ORIGINAL ARTICLE
Comparison of Perceptions of Skin Condition, Product Use and Allergen Reactivity Between People with Psoriasis and Controls in the European Dermato-Epidemiology Network (EDEN) Fragrance Study
Fortunato CASSALIA1,2, Simone CAZZANIGA1,3, Robert OFENLOCH4, Peter ELSNER5, Margarida GONÇALO6, Marie-Louise SCHUTTELAAR7, Åke SVENSSON8, Elena PEZZOLO1,9, Magnus BRUZE10 and Luigi NALDI1,9
1Centro Studi GISED, Bergamo, 2Dermatology Unit, Department of Medicine, University of Padova, Padua, Italy, 3Inselspital University Hospital of Bern, University of Bern, Bern, Switzerland, 4Section of Occupational Dermatology, Department of Dermatology, University Hospital Heidelberg, Heidelberg, Germany, 5Dermatology, Allergology, Dermatopathology, SRH- Klinikum Gera, Germany, 6Department of Dermatology, Faculty of Medicine, University Hospital, University of Coimbra, Portugal, 7Department of Dermatology, University Medical Center Groningen, Groningen, The Netherlands, 8Department of Dermatology, University Hospital, Lund University, Malmö, Sweden, 9Department of Dermatology, Ospedale San Bortolo, Vicenza, Italy and 10Department of Occupational and Environmental Dermatology, Skåne University Hospital, Malmö, Sweden
Psoriasis, a chronic inflammatory skin disease, goes beyond visible symptoms and affects the general well-being of patients. The aim of this study is to understand how patients with psoriasis perceive their skin characteristics and reactivity to allergens. The study population includes 11,283 participants within the European Dermato-Epidemiology Network (EDEN) Fragrance study, covering several European regions. The study compared perceptions of skin dryness, sensitivity, product avoidance and reactivity to allergens between patients with psoriasis and controls, evaluating the potential influence of psoriasis severity. The results showed that subjects with psoriasis reported dry skin (71.1%) and sensitive skin (49.4%) more often than did controls (51.6% and 38.5%, respectively). Psoriasis patients were more likely to avoid specific products. Interestingly, there were no significant differences in patch-test results between the 2 groups and the severity of psoriasis did not have a consistent impact on these perceptions. In conclusion, people with psoriasis tend to perceive their skin as drier and more sensitive. Notably, the severity of psoriasis did not consistently influence these perceptions and objective reactivity to allergens did not align with subjective perception. Understanding these aspects is crucial for tailoring treatments to improve the well-being of patients with psoriasis, which warrants further research to explore subjective perceptions of skin well-being in patients with psoriasis.
Key words: psoriasis; skin dryness; skin sensitivity; allergen reactivity; patch-test; topical treatment; neuro-immune inflammation.
SIGNIFICANCE
This study examines the question as to whether the perception of skin dryness and sensitivity differs between patients with psoriasis and controls. In this population-based survey (cross-sectional study) of 11,283 participants, subjects with psoriasis reported a higher prevalence of dry (71.1%) and sensitive (49.4%) skin than those without psoriasis (51.6% and 38.5%, respectively). However, no significant differences in patch-test results were observed between the 2 groups. Finally, the study found that people with psoriasis perceived their skin as drier and more sensitive than controls, regardless of psoriasis severity, highlighting the importance of addressing subjective perceptions in treatment strategies.
Citation: Acta Derm Venereol 2024; 104: adv23513. DOI https://doi.org/10.2340/actadv.v104.23513.
Copyright: © Published by Medical Journals Sweden, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Submitted: Oct 13, 2023; Accepted: Jan 30, 2024; Published: Mar 4, 2024
Corr: Luigi Naldi, Department of Dermatology, AULSS8 Berica, Ospedale San Bortolo, viale Rodolfi 37, IT-36100 Vicenza, Italy and Centro Studi GISED, via Carnovali 100/C – 6 piano, IT-24100 Bergamo, Italy. E-mail: luigi.naldi@aulss8.veneto.it; luigi.naldi@gised.it
Competing interests and funding: The authors have no conflicts of interest to declare.
INTRODUCTION
Psoriasis is a chronic, inflammatory skin disease characterized by the presence of red, scaly plaques accompanied by symptoms such as itching, burning and pain (1). Notably, psoriasis is not limited to dermatological implications, as it has been associated with arthritis (2, 3) and other comorbidities, e.g. cardiovascular disease (4–7). The association between psoriasis and mental health should not be overlooked (8). Numerous studies have reported the social, relational, work, and quality of life (QoL) implications of living with psoriasis (9–12). In this scenario, an area of interest focuses on the subjective perception of overall skin well-being reported by people with psoriasis. Most studies have considered itching, and pain associated with skin lesions (13–15). To our knowledge, there is no work to date that has investigated the association of the subjective perception of overall skin dryness or sensitivity, and reactivity to specific allergens in patients with psoriasis. This population-based survey, performed in the context of the European Dermato-Epidemiology Network (EDEN) Fragrance study (16) aimed to comprehensively explore the subjective perception of dry and/or sensitive skin, and avoidance of products of common use in subjects with psoriasis and in people without psoriasis, by using a validated questionnaire, and to assess allergen reactivity using standardized patch-test procedures.
MATERIALS AND METHODS
Study design
The study was approved by the ethics committee of each participating centre. All participants gave written informed consent before starting the interview. The European Dermato-Epidemiology Network (EDEN) Fragrance Study comprised a large descriptive epidemiological survey of the general population conducted in 6 European regions. These included the metropolitan areas of Malmö (Sweden), Thüringen (Germany), and Heidelberg (Germany), as well as the provinces of Groningen (The Netherlands), Bergamo (Italy), and Coimbra (Portugal). The study methods were previously published (17). Briefly, a random sample (age range 18–74 years) was selected from the general population, based on electoral precincts. The study followed a stratified, proportional, random sampling-with-replacement design. The participants were interviewed using a standardized questionnaire and were offered patch-testing to investigate sensitization to various fragrances. We present here the interview data and patch-test results. The full phase of the study was from 20 August 2008 to 10 October 2011. Each potential participant was contacted by letter. Non-responses were followed up with a second and third letter and a telephone call. If no contact was achieved, another individual was randomly selected in the same age and sex strata. The initial contact participation rates ranged from 20.3% to 50.7% depending on the region considered. Psoriasis was defined as a medical diagnosis of the disease ever received in the past. Severe psoriasis was considered as a disease diagnosed by a dermatologist and undergoing systemic therapy. Controls were all the people in the samples not reporting psoriasis. People reporting other skin diseases, such as atopic dermatitis or contact dermatitis, were maintained in the control group.
Data collection
Trained interviewers conducted face-to-face interviews, either at the home of the sampled person or at hospital, based on participant preference. The interview comprised 3 parts, recording demographic data, skin problem history, and exposure to consumer products. Participants were asked about sensitive and dry skin, previous dermatological diagnoses and their treatment, previous allergy tests, and product usage frequency. Questionnaire reliability was assessed on a subsample of 96 individuals, with strong agreement for demographic data and skin-related questions. For exposure frequencies to products, κ statistics ranged from 0.54 to 0.91, mostly exceeding 0.70. A web-based electronic form minimized errors and inconsistencies during data collection. In addition, a random sample (n = 3,119) of subjects were patch-tested with TRUE-test panel 1, 2 and 3 plus fragrance mix II, hydroxyisohexyl 3-cyclohexene carboxaldehyde (HICC), and sesquiterpene lactone mix. A positive patch-test reaction was considered as contact allergy.
Since information on psoriasis severity was not collected in the study, an algorithmic classification of disease severity was used. More specifically, the study considered subjects with moderate-to-severe psoriasis to be those diagnosed and treated by a dermatologist with the use of non-topical (systemic) medications in the previous 12 months (Table SI).
Sample size and data analyses
The study aimed to obtain confidence estimates of rates exceeding 0.5%. Using the Clopper-Pearson confidence interval (CI) method (18), we estimated that a sample size of 12,000 individuals would produce a 95% CI, with a width equal to 0.003 and a relative standard error (SE) of 13% when the sample prevalence was 0.5%. Therefore, we interviewed approximately 2,000 individuals per centre; a total of 12,377 participants. To assess the representativeness of the sample, selected demographic variables of the sample were compared with those of Eurostat 2010 data (19). For the purpose of this analysis, continuous data were categorized using clinically relevant or pre-defined cut-offs and presented as absolute numbers with percentages. Univariate differences of investigated variables between groups of patients were assessed using Pearson’s χ2 test or Fisher’s exact test in places where required. In addition, multivariable logistic regression analysis was performed to control for potential confounding factors, such as sex, age, occupation, marital status, smoking habits, body mass index (BMI), and country of residence (20). The strength of association was expressed in terms of odds ratio (OR) along with its 95% CI and p-value. Patients with missing data were excluded from the analyses. All tests were considered statistically significant at p < 0.05. Analyses were performed using SPSS software v.26.0 (IBM Corp, Armonk, NY, USA).
RESULTS
Demographics and characteristics of the study population
The demographics and general characteristics of the study population is presented in Table I. A larger proportion of individuals in the age group 30–44 was observed among those with psoriasis (27.0%) than controls (24.4%) (p-value 0.02), and the prevalence of psoriasis tended to increase in older age groups. A significant increased prevalence of smokers and ex-smokers in the psoriasis group compared with controls (p < 0.001), and a significant association between psoriasis and higher BMI categories (p < 0.001) were also documented.
| Total | Univariate analysis | Multivariable analysis | ||||||||
| No psoriasis | With psoriasis | p** | OR (95% CI) | p*** | ||||||
| N* | % | N* | % | N* | % | |||||
| Sex | Total | 11,283 | 100 | 10,693 | 94.8 | 590 | 5.2 | |||
| Male | 5,274 | 46.7 | 4,993 | 46.7 | 281 | 47.6 | 0.66 | 1 | ||
| Female | 6,009 | 53.3 | 5,700 | 53.3 | 309 | 52.4 | 1.00 (0.84–1.20) | 0.96 | ||
| Age | 18–29 years | 2,906 | 25.8 | 2,796 | 26.1 | 110 | 18.6 | < 0.001 | 1 | |
| 30–44 years | 3,035 | 26.9 | 2,891 | 27.0 | 144 | 24.4 | 1.49 (1.07–2.08) | 0.02 | ||
| 45–59 years | 2,881 | 25.5 | 2,708 | 25.3 | 173 | 29.3 | 1.98 (1.39–2.82) | < 0.001 | ||
| 60–74 years | 2,461 | 21.8 | 2,298 | 21.5 | 163 | 27.6 | 2.09 (1.33–3.27) | 0.001 | ||
| Occupation | Working | 6,386 | 56.7 | 6,060 | 56.7 | 326 | 55.3 | < 0.001 | 1 | |
| Student | 1,677 | 14.9 | 1,606 | 15.0 | 71 | 12.1 | 1.08 (0.76–1.55) | 0.67 | ||
| Unemployed | 482 | 4.3 | 450 | 4.2 | 32 | 5.4 | 1.21 (0.82–1.79) | 0.33 | ||
| Retired | 1,824 | 16.2 | 1,698 | 15.9 | 126 | 21.4 | 1.00 (0.70–1.42) | 0.98 | ||
| Homemaker | 479 | 4.3 | 468 | 4.4 | 11 | 1.9 | 0.54 (0.28–1.04) | 0.07 | ||
| Other | 420 | 3.7 | 397 | 3.7 | 23 | 3.9 | 0.90 (0.57–1.41) | 0.64 | ||
| Marital status | Married/common law | 6,224 | 55.4 | 5,919 | 55.6 | 305 | 51.8 | 0.07 | 1 | |
| Divorced/widowed | 1,110 | 9.9 | 1,038 | 9.8 | 72 | 12.2 | 1.03 (0.78–1.35) | 0.85 | ||
| Single | 3,899 | 34.7 | 3,687 | 34.6 | 212 | 36.0 | 1.25 (1.00–1.57) | 0.06 | ||
| Smoking habits | Non-smoker | 6,299 | 55.9 | 6,036 | 56.5 | 263 | 44.7 | < 0.001 | 1 | |
| Ex-smoker | 2,439 | 21.6 | 2,267 | 21.2 | 172 | 29.2 | 1.36 (1.10–1.68) | 0.004 | ||
| Smoker | 2,529 | 22.4 | 2,375 | 22.2 | 154 | 26.1 | 1.50 (1.22–1.86) | < 0.001 | ||
| Body mass index (kg/m2) | < 20 | 998 | 8.9 | 960 | 9.0 | 38 | 6.5 | < 0.001 | 0.88 (0.62–1.26) | 0.48 |
| 20–24.9 | 5,399 | 48.1 | 5,128 | 48.2 | 271 | 46.1 | 1 | |||
| 25–29.9 | 3,554 | 31.7 | 3,374 | 31.7 | 180 | 30.6 | 0.96 (0.78–1.18) | 0.72 | ||
| ≥30 | 1,269 | 11.3 | 1,170 | 11.0 | 99 | 16.8 | 1.44 (1.12–1.85) | 0.005 | ||
| 95% CI: 95% confidence interval; OR: odds ratio. | ||||||||||
| *Numbers may not add up to the total due to missing data. **Pearson’s χ2 test. ***Multivariable logistic regression analysis including terms for sex, age, occupation, marital status, smoking habits, body mass index and country of residence. | ||||||||||
Subjective perceptions related to skin conditions and avoidance experience of subjects with and without a lifetime diagnosis of psoriasis
Table II presents the findings regarding perception related to the skin and avoidance experience in subjects with and without a lifetime diagnosis of psoriasis. An association between psoriasis and dry skin, with an OR 1.99 (95% CI 1.64–2.41) was observed, indicating that individuals with psoriasis were nearly twice as likely to experience dry skin compared with controls. Similarly, the perception of sensitive skin was more prevalent in the psoriasis group (49.4%) than in the non-psoriasis group (38.5%), OR 1.65 (95% CI 1.38–1.97), indicating that individuals with psoriasis had a 65% higher likelihood of reporting sensitive skin. Regarding avoidance behaviour, individuals with psoriasis showed higher rates of avoiding leave-on products (49.8%), rinse-off products (30.3%), household products (26.9%), and other products (33.7%) compared with individuals without psoriasis. All these avoidance behaviours exhibited statistically significant associations with psoriasis (p < 0.001) with ORs ranging from 1.47 to 1.62. Also, avoidance of topical medications at any time was significantly more common in individuals with psoriasis (9.2%) than in those without psoriasis (5.0%). Fig. 1 depicts the avoidance of products among subjects with and without a lifetime diagnosis of psoriasis. No consistent association between psoriasis severity and the factors investigated was documented, the only variables showing an association with severity being avoidance of household products (Table SII).
| Univariate analysis | Multivariable analysis | ||||||
| No psoriasis | With psoriasis | p** | OR (95% CI)^ | p*** | |||
| N* | % | N* | % | ||||
| Dry skin | 5,435 | 51.6 | 414 | 71.1 | < 0.001 | 1.99 (1.64–2.41) | < 0.001 |
| Sensitive skin | 4,054 | 38.5 | 288 | 49.4 | < 0.001 | 1.65 (1.38–1.97) | < 0.001 |
| Avoidance of metals | 3,107 | 29.0 | 208 | 35.3 | 0.001 | 1.20 (0.99–1.46) | 0.06 |
| Avoidance of rubbers | 688 | 6.4 | 52 | 8.8 | 0.02 | 1.29 (0.95–1.75) | 0.10 |
| Avoidance of leave-on products | 3,780 | 35.3 | 294 | 49.8 | < 0.001 | 1.47 (1.23–1.77) | < 0.001 |
| Avoidance of rinse-off products | 2,156 | 20.1 | 179 | 30.3 | < 0.001 | 1.48 (1.22–1.79) | < 0.001 |
| Avoidance of household products | 1,812 | 16.9 | 159 | 26.9 | < 0.001 | 1.62 (1.33–1.98) | < 0.001 |
| Avoidance of other products° | 2,360 | 22.1 | 199 | 33.7 | < 0.001 | 1.43 (1.19–1.73) | < 0.001 |
| Avoidance of topical medications | 537 | 5.0 | 54 | 9.2 | < 0.001 | 1.62 (1.19–2.19) | < 0.001 |
| 95% CI: 95% confidence interval; OR: odds ratio. | |||||||
| *Numbers may not add up to the total due to missing data. **Pearson’s χ2 test. ***Multivariable logistic regression analysis including terms for sex, age, occupation, marital status, smoking habits, body mass index (BMI) and country of residence. | |||||||
| ^Odds ratio (OR) comparing yes vs no. °Including bandages or tape, leather products, henna or permanent tattoos, hair colourants. | |||||||
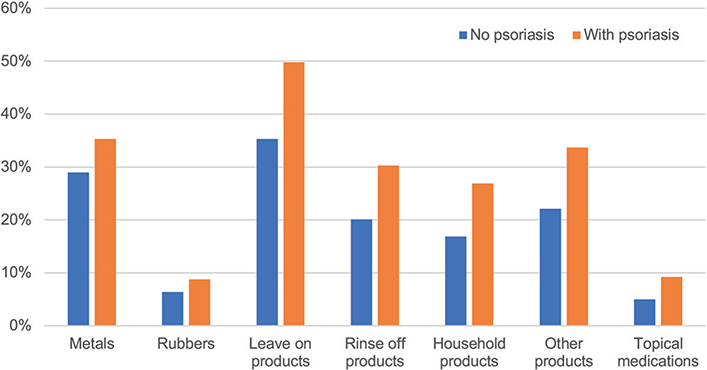
Fig. 1. Avoidance of products among subjects with and without a lifetime diagnosis of psoriasis.
Use of medications, history of allergy tests and results of patch-testing
As shown in Table III, the use of anti-inflammatories, antibiotics and analgesics showed no significant difference between subjects with and without a lifetime diagnosis of psoriasis. The use of topical steroids in the past year was significantly more prevalent in the psoriasis group (40.3%) compared with the non-psoriasis group (14.9%) (p < 0.001), with a substantial OR of 3.13.
| Univariate analysis | Multivariable analysis | ||||||
| No psoriasis | With psoriasis | p** | OR (95% CI)^ | p*** | |||
| N* | % | N* | % | ||||
| Anti-inflammatory drugs used in past year? | 3,294 | 31.2 | 195 | 33.5 | 0.24 | 1.07 (0.89–1.28) | 0.48 |
| Analgesics used in past year? | 3,713 | 35.1 | 233 | 40.0 | 0.02 | 1.02 (0.85–1.23) | 0.81 |
| Antibiotics used in past year? | 958 | 9.1 | 49 | 8.6 | 0.65 | 1.06 (0.77–1.45) | 0.73 |
| Topical steroids used in past year? | 1,568 | 14.9 | 231 | 40.3 | < 0.001 | 3.13 (2.60–3.76) | < 0.001 |
| Topical anaesthetics used in past year? | 734 | 7.7 | 33 | 6.7 | 0.39 | 0.93 (0.63–1.35) | 0.69 |
| Prick tests performed in lifetime? | 2,879 | 27.4 | 211 | 37.2 | < 0.001 | 1.14 (0.94–1.38) | 0.17 |
| Patch tests performed in lifetime? | 1,088 | 10.5 | 121 | 21.1 | < 0.001 | 1.60 (1.28–2.00) | < 0.001 |
| Allergy testing performed in lifetime? | 730 | 7.2 | 65 | 12.0 | < 0.001 | 1.56 (1.18–2.06) | 0.002 |
| 95% CI: 95% confidence interval; OR: odds ratio. | |||||||
| *Numbers may not add up to the total due to missing data. **Pearson’s χ2 test. ***Multivariable logistic regression analysis including terms for sex, age, occupation, marital status, smoking habits, body mass index (BMI) and country of residence. | |||||||
| ^OR comparing yes vs no. | |||||||
Individuals with psoriasis were more likely to have undergone patch-tests (21.1%) and other allergy tests (12.0%) in their lifetime compared with those without psoriasis (10.5% and 7.2%, respectively). Both patch-tests and other allergy tests showed statistically significant associations with psoriasis (p < 0.001), with ORs of 1.60 and 1.56, respectively.
Table IV presents the results of patch-testing in the random sample of subjects selected for performing such a procedure. There was no significant difference in the rates of positive reactions between individuals with psoriasis and those without psoriasis for the tested allergens. No consistent correlation of any of the above-mentioned variables with the severity of psoriasis was shown; the only significant association being antibiotics used in the last year (Table SIII).
| At least 1 positive reaction to: | Univariate analysis | Multivariable analysis | ||||||
| No psoriasis | With psoriasis | p** | OR (95% CI)^ | p*** | ||||
| N = 2,743* | % | N = 163* | % | |||||
| True Test Panel 1 | 507 | 18.5 | 32 | 19.6 | 0.71 | 1.15 (0.75–1.76) | 0.52 | |
| True Test Panel 2 | 246 | 9.0 | 19 | 11.7 | 0.25 | 1.26 (0.74–2.12) | 0.39 | |
| True Test Panel 3 | 23 | 0.8 | 1 | 0.6 | 1 | 0.62 (0.08–4.72) | 0.65 | |
| Single substances of FM I | 73 | 2.7 | 7 | 4.3 | 0.21 | 1.35 (0.56–3.24) | 0.50 | |
| Single substances of FM II | 62 | 2.3 | 5 | 3.1 | 0.42 | 1.02 (0.36–2.91) | 0.97 | |
| EU–Standard series1 | 103 | 4.2 | 6 | 4.1 | 0.98 | 1.04 (0.44–2.46) | 0.94 | |
| Metals2 | 422 | 15.4 | 25 | 15.3 | 0.99 | 1.07 (0.67–1.72) | 0.77 | |
| Preservatives3 | 179 | 6.5 | 9 | 5.5 | 0.61 | 0.69 (0.33–1.46) | 0.34 | |
| Rubbers4 | 37 | 1.3 | 5 | 3.1 | 0.08 | 2.35 (0.87–6.35) | 0.09 | |
| Topical steroids5 | 17 | 0.6 | 1 | 0.6 | 1 | 0.77 (0.10–5.97) | 0.80 | |
| Any tested allergen | 772 | 28.1 | 43 | 26.4 | 0.63 | 0.90 (0.62–1.32) | 0.60 | |
| 1Including new fragrance mix (b+), fragrance mix ii 14% pet, balsam of Peru, sesquiterpenelactone mix 0.1% pet and lyral 5% pet. 2Including nickel sulphate, potassium dichromate and cobalt chloride. 3Including thiomersal, cl+me-isothiazolinone, quaternium 15-, formaldehyde, parabens mix, diazolidinyl urea and imidazolidinyl urea. 4Including carba mix 250, black rubber mix, mercaptobenzothiazole, mercapto mix and thiuram mix. 5Including budesonide, tixocortol-21-pivalate and hydrocortisone-17-butyrate. | ||||||||
| 95% CI: 95% confidence interval; FM: fragrance mix; OR: odds ratio. | ||||||||
| *Numbers may not add up to the total due to missing data. **Pearson’s χ2 test or Fisher’s exact test where required. ***Multivariable logistic regression analysis including terms for sex, age, occupation, marital status, smoking habits, body mass index (BMI) and country of residence. | ||||||||
| ^OR comparing yes vs no. | ||||||||
DISCUSSION
Psoriasis, a complex and chronic inflammatory skin disease, has a significant impact on the physical, emotional, and social well-being of people with the condition (1). This study, using data from the EDEN Fragrance Study, conducted in 6 European regions sheds light on various aspects of psoriasis, revealing valuable information about the subjective experiences, coping behaviours, and allergen reactivity of those living with the condition. One of the most significant and intriguing finding was the higher prevalence of perceived dry and sensitive skin reported by those with psoriasis compared with those without the condition. Remarkably, this perception was independent of the severity of psoriasis, suggesting that factors other than the visible extent of skin lesions may contribute to these feelings (21). The study also revealed the cautious approach taken by people with psoriasis in exposing themselves to products of common use. Patients showed greater vigilance in avoiding specific products and substances than those without psoriasis. Specifically, patients with psoriasis showed a significantly higher tendency to avoid leave-on products, rinse-off products, and household products. Despite a significant association between psoriasis and the use of topical steroids in the past year, a greater percentage of patients with psoriasis (9.2%) compared with those without psoriasis (5.0%) reported having avoided some topical medications in their past history. This behaviour of avoiding topical medications may suggest a degree of non-adherence to topical medications. Psoriasis is a chronic condition that requires consistent and regular use of topical medications. Such a regular use may be difficult to follow on a long-term basis (22–26). In general, the avoidance behaviour might be a consequence of the perceived heightened sensitivity and dryness of the skin experienced by individuals with psoriasis. The higher frequency of allergy tests performed in their lifetime history may be an additional reflection of the concern of people with psoriasis about contact with products of common use (27). Despite these subjective experiences and behaviours, the study found no significant difference in positive reactions to patch-tests between individuals with and without psoriasis. It is possible that the psycho-emotional impact of psoriasis, widely documented in the literature, may influence the perception of skin reaction and sensitivity (28). Also, the release of cytokines and chemokines linked with psoriasis may influence neuro-inflammation and/or an increased excitability of peripheral nerve fibres, resulting in nerve hypersensitivity and alloesthesia not proportional to objective disease severity (29–39). Notably, vulvar pruritus and burning sensation is highly prevalent in women with psoriasis. In most of the cases these symptoms are not correlated with psoriasis severity or with location of the disease in the vulvar area (40).
It should be noted that the current study did not exclude from the control group people with dermatological conditions, such as atopic dermatitis or contact dermatitis. Hence, our estimates may be conservative and the association of psoriasis with skin sensitivity or product avoidance may be even more relevant than documented in this study.
To the best of our knowledge there is a paucity of studies investigating the subjective skin perception and skin reactivity of patients with psoriasis. Therefore, the current study will be a basis for future research and further investigation. In fact, delving into these aspects could be of importance in developing effective treatment strategies tailored to the specific needs of individuals with psoriasis. Considering the multifaceted nature of the condition, a better understanding of the complex interplay of factors contributing to subjective experiences in psoriasis may pave the way for more personalized and effective management approaches, ultimately improving the quality of life of people with the condition.
ACKNOWLEDGEMENTS
This study was partly funded by the Research Institute for Fragrance Materials (RIFM) and L’Oreal.
REFERENCES
- Griffiths CEM, Armstrong AW, Gudjonsson JE, Barker JNWN. Psoriasis. Lancet 2021; 397: 1301–1315.
- Griffiths CE, Iaccarino L, Naldi L, Olivieri I, Pipitone N, Salvarani C, et al. Psoriasis and psoriatic arthritis: immunological aspects and therapeutic guidelines. Clin Exp Rheumatol 2006; 24: S72–S78.
- Coates LC, Soriano ER, Corp N, Bertheussen H, Callis Duffin K, Campanholo CB, et al GRAPPA. Treatment Recommendations domain subcommittees Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA): updated treatment recommendations for psoriatic arthritis. Nat Rev Rheumatol 2021; 18: 465–479.
- Korman NJ. Management of psoriasis as a systemic disease: what is the evidence? Br J Dermatol 2020; 182: 840–848.
- Takeshita J, Grewal S, Langan SM, Mehta NN, Ogdie A, Van Voorhees AS., et al. Psoriasis and comorbid diseases: epidemiology. J Am Acad Dermatol 2017; 76: 377–390.
- Amin, M, Lee, EB, Tsai, TF, Wu, JJ. Psoriasis and co-morbidity. Acta Derm Venereol 2020; 100: adv00033.
- Naldi L, Mercuri SR. Epidemiology of comorbidities in psoriasis. Dermatol Ther 2010; 23: 114–118.
- Kleyn CE, Talbot PS, Mehta NN, Sampogna F, Bundy C, Ashcroft DM, et al. Psoriasis and mental health workshop report: exploring the links between psychosocial factors, psoriasis, neuroinflammation and cardiovascular disease risk. Acta Derm Venereol 2020; 100: adv00020.
- Mattei PL, Corey KC, Kimball AB. Psoriasis Area Severity Index (PASI) and the Dermatology Life Quality Index (DLQI): the correlation between disease severity and psychological burden in patients treated with biological therapies. J Eur Acad Dermatol Venereol 2014; 28: 333–337.
- Boswell ND, Cook MK, Balogh EA, Feldman SR. The impact of complete clearance and almost complete clearance of psoriasis on quality of life: a literature review. Arch Dermatol Res 2023; 315: 699–706.
- Puig L, Thom H, Mollon P, Tian H, Ramakrishna GS. Clear or almost clear skin improves the quality of life in patients with moderate-to-severe psoriasis: a systematic review and meta-analysis. J Eur Acad Dermatol Venereol 2017; 31: 213–220.
- Van Voorhees AS, Fried R. Depression and quality of life in psoriasis. Postgrad Med 2009; 121: 154–161.
- Pithadia DJ, Reynolds KA, Lee EB, Wu JJ. Psoriasis-associated cutaneous pain: etiology, assessment, impact, and management. J Dermatolog Treat 2019; 30: 435–440.
- Ayasse MT, Buddenkotte J, Alam M, Steinhoff M. Role of neuroimmune circuits and pruritus in psoriasis. Exp Dermatol 2020; 29: 414–426.
- Ljosaa TM, Bondevik H, Halvorsen JA, Carr E, Wahl AK. The complex experience of psoriasis related skin pain: a qualitative study. Scand J Pain 2020; 20: 491–498.
- Langan SM, Bouwes Bavinck JN, Coenraads PJ, Diepgen T, Elsner P, Grob JJ, et al, & European Dermato-Epidemiology Network. Update on the activities of the European Dermato-Epidemiology Network (EDEN). Dermatology 2006; 213: 1–2.
- Naldi L, Cazzaniga S, Gonçalo M, Diepgen T, Bruze M, Elsner P, et al, & EDEN Fragrance Study Group. Prevalence of self-reported skin complaints and avoidance of common daily life consumer products in selected European Regions. JAMA Dermatol 2014; 150: 154–163.
- Brown LD, Cai TT, DasGupta A. Interval estimation for a binomial proportion. Stat Sci 2001; 16: 101–133.12.
- European Commission. Europe in figures – Eurostat yearbook 2010. Luxembourg, Publications Office of the European Union; 2010.
- Ahmad OB, Boschi-Pinto C, Lopez AD, Murray CJL, Lozano R, Inoue M. Age standardization of rates: a new WHO standard. Geneva: World Health Organization; 2001.
- Nordbø ECA, Aamodt G, Ihlebæk CM. Subjective health complaints in individuals with psoriasis and psoriatic arthritis: associations with the severity of the skin condition and illness perceptions – a cross-sectional study. Int J Behav Med 2017; 24: 438–446.
- Zschocke I, Mrowietz U, Karakasili E, Reich K. Non-adherence and measures to improve adherence in the topical treatment of psoriasis. J Eur Acad Dermatol Venereol 2014; 28: 4–9.
- Choi JW, Kim BR, Youn SW. Adherence to topical therapies for the treatment of psoriasis: surveys of physicians and patients. Ann Dermatol 2017; 29: 559–564.
- Devaux S, Castela A, Archier E, Gallini A, Joly P, Misery L, et al. Adherence to topical treatment in psoriasis: a systematic literature review. J Eur Acad Dermatol Venereol 2012; 26: 61–67.
- Chat VS, Kearns DG, Uppal SK, Han G, Wu JJ. Management of psoriasis with topicals: applying the 2020 AAD-NPF guidelines of care to clinical practice. Cutis 2022; 110: 8–14.
- Ninosu N, Hoelker S, Kappenstein M, Buettner S, Peitsch WK, Schaarschmidt ML. Treatment satisfaction of patients with psoriasis with topical therapy in a real-world setting: unmet need for higher effectiveness. J Dermatol Treat 2023; 34: 2200570.
- Malhotra V, Kaur I, Saraswat A, Kumar B. Frequency of patch-test positivity in patients with psoriasis: a prospective controlled study. Acta Derm Venereol 2002; 82: 432–435.
- Misery L, Loser K, Ständer S. Sensitive skin. J Eur Acad Dermatol Venereol 2016; 30: 2–8.
- Singh R, Koppu S, Perche PO, Feldman SR. The cytokine mediated molecular pathophysiology of psoriasis and its clinical implications. Int J Mol Sci 2021; 22: 12793.
- Holman DM, Kalaaji AN. Cytokines in dermatology. J Drugs Dermatol 2006; 5: 520–524.
- de Alcantara CC, Reiche EMV, Simão ANC. Cytokines in psoriasis. Adv Clin Chem 2021; 100: 171–204.
- Iznardo H, Puig L. The interleukin-1 family cytokines in psoriasis: pathogenetic role and therapeutic perspectives. Expert Rev Clin Immunol 2021; 17: 187–199.
- Peters EM, Liezmann C, Klapp BF, Kruse J. The neuroimmune connection interferes with tissue regeneration and chronic inflammatory disease in the skin. Ann N Y Acad Sci 2012; 1262: 118–126.
- Ruppenstein A, Limberg MM, Loser K, Kremer AE, Homey B, Raap U. Involvement of neuro-immune interactions in pruritus with special focus on receptor expressions. Front Med (Lausanne) 2021; 8: 627985.
- Shang L, Zhao S, Shi H, Xing X, Zhang J, He Y. Nerve growth factor mediates activation of transient receptor potential vanilloid 1 in neurogenic pruritus of psoriasis. Int Immunopharmacol 2023; 118: 110063.
- Moon HS, Mizara A, McBride SR. Psoriasis and psycho-dermatology. Dermatol Ther (Heidelb) 2013; 3: 117–130.
- Martins AM, Ascenso A, Ribeiro HM, Marto J. The brain-skin connection and the pathogenesis of psoriasis: a review with a focus on the serotonergic system. Cells 2020; 9: 796.
- Galimova E, Rätsep R, Traks T, Chernov A, Gaysina D, Kingo K, et al. Polymorphisms in corticotrophin-releasing hormone-proopiomalanocortin (CRH-POMC) system genes: Neuroimmune contributions to psoriasis disease. J Eur Acad Dermatol Venereol 2023; 37: 2028–2040.
- Amalia SN, Baral H, Fujiwara C, Uchiyama A, Inoue Y, Yamazaki S, et al. TRPV4 regulates the development of psoriasis by controlling adenosine triphosphate expression in keratinocytes and the neuroimmune system. J Invest Dermatol 2023; 143: 2356–2365.e5.
- Zamirska A, Reich A, Berny-Moreno J, Salomon J, Szepietowski JC. Vulvar pruritus and burning sensation in women with psoriasis. Acta Derm Venereol 2008; 88: 132–135.