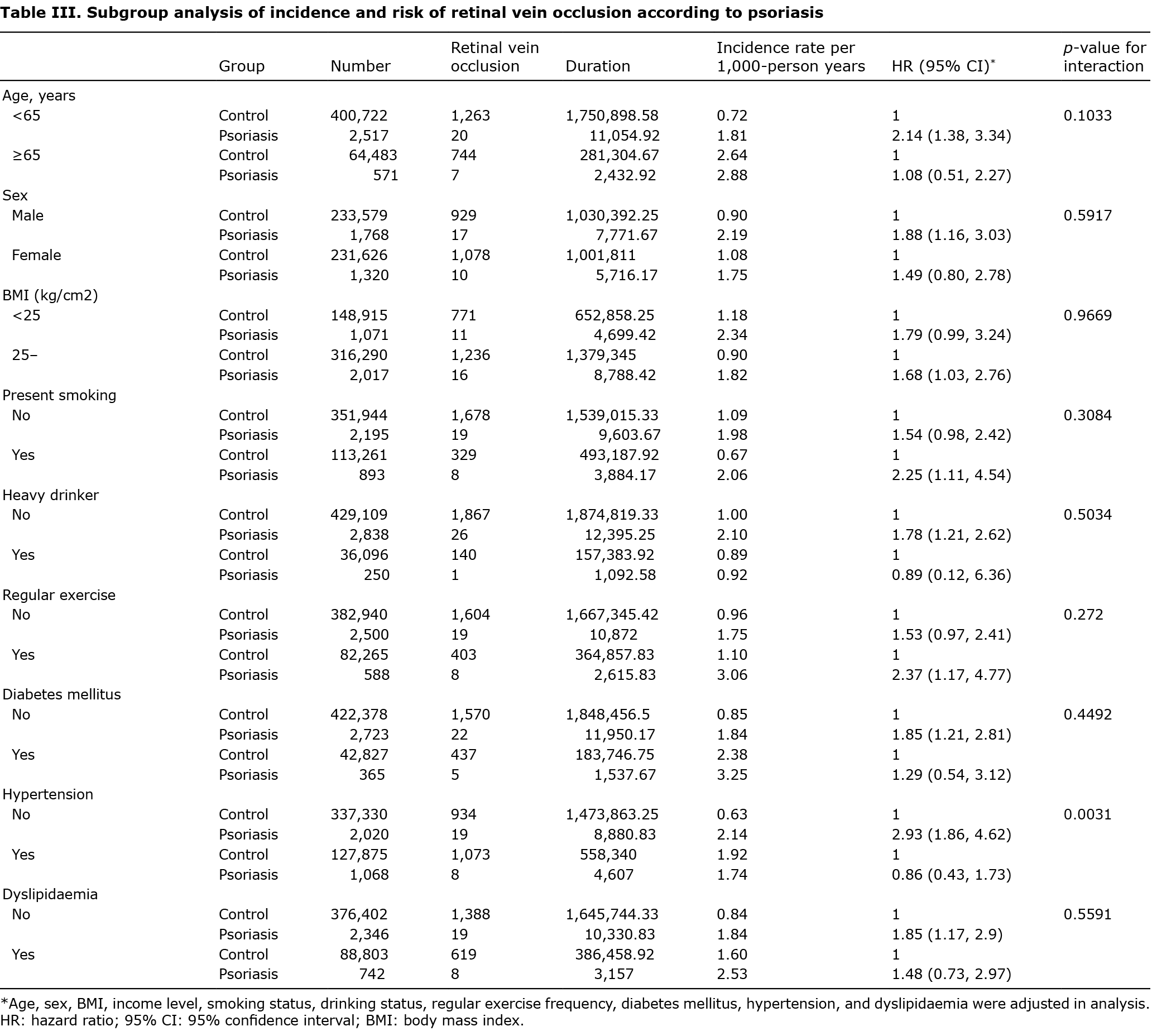
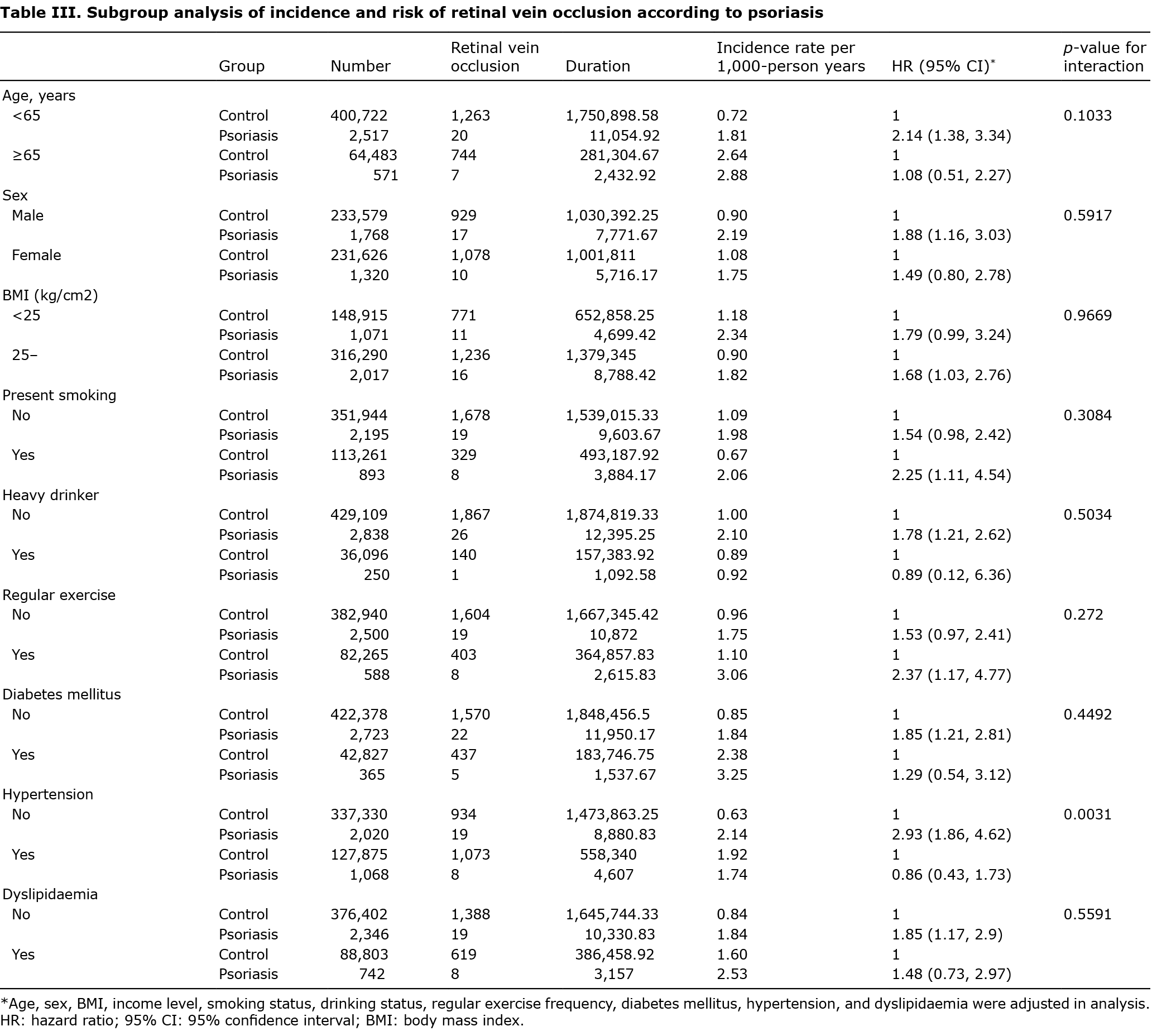
To verify the increased risk of retinal vein occlusion in individuals with psoriasis, subgroup analysis was performed according to age, sex, BMI, smoking status, drinking status, regular exercise frequency, and the presence of comorbid disease including diabetes mellitus, hypertension, and dyslipidaemia (Table III). Regardless of the covariates, the increased risk of retinal vein occlusion was consistent in individuals with psoriasis. The increased risk of retinal vein occlusion was significantly higher in individuals with psoriasis who were <65 years old (HR 2.14, 95% CI 1.38–3.34), male (HR 1.88, 95% CI 1.16-3.03), currently smoking (HR 2.25, 95% CI 1.11–4.54), non-heavy drinking (HR 1.78, 95% CI 1.21–2.62), and regular exercisers (HR 2.37, 95% CI 1.17–4.77) compared with the risk of retinal vein occlusion in control. Increased hazard ratio for retinal vein occlusion in individuals with psoriasis was significantly high when the individuals had no comorbidities, including diabetes mellitus (HR 1.85, 95% CI 1.21–2.81), hypertension (HR 2.93, 95% CI: 1.86–4.62), and dyslipidaemia (HR 1.85, 95% CI 1.17–2.9) compared to controls. The p-value for interaction showed significance in subgroup analysis on hypertension (Table III).
DISCUSSION
This population-based study showed increased risk of retinal vein occlusion in individuals with psoriasis. The findings suggest that psoriasis is an independent risk factor for retinal vein occlusion.
Psoriasis is a chronic inflammatory cutaneous disease. The prevalence of psoriasis varies from 0.14% in East Asia to 1.99% in Australasia.(14) A previous Korean study reported the prevalence of psoriasis in Korea according to the Korean national insurance database was 0.44–0.45% of the general population (15). Psoriasis is associated with increased cardiovascular risk, including myocardial infarction, heart failure, and cardiovascular mortality (16–19). The association between psoriasis and ocular disease has not been well eludicated. Recently, a Taiwan study reported increased risk of retinal vascular (both arterial and venous) occlusion in individuals with psoriasis (11). Although the clinical finding, cause, and prognosis are different between retinal artery occlusion and retinal vein occlusion, the incidence rate of retinal vein occlusion was not specified in the previous Taiwan study (11). The retinal vasculopathy in individuals with psoriasis has not been evaluated in Korea. A previous Korean study reported the development of psoriasis in diabetes patients with diabetic retinopathy (20). That study also included the psoriasis incidence in diabetic patients, although the risk of ophthalmic vascular complications in individuals with psoriasis was not evaluated in the previous Korean study. In this study, the subgroup analysis showed that the psoriasis patients without hypertension, diabetes mellitus, or dyslipidaemia had high risk of retinal vein occlusion compared with individuals without psoriasis. The results might suggest that psoriasis itself is a risk factor for retinal vein occlusion regardless of metabolic syndrome, the powerful risk factor for retinal vein occlusion.
The mechanisms that underlie these associations are not well understood. However, inflammatory status and increased vascular complications in individuals with psoriasis are thought to play roles in retinal vein occlusion.
This association is based on the hypothesis that the 2 conditions share pathological mechanisms as follows. First, psoriasis and retinal vein occlusion share common risk factors, such as hypertension, diabetes mellitus, and hyperlipidaemia. Metabolic syndrome is considered a risk factor for both psoriasis and retinal vein occlusion (4, 21). Secondly, homocysteinaemia is commonly observed in both psoriasis and retinal vein occlusion patients, and the increased level of homocysteine in both populations might play a critical role in the development of both psoriasis and retinal vein occlusion. In individuals with psoriasis, the homocysteine level is significantly higher than that seen in healthy controls (22–24). Homocysteinaemia is also a risk factor for retinal vein occlusion (25, 26). Homocysteine promotes inflammation by activating Th1 and Th17 cells and neutrophils while suppressing regulatory T cells. Moreover, it enhances the production of pro-inflammatory cytokines by inducing nuclear factor kappa B activation, which is critical in the immunopathogenesis of psoriasis and retinal vein occlusion. Thirdly, interleukin-17 is a potential mechanistic link between psoriasis and retinal vein occlusion. Interleukin 17 is produced by Th17 cells and is a pivotal cytokine in the pathogenesis of psoriasis. High serum level of interleukin 17 can disrupt endothelial function and vascular health and result in vascular dysfunction. The pathological role of interleukin 17 is also indicated in retinal vein occlusion (27). Fourthly, tumour necrosis factor alpha, another key cytokine in psoriasis, might be associated with a common pathogenesis of psoriasis and retinal vein occlusion. A previous study reported that anti-tumour necrosis factor alpha treatment improved the symptoms of retinal vein occlusion in patients with rheumatoid arthritis (28). As such, the 2 conditions share a common cytokine that is probably involved in their pathogenesis. Although the complications of retinal vein are severe including vitreous haemorrhage, retinal detachment, neovascular glaucoma, and even visual loss, the vascular alterations can progress without any clinical evidence of ocular inflammation sign (29). Therefore, the recommendation of regular eye examination is considered to be important for individuals with psoriasis.
Study limitations
This study has some limitations. First, psoriasis, retinal vein occlusion, and other comorbidities were defined by claims data from the KNHIS database, which might not have been accurate. Secondly, the severity of the diseases and the types of medications prescribed were not considered in the analysis, so we could have missed some important factors. Thirdly, the data about the articular involvement in individuals with psoriasis and the diagnosis of psoriatic arthritis were analysed in this study. The association between psoriatic arthritis and retinal vein occlusion should be evaluated in further study. Fourthly, lifestyle factors were based on self-report, a problematic aspect given the potential for social desirability bias.
Conclusion
Despite the limitations of this nationwide cohort study, the study found that psoriasis was an independent risk factor for retinal vein occlusion, after adjustment for covariates including diabetes mellitus, hypertension, and dyslipidaemia. Therefore, physicians should recommend regular eye examinations throughout the retina in order to monitor the development of retinal problems in individuals with psoriasis. Further studies are needed to identify the pathological mechanism of increased retinal vasculopathy in individuals with psoriasis with more large-scale study and to identify factors that can predict increased risk of microvascular complications in individuals with psoriasis.
ACKNOWLEDGEMENTS
This study was approved by the Institutional Review Board at Uijeongbu St Mary’s Hospital, The Catholic University of Korea (UC22ZISI0032).
The authors have no conflicts of interest to declare.
REFERENCES
- Michalek IM, Loring B, John SM. A systematic review of worldwide epidemiology of psoriasis. J Eur Acad Derm Venereol 2017; 31: 205–212.
- Egeberg A, Mallbris L, Hilmar Gislason G, Skov L, Riis Hansen P. Increased risk of migraine in patients with psoriasis: a Danish nationwide cohort study. J Amer Acad Dermatol 2015; 73: 829–835.
- Edson-Heredia E, Zhu B, Lefevre C, Wang M, Barrett A, Bushe CJ, et al. Prevalence and incidence rates of cardiovascular, autoimmune, and other diseases in patients with psoriatic or psoriatic arthritis: a retrospective study using Clinical Practice Research Datalink. J Eur Acad Derm Venereol 2015; 29: 955–963.
- Ip M, Hendrick A. Retinal vein occlusion review. Asia Pac J Ophthalmol (Phila) 2018; 7: 40–45.
- Rogers S, McIntosh RL, Cheung N, Lim L, Wang JJ, Mitchell P, et al. The prevalence of retinal vein occlusion: pooled data from population studies from the United States, Europe, Asia, and Australia. Ophthalmology 2010; 117: 313–319.e1.
- Park JY, Park SJ, Byun SJ, Woo SJ, Park KH. Twelve-year incidence of retinal vein occlusion and its trend in Korea. Graefes Arch Clin Exp Ophthalmol 2020; 258: 2095–2104.
- O’Mahoney PR, Wong DT, Ray JG. Retinal vein occlusion and traditional risk factors for atherosclerosis. Arch Ophthalmol 2008; 126: 692–699.
- Yen YC, Weng SF, Chen HA, Lin YS. Risk of retinal vein occlusion in patients with systemic lupus erythematosus: a population-based cohort study. Br J Ophthalmol 2013; 97: 1192–1196.
- Fong AC, Schatz H. Central retinal vein occlusion in young adults. Surv Ophthalmol 1993; 37: 393–417.
- Yen YC, Weng SF, Lai FJ, Lin YS. Risk of retinal vein occlusion in patients with psoriasis: a population-based cohort study. Retina 2015; 35: 1786–1794.
- Dai YX, Tai YH, Lee DD, Chang YT, Chen TJ, Chen MH. Risk of retinal diseases in patients with psoriasis: a population-based cohort study in Taiwan. J Dermatol 2021; 48: 1550–1556.
- Koo BK, Lee CH, Yang BR, Hwang SS, Choi NK. The incidence and prevalence of diabetes mellitus and related atherosclerotic complications in Korea: a National Health Insurance Database Study. PLoS One 2014; 9: e110650.
- Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort Profile: The National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol 2017; 46: e15.
- Parisi R, Iskandar IYK, Kontopantelis E, Augustin M, Griffiths CEM, Ashcroft DM, et al. National, regional, and worldwide epidemiology of psoriasis: systematic analysis and modelling study. BMJ 2020; 369: m1590.
- Lee JY, Kang S, Park JS, Jo SJ. Prevalence of psoriasis in Korea: a population-based epidemiological study using the Korean National Health Insurance database. Ann Dermatol 2017; 29: 761–767.
- Gelfand JM, Neimann AL, Shin DB, Wang X, Margolis DJ, Troxel AB. Risk of myocardial infarction in patients with psoriasis. JAMA 2006; 296: 1735–1741.
- Gelfand JM, Troxel AB, Lewis JD, Kurd SK, Shin DB, Wang X, et al. The risk of mortality in patients with psoriasis: results from a population-based study. Arch Dermatol 2007; 143: 1493–1499.
- Khalid U, Ahlehoff O, Gislason GH, Kristensen SL, Skov L, Torp-Pedersen C, et al. Psoriasis and risk of heart failure: a nationwide cohort study. Eur J Heart Fail 2014; 16: 743–748.
- Mehta NN, Yu Y, Pinnelas R, Krishnamoorthy P, Shin DB, Troxel AB, et al. Attributable risk estimate of severe psoriasis on major cardiovascular events. Am J Med 2011; 124: 775.e1–6.
- Lee JH, Han JH, Han KD, Park YM, Lee JY, Park YG, et al. Psoriasis risk in patients with diabetic retinopathy: a nationwide population-based study. Sci Rep 2018; 8: 9086.
- Fernandez-Armenteros JM, Gomez-Arbones X, Buti-Soler M, Betriu-Bars A, Sanmartin-Novell V, Ortega-Bravo M, et al. Psoriasis, metabolic syndrome and cardiovascular risk factors. A population-based study. J Eur Acad Derm Venereol 2019; 33: 128–135.
- Lin X, Meng X, Song Z. Homocysteine and psoriasis. Biosci Rep 2019; 39: BSR20190867.
- Kim JE, Lee HJ, Lee JS, Whang KU, Park YL, Lee SY, et al. Association between homocysteine levels and psoriasis: a meta-analysis. Ann Dermatol 2019; 31: 378–386.
- Giannoni M, Consales V, Campanati A, Ganzetti G, Giuliodori K, Postacchini V, et al. Homocysteine plasma levels in psoriasis patients: our experience and review of the literature. J Eur Acad Derm Venereol 2015; 29: 1781–1785.
- Abu El-Asrar AM, Abdel Gader AG, Al-Amro SA, Al-Attas OS. Hyperhomocysteinemia and retinal vascular occlusive disease. Eur J Ophthalmol 2002; 12: 495–500.
- Chua B, Kifley A, Wong TY, Mitchell P. Homocysteine and retinal vein occlusion: a population-based study. Am J Ophthalmol 2005; 139: 181–182.
- Li Y, Zhou Y. Interleukin-17: the role for pathological angiogenesis in ocular neovascular diseases. Tohoku J Exp Med 2019; 247: 87–98.
- Kachi S, Kobayashi K, Ushida H, Ito Y, Kondo M, Terasaki H. Regression of macular edema secondary to branch retinal vein occlusion during anti-TNF-alpha therapy for rheumatoid arthritis. Clin Ophthalmol 2010; 4: 667–670.
- Castellino N, Longo A, Fallico M, Russo A, Bonfiglio V, Cennamo G, et al. Retinal vascular assessment in psoriasis: a multicenter study. Front Neurosci 2021; 15: 629401.
![]()