Erythromelalgia is a rare disorder characterized by erythema, warmth, and episodic burning pain of the extremities, which is relieved by cooling and worsened by warming (1). Erythromelalgia is commonly divided into primary and secondary cases. We report here a case of erythromelalgia associated with neuropathy in Sjögren’s syndrome (SS).
CASE REPORT
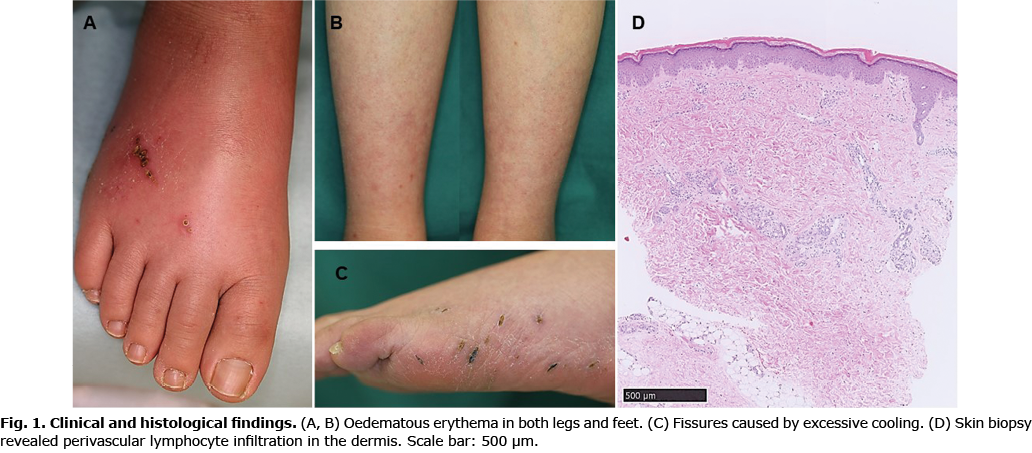
A 35-year-old woman presented with numbness in her limbs, voiding dysfunction, palpitations, tachycardia, and profuse sweating. She was referred to neurology due to worsening symptoms. Antinuclear antibody levels were found to be high in laboratory tests (1: 160; normal range, <1: 40) and an anti-SS-A antibody was positive (683 U/ml; normal range, ≤ 10 U/ml). Salivary gland scintigraphy revealed reduced uptake, and the chewing gum test was positive. A nerve conduction test revealed perceptual neuropathy. The patient was diagnosed with sensory and automatic neuropathy in SS. Subsequently, she had frequent burning pains together with erythema in her legs and feet, and was referred to our Department of Dermatology of Shinshu University Hospital. Physical examination indicated redness, heat, and oedema in both legs and feet (Fig. 1A, B). Excessive cooling caused fissures and ulcers on her feet (Fig. 1C). A dorsal foot skin biopsy revealed perivascular lymphocyte infiltration in the dermis (Fig. 1D). There were no signs of vasculitis. A diagnosis ofsecondary erythromelalgia associated with neuropathy in SS was made. She received 2 courses of intravenous immunoglobulin (400 mg/kg/day for 5 days at 4-week intervals), and oral prednisolone (starting dose 40 mg/day). In addition, pregabalin 600 mg/day, tramadol 150 mg/day, and loxoprofen 180 mg/day were administered to relieve pain. Her symptoms progressively improved once she began receiving therapy. She could continue her everyday activities although she still had mild symptoms.
DISCUSSION
This was a case of secondary erythromelalgia associated with neuropathy in SS. Recent research suggests that erythromelalgia is associated with small fibre neuropathy (SFN) (2). Primary erythromelalgia is linked to the SCN9A mutations that produce SFN (2, 3). SFN selectively damages peripheral Aδ and C fibers, and also the automatic nervous system: the former cause neurological pain, numbness, and burning sensation, and the latter leads to automatic dysfunction. Erythema with warmth is thought to be induced by vasodilation and increased blood flow due to SFN (2). SFN is thought to occur in 5–10% of patients with SS (4). Although there have been few reports of SS-related erythromelalgia, patients with SS may occasionally have erythromelalgia if mild symptoms are included. Erythromelalgia is caused by various diseases (collagen disease, vasculitis, diabetes, sarcoidosis, amyloidosis, and drug-induced, etc.) associated with SFN (5), and it may not be a rare disorder.
No specific and effective therapies exist for erythromelalgia (2). In secondary erythromelalgia, therapy should focus on both the underlying disorders and symptom relief (1). As reported previously, a delayed initiation of therapy can lead to a negative prognosis (6). An early therapeutic intervention may have resulted in an improved outcome in the current case study.
ACKNOWLEDGEMENTS
The authors would like to thank Drs Nonami J and Kido K for their helpful discussions.
The authors have no conflicts of interest to declare.
REFERENCES
- Mann N, King T, Murphy R. Review of primary and secondary erythromelalgia. Clin Exp Dermatol 2019; 44: 477–482.
- Leroux MB. Erythromelalgia: a cutaneous manifestation of neuropathy? An Bras Dermatol 2018; 93: 86–94.
- McDonnell A, Schulman B, Ali Z, Dib-Hajj SD, Brock F, Cobain S, et al. Inherited erythromelalgia due to mutations in SCN9A: natural history, clinical phenotype and somatosensory profile. Brain 2016; 139: 1052–1065.
- Perzyńska-Mazan J, Maślińska M, Gasik R. Neurological manifestations of primary Sjögren’s syndrome. Reumatologia 2018; 56: 99–105.
- Terkelsen AJ, Karlsson P, Lauria G, Freeman R, Finnerup NB, Jensen TS. The diagnostic challenge of small fibre neuropathy: clinical presentations, evaluations, and causes. Lancet Neurol 2017; 16: 934–944.
- Pagani-Estévez GL, Sandroni P, Davis MD, Watson JC. Erythromelalgia: Identification of a corticosteroid-responsive subset. J Am Acad Dermatol 2017; 76: 506–511.e1.